REVIEW PAPER
Prevention of iron deficiency in persons on vegan diet
1
Zakład Towaroznawstwa Żywności, Gdański Uniwersytet Medyczny, Polska
Corresponding author
Patrycja Gogga
Gdański Uniwersytet Medyczny, Zakład Towaroznawstwa Żywności, Dębinki 7, 80-211, Gdańsk, Polska
Gdański Uniwersytet Medyczny, Zakład Towaroznawstwa Żywności, Dębinki 7, 80-211, Gdańsk, Polska
Med Og Nauk Zdr. 2022;28(1):33-39
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Iron is an essential mineral, the reserves of which in people on a plantbased diet are lower than in regular meatconsumers. The aim of the study was to summarize knowledge on factors that inhibit and improve iron absorption and on ways how to properly compose and prepare meals in order to maximize the bioavailibility of this micronutrient.
Review methods:
The article is based on a literature review covering the following issues: iron status of vegans and vegetarians, iron bioavailability, factors reducing and improving iron absorption. The study is mainly based on the results of research involving human subjects. The publications used originate from electronic databases – PubMed and Google Scholar.
Brief description of the state of knowledge:
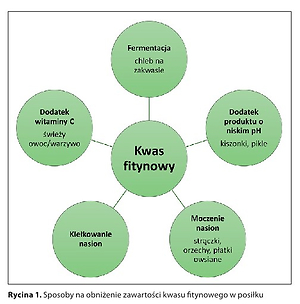
In order to increase the absorption of iron from plant foods, a source of vitamin C should be added to meals, preferably raw vegetables or fruits. Various types of seeds (cereals, nuts, legumes) should be soaked before consumption; one should also consume sprouted seeds and fermented products. It is recommended not to drink with meals, especially tea and coffee, and to eat foods rich in iron and calcium in one meal. It may be helpful to introduce ironfortified products into the diet and appropriate probiotic therapy.
Summary:
People on a properly balanced plant diet, covering the recommended daily intake for iron, are not more likely to develop iron deficiency anaemia than people on a mixed diet. However, in order to meet the need for iron, increased in vegans (especially in women), it is necessary not only to choose products rich in this micronutrient, but also to properly compose and prepare meals.
Iron is an essential mineral, the reserves of which in people on a plantbased diet are lower than in regular meatconsumers. The aim of the study was to summarize knowledge on factors that inhibit and improve iron absorption and on ways how to properly compose and prepare meals in order to maximize the bioavailibility of this micronutrient.
Review methods:
The article is based on a literature review covering the following issues: iron status of vegans and vegetarians, iron bioavailability, factors reducing and improving iron absorption. The study is mainly based on the results of research involving human subjects. The publications used originate from electronic databases – PubMed and Google Scholar.
Brief description of the state of knowledge:
In order to increase the absorption of iron from plant foods, a source of vitamin C should be added to meals, preferably raw vegetables or fruits. Various types of seeds (cereals, nuts, legumes) should be soaked before consumption; one should also consume sprouted seeds and fermented products. It is recommended not to drink with meals, especially tea and coffee, and to eat foods rich in iron and calcium in one meal. It may be helpful to introduce ironfortified products into the diet and appropriate probiotic therapy.
Summary:
People on a properly balanced plant diet, covering the recommended daily intake for iron, are not more likely to develop iron deficiency anaemia than people on a mixed diet. However, in order to meet the need for iron, increased in vegans (especially in women), it is necessary not only to choose products rich in this micronutrient, but also to properly compose and prepare meals.
REFERENCES (52)
1.
Kamiński M, Skonieczna-Żydecka K, Nowak JK, et al. Global and local diet popularity rankings, their secular trends, and seasonal variation in Google Trends data. Nutrition. 2020; 79–80: 110759. doi: 10.1016/j.nut.2020.110759.
2.
Roślinnie-jemy. Postawy Polaków wobec produktów roślinnych – raport z badań opinii publicznej. https://roslinniejemy.org/publ... roslinnych-raport-z-badan-opi-nii-publicznej (access: 14.09.2021).
3.
Główny Urząd Statystyczny. Rolnictwo w 2019 r. https://stat.gov.pl/files/gfx/... (access 15.12.2020).
4.
Melina V, Craig W, Levin S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J Acad Nutr Diet. 2016; 116(12): 1970–1980. doi: 10.1016/j.jand.2016.09.025.
5.
Sobiecki JG, Appleby PN, Bradbury KE, et al. High compliance with dietary recommendations in a cohort of meat eaters, fish eaters, vegetarians, and vegans: results from the European Prospective Investigation into Cancer and Nutrition-Oxford study. Nutr Res. 2016; 36(5): 464–77. doi: 10.1016/j.nutres.2015.12.016.
6.
Haider LM, Schwingshackl L, Hoffmann G, et al. The effect of vegetarian diets on iron status in adults: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2018; 58(8): 1359–1374. doi: 10.1080/10408398.2016.1259210.
7.
Jarosz M, Rychlik E, Stoś K, et al. Normy żywienia dla populacji Polski i ich zastosowanie. Narodowy Instytut Zdrowia Publicznego – Państwowy Zakład Higieny; 2020.
8.
Pawlak R, Berger J, Hines I. Iron Status of Vegetarian Adults: A Review of Literature. Am J Lifestyle Med. 2016; 12(6): 486–498. doi: 10.1177/1559827616682933.
9.
Dasa F, Abera T. Factors Affecting Iron Absorption and Mitigation Mechanisms: A review. Int J Agric Sc Food Technol. 2018; 4(1): 024–030. doi: http://dx.doi.org/10.17352/ija....
10.
Wallace DF. The Regulation of Iron Absorption and Homeostasis. Clin Biochem Rev. 2016; 37(2): 51–62.
11.
Langer AL, Ginzburg YZ. Role of hepcidin-ferroportin axis in the pathophysiology, diagnosis, and treatment of anemia of chronic inflammation. Hemodial Int. 2017; 21 Suppl 1(Suppl 1): S37-S46. doi: 10.1111/hdi.12543.
12.
Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014; 19(2): 164–74.
13.
Barragán-Ibanez G, Santoyo-Sánchez A, Ramos-Penafiel C. Iron deficiency anaemia. Rev Med Hosp Gen Mex. 2015; 79(2): 88–97. doi: 10.1016/j.hgmx.2015.06.008.
14.
Bresgen N, Eckl PM. Oxidative stress and the homeodynamics of iron metabolism. Biomolecules. 2015; 5(2): 808–847. doi: 10.3390/biom5020808.
15.
Wessling-Resnick M. Excess iron: considerations related to development and early growth. Am J Clin Nutr. 2017; 106(Suppl 6): 1600S-1605S. doi: 10.3945/ajcn.117.155879.
16.
Yiannikourides A, Latunde-Dada GO. A Short Review of Iron Metabolism and Pathophysiology of Iron Disorders. Medicines (Basel). 2019; 6(3): 85. doi: 10.3390/medicines6030085.
17.
Śliwińska A, Luty J, Aleksandrowicz-Wrona E, et al. Iron status and dietary iron intake in vegetarians. Adv Clin Exp Med. 2018; 27(10): 1383–1389. doi: 10.17219/acem/70527.
18.
Gupta RK, Gangoliya SS, Singh NK. Reduction of phytic acid and enhancement of bioavailable micronutrients in food grains. J Food Sci Technol. 2015; 52(2): 676–684. doi: 10.1007/s13197-013-0978-y.
19.
Hurrell RF, Reddy MB, Juillerat MA, et al. Degradation of phytic acid in cereal porridges improves iron absorption by human subjects. Am J Clin Nutr. 2003; 77(5): 1213–1219. doi: 10.1093/ajcn/77.5.1213.
20.
Lesjak M, KS Srai S. Role of Dietary Flavonoids in Iron Homeostasis. Pharmaceuticals (Basel). 2019; 12(3): 119. doi: 10.3390/ph12030119.
21.
Khodaii Z, Zadeh MN, Kamali J, et al. Enhanced iron absorption from lactic acid fermented bread (an in vivo/ex vivo study). Gene Rep. 2019; 15: 100389. doi.org/10.1016/j.genrep.2019.100389.
22.
Sharma N, Angural S, Rana M, et al. Phytase producing lactic acid bacteria: Cell factories for enhancing micronutrient bioavailability of phytate rich foods. Trends Food Sci Tech. 2020; 96: 1–12. doi: 10.1016/j.tifs.2019.12.001.
23.
Song HY, Sheikha AFEL, Hu DM. The positive impacts of microbial phytase on its nutritional applications. Trends Food Sci Tech. 2019; 86(4): 553–562. doi: 10.1016/j.tifs.2018.12.001.
24.
Scheers N, Rossander-Hulthen L, Torsdottir I, et al. Increased iron bioavailability from lactic-fermented vegetables is likely an effect ofpromoting the formation of ferric iron (Fe(3+)). Eur J Nutr. 2016; 55(1): 373–382. doi: 10.1007/s00394-015-0857-6.
25.
Hurrell R, Egli I. Iron bioavailability and dietary reference values. Am J Clin Nutr. 2010; 91(5): 1461S-1467S. doi: 10.3945/ajcn.2010.28674F.
26.
Shubham K, Anukiruthika T, Dutta S, et al. Iron deficiency anemia: A comprehensive review on iron absorption, bioavailability and emerging food fortification approaches Trends Food Sci Tech. 2020; 99: 58–75. https://doi.org/10.1016/j.tifs....
27.
Gaitán D, Flores S, Saavedra P, et al. Calcium does not inhibit the absorption of 5 milligrams of nonheme or heme iron at doses less than 800 milligrams in nonpregnant women. J Nutr. 2011; 141(9): 1652–6. doi: 10.3945/jn.111.138651.
28.
Benkhedda K, L'abbé MR, Cockell KA. Effect of calcium on iron absorption in women with marginal iron status. Br J Nutr. 2010; 103(5): 742–748. doi: 10.1017/S0007114509992418.
29.
Lönnerdal B. Calcium and iron absorption--mechanisms and public health relevance. Int J Vitam Nutr Res. 2010; 80(4–5): 293–299. doi: 10.1024/0300-9831/a000036.
30.
Omotayo MO, Dickin KL, O'Brien KO, et al. Calcium Supplementation to Prevent Preeclampsia: Translating Guidelines into Practice in Low-Income Countries. Adv Nutr. 2016; 7(2): 275–278. doi: 10.3945/an.115.010736.
31.
Morck TA, Lynch SR, Cook JD. Inhibition of food iron absorption by coffee. Am J Clin Nutr. 1983 Mar; 37(3): 416–20. doi: 10.1093/ajcn/37.3.416.
32.
Lazrak M, El Kari K, Stoffel NU, et al. Tea Consumption Reduces Iron Bioavailability from NaFeEDTA in Nonanemic Women and Women with Iron Deficiency Anemia: Stable Iron Isotope Studies in Morocco. J Nutr. 2021; 151(9): 2714–2720. doi: 10.1093/jn/nxab159.
33.
Sung ES, Choi CK, Kim NR, et al. Association of Coffee and Tea with Ferritin: Data from the Korean National Health and Nutrition Examination Survey (IV and V). Chonnam Med J. 2018; 54(3): 178–183. doi: 10.4068/cmj.2018.54.3.178.
34.
Milman NT. A Review of Nutrients and Compounds, Which Promote or Inhibit Intestinal Iron Absorption: Making a Platform for Dietary Measures That Can Reduce Iron Uptake in Patients with Genetic Haemochromatosis. J Nutr Metab. 2020; 2020: 7373498. doi: 10.1155/2020/7373498.
35.
Hurrell RF, Reddy M, Cook JD. Inhibition of non-haem iron absorption in man by polyphenolic-containing beverages. Br J Nutr. 1999; 81(4): 289–295.
36.
Yang J, Jensine J, Dwyer J, et al. Polyphenols in Foods, Nutr. 2016; 51(6): 290–300. doi: 10.1097/NT.0000000000000183.
37.
Brune M, Rossander L, Hallberg L. Iron absorption and phenolic compounds: importance of different phenolic structures. Eur J Clin Nutr. 1989; 43(8): 547–557.
38.
Ahmad Fuzi SF, Koller D, Bruggraber S, et al. A 1-h time interval between a meal containing iron and consumption of tea attenuates the inhibitory effects on iron absorption: a controlled trial in a cohort of healthy UK women using a stable iron isotope. Am J Clin Nutr. 2017; 106(6): 1413–1421. doi: 10.3945/ajcn.117.161364.
39.
Siegenberg D, Baynes RD, Bothwell TH, et al. Ascorbic acid prevents the dose-dependent inhibitory effects of polyphenols and phytates on nonheme-iron absorption. Am J Clin Nutr. 1991; 53(2): 537–541. doi: 10.1093/ajcn/53.2.537.
40.
Hurrell RF, Reddy MB, Juillerat MA, et al. Degradation of phytic acid in cereal porridges improves iron absorption by human subjects. Am J Clin Nutr. 2003; 77(5): 1213–121.
41.
Phillips KM, Council-Troche M, McGinty RC, et al. Stability of vitamin C in fruit and vegetable homogenates stored at different temperatures. J Food Compost Anal. 2016; 45: 147–162. doi: 10.1016/j.jfca.2015.09.008.
42.
Lee S, Choi Y, Jeong HS, et al. Effect of different cooking methods on the content of vitamins and true retention in selected vegetables. Food Sci Biotechnol. 2017; 27(2): 333–342. doi: 10.1007/s10068-017-0281-1.
43.
Murray-Kolb LE, Welch R, Theil EC, et al. Women with low iron stores absorb iron from soybeans. Am J Clin Nutr. 2003; 77(1): 180–184. doi: 10.1093/ajcn/77.1.180.
44.
Lönnerdal B. Soybean ferritin: implications for iron status of vegetarians. Am J Clin Nutr. 2009; 89(5): 1680S-1685S. doi: 10.3945/ajcn.2009.26736W.
45.
Prentice AM, Mendoza YA, Pereira D, et al. Dietary strategies for improving iron status: balancing safety and efficacy. Nutr Rev. 2017; 75(1): 49–60. doi: 10.1093/nutrit/nuw055.
46.
Jahan TA, Vandenberg A, Glahn RP, et al. Iron Fortification and Bioavailability of Chickpea (Cicer arietinum L.) Seeds and Flour. Nutrients. 2019; 11(9): 2240. doi: 10.3390/nu11092240.
47.
Blanco-Rojo R, Vaquero MP. Iron bioavailability from food fortification to precision nutrition. A review. Innov Food Sci Emerg Technol. 2018 Apr (51). doi: 10.1016/j.ifset.2018.04.015.
48.
Żuk E, Skrypnik K, Suliburska J. Analiza wybranych grup produktów spożywczych wzbogaconych w żelazo. Forum Zaburzeń Metabolicznych. 2018; 9(3): 103–111.
49.
Gera T, Sachdev HS, Boy E. Effect of iron-fortified foods on hematologic and biological outcomes: systematic review of randomized controlled trials. Am J Clin Nutr. 2012; 96(2): 309–324. doi: 10.3945/ajcn.111.031500.
50.
Vonderheid SC, Tussing-Humphreys L, Park C, et al. A Systematic Review and Meta-Analysis on the Effects of Probiotic Species on Iron Absorption and Iron Status. Nutrients. 2019; 11(12): 2938. doi: 10.3390/nu11122938.
51.
Hoppe M, Önning G, Hulthén L. Freeze-dried Lactobacillus plantarum 299v increases iron absorption in young females-Double isotope sequential single-blind studies in menstruating women. PLoS One. 2017; 12(12): e0189141. doi: 10.1371/journal.pone.0189141.
52.
Hoppe M, Önning G, Berggren A, et al. Probiotic strain Lactobacillus plantarum 299v increases iron absorption from an iron-supplemented fruit drink: a double-isotope cross-over single-blind study in women of reproductive age. Br J Nutr. 2015; 114(8): 1195–1202. doi: 10.1017/S000711451500241X.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.