REVIEW PAPER
Effect of environmental factors on occurrence of male infertility
1
Koło Naukowe przy Katedrze Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska
2
Katedra Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska
Corresponding author
Monika Rusin
Katedra Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska
Katedra Zdrowia Środowiskowego, Wydział Nauk o Zdrowiu w Bytomiu, Śląski Uniwersytet Medyczny w Katowicach, Polska
Med Og Nauk Zdr. 2021;27(2):126-133
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Infertility is the inability of a sexually active couple to achieve pregnancy within one year of regular intercourse without the use of contraception. At present, this problem concerns approximately 10–20% of couples. Among the causes of male infertility are distinguished pre-testicular, testicular and extra-testicular factors.
Objective:
The aim of the study was to review the available literature data concerning the effect of individual, selected environmental factors on the phenomenon of infertility in the male population.
Brief description of the state of knowledge:
Many studies confirmed a progressive deterioration of sperm quality in the male population. Among the factors responsible for the occurrence of this phenomenon are heavy metals present in the environment, such as lead, mercury and cadmium, commonly used pesticides, bisphenol A, as well as dioxins and furans, classified as persistent organic pollutants. These substances exert a negative effect on the body's hormonal balance, and also damage Sertoli and Leydig cells, which may result in reduced sperm count and motility. Life style also plays an important role in maintaining male fertility. Unhealthy diet, tobacco smoking and alcohol consumption reduce testosterone levels and damage the genetic material of sperm.
Summary:
Many chemicals can negatively affect male fertility. Efforts should be made to reduce exposure to pollutants in the environment, improve life style, undertake physical activity, and abstain from stimulants
Infertility is the inability of a sexually active couple to achieve pregnancy within one year of regular intercourse without the use of contraception. At present, this problem concerns approximately 10–20% of couples. Among the causes of male infertility are distinguished pre-testicular, testicular and extra-testicular factors.
Objective:
The aim of the study was to review the available literature data concerning the effect of individual, selected environmental factors on the phenomenon of infertility in the male population.
Brief description of the state of knowledge:
Many studies confirmed a progressive deterioration of sperm quality in the male population. Among the factors responsible for the occurrence of this phenomenon are heavy metals present in the environment, such as lead, mercury and cadmium, commonly used pesticides, bisphenol A, as well as dioxins and furans, classified as persistent organic pollutants. These substances exert a negative effect on the body's hormonal balance, and also damage Sertoli and Leydig cells, which may result in reduced sperm count and motility. Life style also plays an important role in maintaining male fertility. Unhealthy diet, tobacco smoking and alcohol consumption reduce testosterone levels and damage the genetic material of sperm.
Summary:
Many chemicals can negatively affect male fertility. Efforts should be made to reduce exposure to pollutants in the environment, improve life style, undertake physical activity, and abstain from stimulants
REFERENCES (93)
1.
Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. The Interna-tional Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary on ART terminology. Hum Reprod. 2009; 24(11): 2683–2687. https://doi.org/10.1093/humrep....
2.
McLaren JF. Infertility Evaluation. Obstet Gynecol Clin North Am. 2012; 39(4): 453–463. https://doi.org/10.1016/j.ogc.....
3.
Bablok L, Dziadecki W, Szymusik I, et al. Patterns of infertility in Po-land – multicenter study. Neuro Endocrinol Lett. 2011; 32(6): 799–804.
4.
Robaina Flores N, Jenaro Rio C, Moreno Rosset C. Couple therapy in infertility. Papeles del Psicólogo. 2008; 29(2): 205–212.
5.
Nagórska M, Bartosiewicz A, Obrzut B, et al. Gender Differences in the Experience of Infertility Concerning Polish Couples: Preliminary Research. Int J Environ Res Public Health. 2019; 16: 2337. https://doi.org/10.3390/ijerph....
7.
Wdowiak A, Bazylewicz A, Dolzhenko MN, et al. Technologie medyczne w diagnostyce męskiej niepłodności. Eur J Med Technol. 2015; 1(6): 7–17. URL:http://www.medical-technologie... (21.09.2020).
8.
Skreczko K. Przyczyny niepłodności w małżeństwie – dramat bezdzietności. Kwart Nauk. 2017; 1(29): 216–226. URL: https://www.stowarzy-szeniefid... (21.09.2020)
9.
Łukaszuk K, Kozioł K, Jakiel G, et al. Diagnostyka i leczenie niepłodnoś-ci – rekomendacje Polskiego Towarzystwa Medycyny Rozrodu i Embrio-logii (PTMRiE) oraz Polskiego Towarzystwa Ginekologów i Położników (PTGP). Ginek Perinat Prakt. 2018; 3(3): 112–118. URL: http://www.ptmrie.org.pl/pliki... %C5%9Bci%20-%20rekomendacje%20PTMRiE%20i%20PTGP%202018.pdf (22.09.2020).
10.
Koperwas M, Głowacka M. Problem niepłodności wśród kobiet i mężczyzn – epidemiologia, czynniki ryzyka i świadomość społeczna. Aspekty Zdrowia i Choroby 2017; 3: 31–49. URL: http://www.wydawnictwo.wsei.eu... (22.09.2020).
11.
Wdowiak A, Sadowska M, Bakalczuk S, et al. Przyczyny niepłodności męskiej. In: Gorzel M, editor. Psychospołeczne aspekty postrzegania zdrowia i urody. Lublin: Wyższa Szkoła Społeczno-Przyrodnicza im. Wincentego Pola w Lublinie; 2016. p. 123–141. URL: http://wydawni-ctwo.wssp.edu.p... (02.12.2020).
12.
Navarro-Casado L, Juncos-Tobarra MA, Cháfer-Rudilla M, et al. Effect of experimental diabetes and STZ on male fertility capacity. Study in rats. J Androl. 2010; 31(6): 584–592. https://doi.org/10.2164/jan-dr....
13.
Wołczyński S, Kuczyński W, Pawelczyk L, et al. Diagnostyka i lecze-nie niepłodności. Ginekol Dypl. 2011; Marzec: 59–88. URL: https://podyplomie.pl/publish/... (22.09.2020).
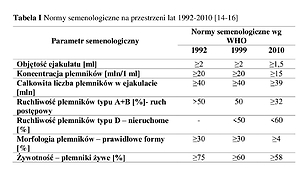
14.
World Health Organization. WHO laboratory manual for the examina-tion and processing of human semen. 5th edition. Genewa: WHO; 2010.
15.
World Health Organization. WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 3rd edition. Cambridge: Cambridge University Press; 1992.
16.
World Health Organization. WHO laboratory manual for the exami-nation of human semen and sperm-cervical mucus interaction. 4th edition. Cambridge: Cambridge University Press; 1999.
17.
Drosdzol-Cop A, Skrzypulec-Plinta V. Niepłodność – postępowanie diagnostyczno-terapeutyczne. Farm Pol. 2011; 67(10): 690–697.
18.
Kołłątaj W, Kołłątaj B, Karwat D, et al. Male infertility and human environmental pollution. J Educ Health Sport. 2017; 7(4): 127–166. http://dx.doi.org/10.5281/zeno....
19.
umar N, Singh AK. Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci. 2015; 8(4): 191–196. https://doi.org/10.4103/0974-1....
20.
Kuladip J, Parimal CS. Environmental Toxicants Induced Male Repro-ductive Disorders: Identification and Mechanism of Action. In: Acree W. Toxicity and Drug Testing. Rijeka: InTech; 2012. p. 473–518. https://doi.org/10.5772/29649.
21.
Ociepa-Kubicka A, Ociepa E. Toksyczne oddziaływanie metali ciężkich na rośliny, zwierzęta i ludzi. Inż Ochr Śr. 2012; 15(2): 169–180. URL: http://yadda.icm.edu.pl/yadda/... (28.09.2020).
22.
Taha E, Sayed S, Ghandour N, et al. Correlation between seminal lead and cadmium and seminal parameters in idiopathic oligoasthenozoo-spermic males. Cent European J Urol. 2013; 66(1): 84–92. https://doi.org/10.5173/ceju.2....
23.
Jastrzębski T, Kowalska A, Szymala I, et al. Narażenie na kadm w okresie pre- i postnatalnym – jego wpływ na płodność i zdrowie dzieci. Med Śr – Environ Med. 2016; 19(3): 58–64. https://doi.org/10.19243/20163....
24.
Olympio KPK, da Rocha Silva JP, da Silva AS, et al. Blood lead and cad-mium levels in preschool children and associated risk factors in São Pau-lo, Brazil Environ Pollut. 2018; 240: 831–838. https://doi.org/10.1016/j.envp....
25.
Socha P, Mojska H, Stoś K, et al. Bezpieczeństwo żywności a potrzeby żywieniowe niemowląt i małych dzieci. „Zdrowe Pokolenia” Stowarzyszenie Promocji Zdrowego Żywienia Dzieci, Warszawa, 2015. URL: http://www.zdrowepokolenia.org... (28.09.2020).
26.
Leon OLL, Pacheco JMS. Effects of Lead on Reproductive Health. Rijeka: InTech; 2019. https://doi.org/10.5772/intech....
27.
Debnath B, Singh WS, Mann K, et al. Sources and Toxicological Effects of Lead on Human Health. Indian J Med Spec. 2019; 10(2): 66. https://doi.org/10.4103/INJMS.....
28.
Pant N, Kumar G, Upadhyay AD, et al. Correlation between lead and cadmium concentration and semen quality. First Int J Androl. 2015; 47(8): 887–891. ht t ps://doi.org /10.1111/a nd.12342.
29.
Sukhn C, Awwad J, Ghantous A, et al. Associations of semen quali-ty with non-essential heavy metals in blood and seminal fluid: data from the Environment and Male Infertility (EMI) study in Lebanon. J Assist Reprod Genet. 2018; 35(9): 1691–1701. https://doi.org/10.1007/s10815....
30.
Claman P. Men at Risk: Occupation and Male Infertility. Sexuality, Re-production and Menopause. 2004; 2(1): 19–26. https://doi.org/10.1016/j.sram....
31.
Rice KM, Walker EM Jr, Wu M, et al. Environmental Mercury and Its Toxic Effects. J Prev Med Public Health. 2014; 47(2): 74–83. https://doi.org/10.3961/jpmph.....
32.
Gworek B, editor. Rtęć w organizmach. Warszawa: Instytut Ochrony Środowiska – Państwowy Instytut Badawczy – Dział Wydawnictw; 2013.
33.
Kot K, Kosik-Bogacka D, Łanocha-Arendarczyk N, et al. Wpływ związków rtęci na organizm człowieka. Farm Współ. 2016; 9: 210–216. URL: https://www.akademiamedycyny.p... (27.09.2020).
34.
Mocevic E, Specht IO, Marott JL, et al. Environmental mercury expo-sure, semen quality and reproductive hormones in Greenlandic Inuit and European men: a cross-sectional study. Asian J Androl. 2013; 15(1): 97–104. https://doi.org/10.1038/aja.20....
35.
Bjørklund G, Chirumbolo S, Dadar M, et al. Mercury exposure and its effects on fertility and pregnancy outcome. Basic Clin Pharmacol Toxicol. 2019; 125(4): 317–327. https://doi.org/10.1111/bcpt.1....
36.
Pasternak-Winiarska A. Wybrane czynniki środowiskowe a ryzyko niepłodności mężczyzn. Kosmos – Probl N Biol. 2019; 68(2): 239–247. https://doi.org/10.36921/kos.2....
37.
Wirth JJ, Mijal RS. Adverse effects of low level heavy metal exposure on male reproductive function. Syst Biol Reprod Med. 2010; 56: 147–167. https://doi.org/10.3109/193963....
38.
Mínguez-Alarcón L, Afeiche MC, Williams PL, et al. Hair mercury (Hg) levels, fish consumption and semen parameters among men attending a fertility center. Int J Hyg Environ Health. 2018; 221(2): 174–182. https://doi.org/10.1016/j.ijhe....
39.
Grotowska M, Janda K, Jakubczyk K. Wpływ pestycydów na zdro-wie człowieka. Pomeranian J Life Sci. 2018; 64(2): 42–50. https://doi.org/10.21164/pomjl....
40.
Carles C, Bouvier G, Lebailly P, et al. Use of job-exposure matrices to estimate occupational exposure to pesticides: A review. J Expo Sci Environ Epidemiol. 2017; 27(2): 125–140. https://doi.org/10.1038/jes.20....
41.
DzU 2009 nr 14 poz. 76. Konwencja Sztokholmska w sprawie trwałych zanieczyszczeń organicznych, sporządzona w Sztokholmie dnia 22 maja 2001 r.
42.
Witczak A, Pohoryło A. Ocena zanieczyszczenia żywności pestycydami fosforoorganicznymi a ryzyko zdrowotne konsumentów. Kosmos. Probl N Biol. 2016; 4: 503–512. URL: http://kosmos.icm.edu.pl/PDF/2... (28.09.2020).
43.
Kowalska G, Kowalski R. Pestycydy – zakres i ryzyko stosowania, korzyści i zagrożenia. Praca przeglądowa. Ann Hort. 2019; 29(2): 5–25. https://doi.org/10.24326/ah.20....
44.
Roszko MŁ, Kamińska M, Szymczyk K, et al. Endocrine disrupting potency of organic pollutant mixtures isolated from commercial fish oil evaluated in yeast-based bioassays. PLoS One. 2018 May; 13(5). https://doi.org/10.1371/journa....
45.
Song Q, Zhanga Y, Yan L, et al. Risk assessment of the endocrine--disrupting effects of nine chiral pesticides. J Hazard Mater. 2017; 338: 57– 65. https://doi.org/10.1016/j.jhaz....
46.
Yang FW, Zhao GP, Rena FZ, et al. Assessment of the endocrine--disrupting effects of diethyl phosphate, a nonspecific metabolite of or-ganophosphorus pesticides, by in vivo and in silico approaches. Environ Int. 2020, Februar y; 135. https://doi.org/10.1016/j.envi....
47.
Perry MJ, Venners SA, Chen X, et al. Organophosphorous pesticide exposures and sperm quality. Reprod Toxicol. 2011; 31(1): 75–79. https://doi.org/10.1016/j.repr....
48.
Lerro CC, Koutros S, Andreotti G, et al. Organophosphate insecticide use and cancer incidence among spouses of pesticide applicators in the Agricultural Health Study. Occup Environ Med. 2015; 72(10): 736–744. https://doi.org/10.1136/oemed-....
49.
Yu D, Liu X, Liu X, et al. Polychlorinated Dibenzo-p-Dioxins, Polychlo-rinated Dibenzofurans, and Dioxin-Like Polychlorinated Biphenyls in Umbilical Cord Serum from Pregnant Women Living Near a Chemical Plant in Tianjin, China. Int J Environ Res Public Health. 2019, June; 16(12). https://doi.org/10.3390/ijerph....
50.
van den Berg M, Denison MS, Birnbaum LS, et al. Polybrominated Dibenzo-p-Dioxins, Dibenzofurans, and Biphenyls: Inclusion in the Toxicity Equivalency Factor Concept for Dioxin-Like Compounds. Toxicol Sci. 2013; 133(2): 197–208. https://doi.org/10.1093/toxsci....
51.
Cieślik I, Migdał W. Dioksyny, furany i polichlorowane bifenyle – toksyczność i występowanie w środowisku. Inż Ochr Śr. 2012; 15(3): 237–247. URL: http://yadda.icm.edu.pl/baztec... (27.09.2020).
52.
World Health Organization. Dioxins and their effects on human health. 2016, Oct. URL: https://www.who.int/news-room/... (24.09.2020).
53.
Całkosiński I, Rosińczuk-Tonderys J, Bazan J, et al. Influence of dioxin intoxication on the human system and possibilities of limiting its negati-ve effects on the environment and living organisms. Ann Agric Environ Med. 2014; 21(3): 518–524. https://doi.org/10.5604/123219....
54.
Lauretta R, Sansone A, Sansone M, et al. Endocrine Disrupting Chemi-cals: Effects on Endocrine Glands. Front Endocrinol (Lausanne). 2019; 10: 178. https://doi.org/10.3389/fendo.....
55.
World Health Organization. Possible developmental early effects of endocrine disrupters on child health. Geneva, 2012.
56.
Słowikowska-Hilczer J, Szarras-Czapnik M, Marchlewska K, et al. Zespół dysgenetycznych jąder: patogeneza i konsekwencje kliniczne. Endokrynol Ped. 2013; 1(42): 67–76. https://doi.org/10.18544/EP-01....
57.
Jambor T, Greifova H, Bistakova J, et al. Endocrine Disruptors and Reproductive Health in Males. Rijeka: InTech; 2018. https://doi.org/10.5772/intech....
58.
Rogala D, Kulik-Kupka K, Spychała A, et al. Bisfenol A – niebezpieczny związek ukryty w tworzywach sztucznych. Probl Hig Epidemiol. 2016; 97(3): 213–219. URL: http://www.phie.pl/pdf/phe-201... (26.09.2020).
59.
Konieczna A, Rutkowska A, Rachoń D. Health risk of exposure to bisphenol A (BPA). Rocz PZH. 2015; 66(1): 5–11. URL: https://pubmed.ncbi.nlm.nih.go... (26.09.2020).
60.
Rubin BS. Bisphenol A: An endocrine disruptor with widespread ex-posure and multiple effects. J Steroid Biochem Mol Biol. 2011; 127(1–2): 27–34. https://doi.org/10.1016/j.jsbm....
61.
Marcoccia D, Pellegrini M, Fiocchetti M, et al. Food components and contaminants as (anti)androgenic molecules. Genes Nutr. 2017; 12(6). https://doi.org/10.1186/s12263....
62.
Rochester JR. Bisphenol A and human health: A review of the lite-rature. Reprod Toxicol. 2013; 42: 132–155. https://doi.org/10.1016/j.repr....
63.
Meeker JD, Ehrlich S, Toth TL, et al. Semen quality and sperm DNA damage in relation to urinary bisphenol A among men from an inferti-lity clinic. Reprod Toxicol, 2010; 30: 532–539. https://doi.org/10.1016/j.repr....
64.
Miao M, Zhou X, Li Y, et al. LINE-1 hypomethylation in spermatozoa is associated with Bisphenol A exposure. Andrology. 2014; 2(1): 138–144. ht t ps://doi.org /10.1111/j.2047-2927.2013.0 0166.x.
65.
Leonardi A, Cofini M, Rigante D, et al. The Effect of Bisphenol A on Puberty: A Critical Review of the Medical Literature. Int J Environ Res Public Health. 2017 Sep; 14(9): 1044. https://doi.org/10.3390/ijer ph14 0910 4 4.
66.
Shen Y, Zheng Y, Jiang J, et al. Higher urinary bisphenol A concentration is associated with unexplained recurrent miscarriage risk: evidence from a case-control study in eastern China. PLoS One. 2015 May 26; 10(5). https://doi.org/10.1371/journa....
67.
Tse LA, Lee PMY, Ho WM, et al. Bisphenol A and other environmental risk factors for prostate cancer in Hong Kong. Environ Int. 2017; 107: 1–7. https://doi.org/10.1016/j.envi....
68.
Jeznach-Steinhagen A, Czerwonogrodzka-Senczyna A. Postępowanie dietetyczne jako element leczenia zaburzeń płodności u mężczyzn z obniżoną jakością nasienia. EOiZPM. 2013; 9(1): 14–19.
69.
World Health Organization. Obesity and overweight. 2020, Apr. URL: https://www.who.int/en/news-ro... (14.12.2020).
70.
Narodowy Fundusz Zdrowia – Departament Analiz i Strategii. Cu-kier, otyłość – konsekwencje. Podsumowanie. 2018. URL: https://zdrowedane.nfz.gov.pl/... (14.12.2020).
71.
Kostecka M, Bojanowska M. Dieta i styl życia jako czynniki wpływające na płodność. Kosmos. Probl N Biol. 2018; 67(2): 425–439. https://doi.org/10.36921/kos.2... _ 2401.
72.
Jensen TK, Andersson AM, Jorgensen N, et al. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril. 2004; 82(4): 863–870. https://doi.org/10.1016/j.fert....
73.
Havrylyuk A, Chopyak V, Nakonechnyyj A, et al. Nowe aspekty nie-płodności partnerskiej: czynnik męski. Postępy Hig Med Dosw. 2015; 69: 1228–1238.
74.
Bebelska KP, Ehmke Vel Emczyńska E, Gmoch-Gajzlerska E. Otyłość jako czynnik zaburzający procesy rozrodcze. Nowiny Lekarskie. 2011; 80(6): 499–507. URL: https://jms.ump.edu.pl/uplo-ad... (14.12.2020).
75.
Kapoor D, Aldred H, Clark S, et al. Clinical and biochemical assessment of hypogonadism in men with type 2 diabetes: correlations with bio-available testosterone and visceral adiposity. Diabetes Care. 2007; 30: 911–917. https://doi.org/10.2337/dc06-1....
76.
Esposito K, Giugliano F, Di PC, et al. Effect of lifestyle changes on erec-tile dysfunction in obese men: a randomized controlled trial. JAMA. 2004; 291: 2978–2984. https://doi.org/10.1001/jama.2....
77.
Rachdaoui N, Sarkar DK. Effects of Alcohol on the Endocrine System. Endocrinol Metab Clin North Am. 2013; 42(3): 593–615. https://doi.org/10.1016/j.ecl.....
78.
Czerwińska A, Pawłowski T. Zaburzenia płodności u mężczyzn uz-leżnionych od alkoholu. Seksuol Pol. 2018; 16(2): 61–66.
79.
Mońka I, Wiechuła D. Znaczenie cynku dla organizmu ludzkiego w aspekcie suplementacji tego pierwiastka. Ann Acad Med Siles. (online) 2017; 71: 314–325. URL: http://psjd.icm.edu.pl/psjd/el... (26.09.2020).
80.
Kothari RP, Chaudhari AR. Zinc Levels in Seminal Fluid in Infer-tile Males and its Relation with Serum Free Testosterone. J Clin Diagn Res. 2016 May; 10(5): CC05–CC08. https://doi.org/10.7860/JCDR/2....
81.
Pendharkar S, Mattoo SK, Grover S. Sexual dysfunctions in alcohol--dependent men: A study from north India. Indian J Med Res. 2016; 144(3): 393–399. https://doi.org/10.4103/0971-5....
82.
Muthusami KR, Chinnaswamy P. Effect of chronic alcoholism on male fertility hormones and semen quality. Fertil Steril. 2005; 84(4): 919–924. https://doi.org/10.1016/j.fert....
83.
Sermondade N, Elloumi H, Berthaut I, et al. Progressive alcohol-induced sperm alterations leading to spermatogenic arrest, which was reversed after alcohol withdrawal. Reprod Biomed Online. 2010; 20(3): 324–327. https://doi.org/10.1016/j.rbmo....
84.
Vu AT, Taylor KM, Holman MR, et al. Polycyclic Aromatic Hydro-carbons in the Mainstream Smoke of Popular U.S. Cigarettes. Chem Res Toxicol. 2015; 28(8): 1616–1626. https://doi.org/10.1021/acs.ch....
85.
World Health Organization. WHO study group on tobacco product regulation. WHO Technical Report Series, 1001. Genewa, 2017.
86.
Główny Inspektorat Sanitarny. Raport z ogólnopolskiego badania ankietowego na temat postaw wobec palenia tytoniu. Warszawa, 2019. URL: https://gis.gov.pl/wp-content/... (02.12.2020).
87.
Ochwanowska E, Stanisławska I, Łyp M, et al. Wpływ dymu tytoniowego na płodność mężczyzn. Med Śr – Environ Med. 2017; 20(2): 46–51.
88.
Ravnborg TL, Jensen TK, Andersson AM, et al. Prenatal and adult exposures to smoking are associated with adverse effects on reproduc-tive hormones, semen quality, final height and body mass index. Hum Reprod. 2011; 26(5): 1000–1011. https://doi.org/10.1093/humrep....
89.
Jurewicz J, Radwan M, Sobala W, et al. Lifestyle and semen quality – role of modifiable risk factors. Syst Biol Reprod Med. 2014; 60(1): 43–51. https://doi.org/10.3109/193963....
90.
Shiva M, Gautam AK, Verma Y, et al. Association between sperm qua-lity, oxidative stress, and seminal antioxidant activity. Clin Biochem. 2011; 44: 319–324. https://doi.org/10.1016/j.clin....
91.
Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, et al. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007; 22(1): 188–196. https://doi.org/10.1093/humrep....
92.
Jungwirth A, Diemer T, Dohle GR, et al. Rekomendacje dotyczące postępowania w męskiej niepłodności. Post Androl. Online 2016; 3(2): 17–54. URL: http://www.postepyandrologii.p... (28.09.2020).
93.
Maksym RB, Ruta H, Konarski Ł, et al. Znaczenie optymalizacji tempe-ratury jąder dla poprawy płodności męskiej. Kwart Nauk. 2019; 3(39): 107–114. https://doi.org/10.34766/fetr.....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.