RESEARCH PAPER
Impact of Covid-19 pandemic in Poland on emergency medical teams interventions for patients reporting pain
1
Wydział Nauk Medycznych i Nauk o Zdrowiu, Państwowa Uczelnia Zawodowa im. prof. S. Tarnowskiego w Tarnobrzegu, Polska
2
Wydział Nauk o Zdrowiu i Nauk Społecznych, Państwowa Akademia Nauk Stosowanych im. I. Mościckiego w Ciechanowie, Polska
3
Zakład Medycyny Ratunkowej dla Dzieci, II Katedra Pediatrii, Uniwersytet Medyczny w Łodzi, Polska
Corresponding author
Leszek Marzec
Wydział Nauk Medycznych i Nauk o Zdrowiu, Państwowa Uczelnia Zawodowa im. prof. S. Tarnowskiego w Tarnobrzegu, H. Sienkiewicza 50, 39-400 Tarnobrzeg, Polska
Wydział Nauk Medycznych i Nauk o Zdrowiu, Państwowa Uczelnia Zawodowa im. prof. S. Tarnowskiego w Tarnobrzegu, H. Sienkiewicza 50, 39-400 Tarnobrzeg, Polska
Med Og Nauk Zdr. 2024;30(3):227-231
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The Covid-19 pandemic limited patients' access to medical services and might have affected decisions regarding calls for emergency medical teams (EMT) due to pain. The aim of the study was analysis of EMT interventions due to pain during the selected period of the pandemic.
Material and methods:
EMT interventions during the period from 1 March- 31 December 2020 were analyzed in terms of the cause of pain, taking into account seasonality and territorial distribution. The results were compared with data from before the pandemic i.e. concerning the same period in 2019.
Results:
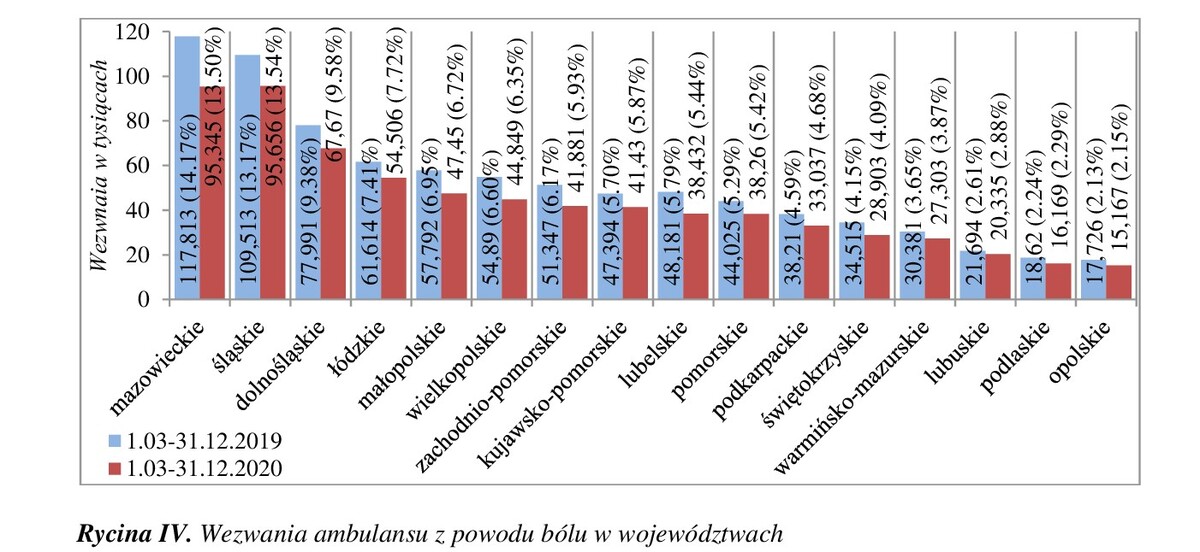
Analyzed calls accounted for 28% of the total 2,483,280 interventions in 2020 and 30% of the total 2,777,291 in 2019. Compared to 2019, a decrease was observed in the number of calls for post-traumatic pain, headache, spine/ back pain and extremities. In turn, an increase was noted in the number of calls for abdominal pain, chest pain, pain in other location, burns and bites/stings. Most calls were for post-traumatic pain (37%-39%), chest pain (25%-27%) and abdominal pain (22%-23%). The percentage of calls was the highest in August 2020 (11%), and in June 2019 (10%), in the Warsaw Province – 13% (14% in 2019), whereas the smallest number of calls were observed in April 2020 (8%), in November 2019 (9%), and in the Opole Province (2%).
Conclusions:
1) Regardless of the Covid-19 pandemic, calls due to pain at various sites account for about one-third of all emergency medical teams interventions. 2) The number of emergency medical teams interventions during the initial period of the Covid-19 pandemic and during the period of the highest number of cases decreased in each province. 3) The most common causes of calls were trauma-induced pain, chest pain, and abdominal pain.
The Covid-19 pandemic limited patients' access to medical services and might have affected decisions regarding calls for emergency medical teams (EMT) due to pain. The aim of the study was analysis of EMT interventions due to pain during the selected period of the pandemic.
Material and methods:
EMT interventions during the period from 1 March- 31 December 2020 were analyzed in terms of the cause of pain, taking into account seasonality and territorial distribution. The results were compared with data from before the pandemic i.e. concerning the same period in 2019.
Results:
Analyzed calls accounted for 28% of the total 2,483,280 interventions in 2020 and 30% of the total 2,777,291 in 2019. Compared to 2019, a decrease was observed in the number of calls for post-traumatic pain, headache, spine/ back pain and extremities. In turn, an increase was noted in the number of calls for abdominal pain, chest pain, pain in other location, burns and bites/stings. Most calls were for post-traumatic pain (37%-39%), chest pain (25%-27%) and abdominal pain (22%-23%). The percentage of calls was the highest in August 2020 (11%), and in June 2019 (10%), in the Warsaw Province – 13% (14% in 2019), whereas the smallest number of calls were observed in April 2020 (8%), in November 2019 (9%), and in the Opole Province (2%).
Conclusions:
1) Regardless of the Covid-19 pandemic, calls due to pain at various sites account for about one-third of all emergency medical teams interventions. 2) The number of emergency medical teams interventions during the initial period of the Covid-19 pandemic and during the period of the highest number of cases decreased in each province. 3) The most common causes of calls were trauma-induced pain, chest pain, and abdominal pain.
REFERENCES (26)
1.
Loeser JD, Treede RG. The Kyodo protocol of ISAP Basic Pain Terminology. Pain. 2008;137(3):473–744. https://doi:10.1016/j.pain.200....
2.
Kocot-Kępska M, Dobrogowski J. Rodzaje bólu. www.mp.pl/bol/wytyczne/94188,rodzaje-bolu (access: 12.09.2022).
3.
Møller TP, Ersbøll AK, Tolstrup JS, et al. Why and when citizens call for emergency help: an observational study of 211,193 medical emergency calls. Scand J Trauma Resusc Emerg Med. 2015;23:88. https://doi:10.1186/s13049-015....
4.
Søvsø MB, Kløjgaard TA, Hansen PA, et al. Repeated ambulance use is associated with chronic diseases – a population-based historic cohort study of patient’s symptoms and diagnoses. Scand J Trauma Resusc Emerg Med. 2019;27(1):46. https://doi.org/10.1186/s13049....
5.
National Emergency Medical Services Information System NEMSIS 2019 Data report. https://nemsis.org/wp-content/.... (access: 22.07.2023).
6.
National Emergency Medical Services Information System NEMSIS 2020 Data report. https://nemsis.org/wp-content/.... (access: 22.07.2023).
7.
Gardocka-Jałowiec A, Śleszyńska-Świderska A, Szalonka K, et al. Wpływ SARS-CoV-2 na konsumpcję leków OTC w Polsce. Zdrowie i style życia. Determinanty długości życia. Wrocław: Uniwersytet wrocławski; 2020. p. 175–194. https://doi:10.34616/23.20.116.
8.
Galani A, Alygizakis N, Aalizadeh R, et al. Patterns of pharmaceutical use during the first wave of Covid-19 pandemic in Athens, Greece as revealed by wastewaster-based epidemiology. STOTEN. 2021;798:149014. https://doi.org/10.1016/j.scit.... (access: 4.08.2023).
9.
Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catherization laboratory activations in the United States during Covid-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. https://doi:10.1016/j.jacc.202....
10.
Metzler B, Siostrzonek P, Binder RK, et al. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852–1853. https://doi.org/10.1093/eurhea....
11.
Grande M, Bjørnsen LP, Naess-Pleym LE, et al. Observational study on chest pain during the Covid-19 pandemic: changes and characteristics of visits to a Norwegian emergency department during the lockdown. BMC Emerg Med. 2022;57. https://doi.org/10.1186/s12873....
12.
Fundacja Centrum Badania Opinii Społecznej. Stosowanie leków dostępnych bez recepty. Warszawa; Oct 2010. https://www.cbos.pl/SPISKOM.PO.... (access: 4.08.2023).
13.
Rozporządzenie Rady Ministrów z dnia 31 marca 2020 r. w sprawie ustanowienia określonych ograniczeń, nakazów i zakazów w związku z wystąpieniem stanu epidemii. (DzU Poz. 566). https://isap.sejm.gov.pl/isap..... (access: 9.08. 2023).
14.
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. https://doi:10.1056/NEJMoa2001....
15.
Zdrowie i ochrona zdrowia w 2020 r. Główny Urząd Statystyczny, Warszawa, Kraków; 2021. p. 108. https://stat.gov.pl/obszary-te.... (access: 7.04.2023).
16.
Legutko J, Niewiara Ł, Bartuś S, et al. The decline of coronary angiography and percutaneous coronary intervention procedures in patients with acute myocardial infarction in Poland during the COVID-19 pandemic. Kardiol Pol. 2020;27(6):574–576. https://doi:10.33963/KP.15393.
17.
De Filippo O, D’Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med. 2020;383(1):88–89. https://doi:10.1056/NEJMc20091....
18.
Aung S, Vittinghoff E, Nah G, et al. Emergency activations for chest pain and ventricular arrhythmias related to regional Covid-19 across the US. Sci Rep. 2021;11(1):23959. https://doi:10.1038/s41598-012....
19.
Dherange P, Lang J, Qian P, et al. Arrhythmias and COVID-19: A review. JACC Clin. Electrophysiol. 2020;6(9):1193–1204. https://doi:10.1016/j.jacep.20....
20.
Larsson G, Hansson P, Olsson E, et al. Prehospital assessment of patients with abdominal pain triaged to self-care at home: an observation study. BMC Emerg Med. 2022;22. https://doi:10.1186/s12873-022....
21.
Gotkowska J. Szwedzkie lekcje z pandemii. Ośrodek Studiów Wschodnich. https://www.osw.waw.pl/pl/publ.... (access: 8.08.2023).
22.
Problemy pacjentów w obliczu epidemii choroby COVID-19. Raport opracowany na podstawie sygnałów kierowanych do Rzecznika Praw Pacjenta od stycznia do września 2020 roku. Rzecznik Praw Pacjenta, Warszawa, październik 2020. https://www.gov.pl/web/rpp/pro.... (access: 26.04.2022).
23.
Caputo EL, Ferreira PH, Feter N, et al. Short-term impact of Covid-19 pandemic on low back pain: data from the PAMPA Cohort, Brazil. BMC Public Health. 2023;44. https://doi.org/10.1186/s12889....
24.
Nowa normalność. Etapy znoszenia ograniczeń związanych z Covid-19. Ministerstwo Zdrowia. https://www.gov.pl/web/koronaw.... (access: 11.08.2023).
25.
Czarkowski MP, Staszewska-Jakubik E, Wielgosz U. Choroby zakaźne i zatrucia w Polsce w 2021 roku. Narodowy Instytut Zdrowia Publicznego – Państwowy Instytut Badawczy Zakład Epidemiologii Chorób Zakaźnych i Nadzoru, Warszawa; 2022. p. 128. http://wwwold.pzh.gov.pl/oldpa.... (access: 11.08.2023).
26.
Podstawowe informacje o przebiegu zjawisk demograficznych w 2020 r. In: Ludność. Stan i struktura oraz ruch naturalny w przekroju terytorialnym w 2020 r. Stan w dniu 31 XII. Warszawa: Główny Urząd Statystyczny; kwiecień 2021. p. 15. https://stat.gov.pl/obszary-te.... (access: 29.09.2022).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.