REVIEW PAPER
Cotard’s syndrome – review of current knowledge
1
Klinika Psychiatrii i Rehabilitacji Psychiatrycznej, Studenckie Koło Naukowe Kliniki Psychiatrii i Rehabilitacji Psychiatrycznej, Lublin, Polska
Corresponding author
Lena Maria Kreczyńska
Lena Maria Kreczyńska, Klinika Psychiatrii i Rehabilitacji Psychiatrycznej, Studenckie Koło Naukowe Kliniki Psychiatrii i Rehabilitacji Psychiatrycznej, Lublin, Polska
Lena Maria Kreczyńska, Klinika Psychiatrii i Rehabilitacji Psychiatrycznej, Studenckie Koło Naukowe Kliniki Psychiatrii i Rehabilitacji Psychiatrycznej, Lublin, Polska
Med Og Nauk Zdr. 2024;30(4):289-293
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Cotard’s syndrome is one of the less common psychiatric disorders. It is defined as a syndrome characterized by the presence of nihilistic delusions which, depending on the course of the illness, can focus on beliefs about one’s own death, the non-existence of internal organs, or the process of their decomposition. Sometimes, external elements of the world can also become the objects of delusions.
Review methods:
This article was based on a systematic review of original articles describing case studies of various patients suffering from Cotard’s syndrome, as well as reviews focusing on understanding the specific nature of this disorder and its underlying causes.
Brief description of the state of knowledge:
Considering the rarity of Cotard’s syndrome, it has not been included in any list of medical conditions, including the ICD-10, ICD-11, or DSM-V classification. When diagnosing patients suspected of Cotard’s syndrome attention should be paid to increased feelings of anxiety, sometimes accompanied by a sense of guilt that cannot be explained by rational causes. Over time, nihilistic delusions also appear, with the key aspect being the patient’s denial of reality.
Summary:
Cotard’s syndrome may manifest in patients as an independent disorder or coexist with other medical conditions such as schizophrenia, depression, anxiety disorders, Parkinson’s disease, or stroke. Depending on the underlying cause of symptoms, different therapeutic approaches may be necessary. Recognizing the significance of coordinated collaboration among doctors of various specialties is crucial in diagnosing this extremely rare disorder.
Cotard’s syndrome is one of the less common psychiatric disorders. It is defined as a syndrome characterized by the presence of nihilistic delusions which, depending on the course of the illness, can focus on beliefs about one’s own death, the non-existence of internal organs, or the process of their decomposition. Sometimes, external elements of the world can also become the objects of delusions.
Review methods:
This article was based on a systematic review of original articles describing case studies of various patients suffering from Cotard’s syndrome, as well as reviews focusing on understanding the specific nature of this disorder and its underlying causes.
Brief description of the state of knowledge:
Considering the rarity of Cotard’s syndrome, it has not been included in any list of medical conditions, including the ICD-10, ICD-11, or DSM-V classification. When diagnosing patients suspected of Cotard’s syndrome attention should be paid to increased feelings of anxiety, sometimes accompanied by a sense of guilt that cannot be explained by rational causes. Over time, nihilistic delusions also appear, with the key aspect being the patient’s denial of reality.
Summary:
Cotard’s syndrome may manifest in patients as an independent disorder or coexist with other medical conditions such as schizophrenia, depression, anxiety disorders, Parkinson’s disease, or stroke. Depending on the underlying cause of symptoms, different therapeutic approaches may be necessary. Recognizing the significance of coordinated collaboration among doctors of various specialties is crucial in diagnosing this extremely rare disorder.
REFERENCES (23)
1.
Dihingia S, Bhuyan D, Bora M, et al. Cotard’s Delusion and Its Relation With Different Psychiatric Diagnoses in a Tertiary Care Hospital. Cureus. 2023;15(5):e39477. https://doi.org/10.7759/cureus....
2.
Koreki A, Mashima Y, Oda A, et al. You are already dead: Case report of nihilistic delusions regarding others as one representation of Cotard’s syndrome. PCN Rep. 2023; 2(2):e93. https://doi.org/10.1002/pcn5.9....
3.
Huarcaya-Victoria J, Bojórquez-De la Torre J, De la Cruz-Oré J. Factor structure of Cotard’s syndrome: Systematic review of case reports. Rev Colomb Psiquiatr. 2020;49(3):187–193. https://doi.org/10.1016/j.rcp.....
4.
Cipriani G, Nuti A, Danti S, et al. I am dead: Cotard syndrome and dementia. Int J Psychiatry Clin Pract. 2019;23(2):149–156. https://doi.org/10.1080/136515....
5.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 10th ed. World Health Organization; 2009.
6.
World Health Organization. International Statistical Classification of Diseases and Related Health Problems. 11th ed. World Health Organization; 2018.
7.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders:DSM-5. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
8.
Sahoo A, Josephs KA. A Neuropsychiatric Analysis of the Cotard Delusion. J Neuropsychiatry Clin Neurosci. 2018 Winter; 30(1):58–65. https://doi.org/10.1176/appi.n....
9.
Dieguez S. Cotard Syndrome. Front Neurol Neurosci. 2018;42:23–34. https://doi.org/10.1159/000475....
10.
Machado L, Peregrino A, Azoubel S, et al. Cotard’s syndrome and major depression with psychotic symptoms. Braz J Psychiatry. 2013;35(2):212. https://doi.org/10.1590/1516-4....
11.
Tomasetti C, Valchera A, Fornaro M, et al. The ‘dead man walking’ disorder: an update on Cotard’s syndrome. Int Rev Psychiatry. 2020;32(5–6):500–509. https://doi.org/10.1080/095402....
12.
Leis K, Gapska D, Aleksiewicz T, et al. Cotard’s syndrome – a review. Psychiatria i psychologia kliniczna. 2018;18(3):320–322. doi:10.15557/PiPK.2018.0040.
13.
Moschopoulos NP, Kaprinis S, Nimatoudis J. Psychiatriki. 2016;27(4):296–302. https://doi.org/10.22365/jpsyc....
14.
Enoch DM, Trethowan W. Uncommon Psychiatric Syndromes. 3rd ed. Oxford: Butterworth & Heinemann; 1991. p. 162–183.
15.
Puri BK,Treasaden IH. Psychiatria podręcznik dla studentów. Edra Urban & Partner; 2014.
16.
Machado L, Evandro de Lima Filho L, Machado L. When the Patient Believes That the Organs Are Destroyed: Manifestation of Cotard’s Syndrome. Case Rep Med. 2016;2016:1–3. http://dx.doi.org/10.1155/2016....
17.
Falkowska U, Adamczyk K, Adamczyk D, et al. Uncommon psychopathological syndromes in psychiatry. Current Problems of Psychiatry. 2018;19(4):314. doi:10.2478/cpp-2018-0024.
18.
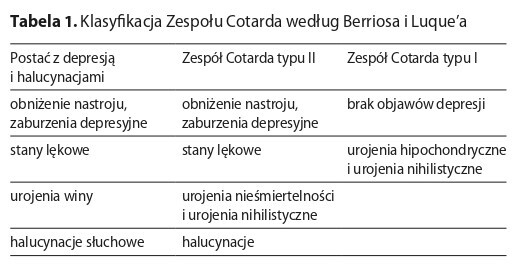
Berrios GE, Luque R. Cotard’s syndrome: analysis of 100 cases. Acta Psychiatr Scand. 1995b;91(3):185–188. https://doi.org/10.1111/j.1600....
19.
Karakuła HK, Romaniuk M, Krupa K, et al. My Body Is Rotting: A case report of Cotard’s syndrome in a postpartum woman. Curr Probl Psychiatry. 2020;21(2):102–108. http://dx.doi.org/10.2478/cpp-....
20.
Lingshuang He, Qingjian Hao, Qiang Wang. Cotard’s Syndrome: A Detailed Description of the Stages. Med Sci Case Rep. 2018;5:27–30. doi:10.12659/MSCR.909512.
21.
Huber CG, Agorastos A. We Are All Zombies Anyway: Aggression in Cotard’s Syndrome. J Neuropsychiatry Clin Neurosci. 2012;24(3):E21. doi:10.1176/appi.neuropsych.11070155.
22.
Revilla J, Aliaga S, Lozano-Vargas A. Cotard and Capgras Syndrome in a Patient with Treatment-Resistant Schizophrenia. Case Rep Psychiatry. 2021:1–3. doi:10.1155/2021/6652336.
23.
Stewart AL, Robinson DM. Cotard’s Syndrome as a Neuropsychiatric Sequela of COVID-19. Journal of the Academy of Consultation-Liaison Psychiatry. 2022;63(2):182–183. doi:10.1016/j.jaclp.2021.09.002.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.