REVIEW PAPER
Clinical usefulness of melatonin MT1 and MT2 receptor agonists in the treatment of sleep disorders and depression
1
Studenckie Koło Naukowe przy Katedrze i Zakładzie Farmakologii z Farmakodynamiką, Uniwersytet Medyczny w Lublinie
2
Katedra i Zakład Farmakologii z Farmakodynamiką, Uniwersytet Medyczny w Lublinie
Corresponding author
Sara Hmaidan
Studenckie Koło Naukowe przy Katedrze i Zakładzie Farmakologii z Farmakodynamiką, Uniwersytet Medyczny w Lublinie
Studenckie Koło Naukowe przy Katedrze i Zakładzie Farmakologii z Farmakodynamiką, Uniwersytet Medyczny w Lublinie
Med Og Nauk Zdr. 2022;28(3):230-238
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Melatonin is the most important compound produced by the pineal gland. Its daily secretion cycle is responsible for the normal rhythm of sleep and wakefulness. The aim of the study was to analyse the clinical application of melatonin and melatonin receptor agonists MT1 and MT2 in the treatment of sleep disorders and depression.
Review methods:
A literature review was performed by searching electronic databases, such as PubMed, Scopus, Google Scholar, Web of Science, entering key words ‘melatonin’, ‘ramelteon’, ‘tasimelteon’, ‘sleep disorders’ in Polish and English.
Brief description of the state of knowledge:
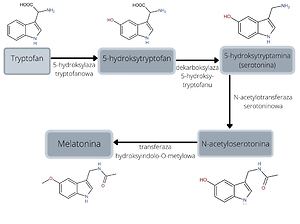
The action of melatonin is determined by its agonistic effect on the melatonin receptors MT1 and MT2. Darkness stimulates the synthesis of this hormone, and the suprachiasmatic nuclei of the hypothalamus (SCN) are responsible for regulation of melatonin secretion. The appearance of melatonin production disorders is a phenomenon observed most frequently in elderly people, the blind, those undertaking shift work or travelling intercontinentally. In addition to melatonin, other MT1 and MT2 receptor agonists such as ramelteon, tasimelteon or agomelatine are used in the treatment of sleep disorders. However, the latter is used primarily as an antidepressant, due to its additional antagonistic effect on serotonin 5-HT2C receptors.
Summary:
Abnormalities of melatonin secretion can lead to sleep disorders, as well as other conditions throughout the body. Melatonin receptor agonists are recognised as relatively well tolerated and safe, and their use may be considered in a wide range of patients.
Melatonin is the most important compound produced by the pineal gland. Its daily secretion cycle is responsible for the normal rhythm of sleep and wakefulness. The aim of the study was to analyse the clinical application of melatonin and melatonin receptor agonists MT1 and MT2 in the treatment of sleep disorders and depression.
Review methods:
A literature review was performed by searching electronic databases, such as PubMed, Scopus, Google Scholar, Web of Science, entering key words ‘melatonin’, ‘ramelteon’, ‘tasimelteon’, ‘sleep disorders’ in Polish and English.
Brief description of the state of knowledge:
The action of melatonin is determined by its agonistic effect on the melatonin receptors MT1 and MT2. Darkness stimulates the synthesis of this hormone, and the suprachiasmatic nuclei of the hypothalamus (SCN) are responsible for regulation of melatonin secretion. The appearance of melatonin production disorders is a phenomenon observed most frequently in elderly people, the blind, those undertaking shift work or travelling intercontinentally. In addition to melatonin, other MT1 and MT2 receptor agonists such as ramelteon, tasimelteon or agomelatine are used in the treatment of sleep disorders. However, the latter is used primarily as an antidepressant, due to its additional antagonistic effect on serotonin 5-HT2C receptors.
Summary:
Abnormalities of melatonin secretion can lead to sleep disorders, as well as other conditions throughout the body. Melatonin receptor agonists are recognised as relatively well tolerated and safe, and their use may be considered in a wide range of patients.
REFERENCES (51)
1.
Winczyk K, Lepa N. Receptory melatoninowe- obecny stan wiedzy. Endokrynologia Polska. 2002; 53(3): 365–377.
2.
Zawilska JB. Melatonina- hormon o działaniu pro nasennym. Bromat Chem Toksykol. 2008; 41: 224–228.
3.
Claustrat B, Leston J. Melatonin: Physiological effects in humans. Neurochirurgie. 2015; 61(2–3): 77–84. https://doi.org/10.1016/j.neuc.... 2015.03.00.
5.
Foster JR. Melatonin in critically ill children. Journal of Pediatric Intensive Care. 2016; 5(04): 172–181. https://doi.org/10.1055/s-0036....
6.
Saptadip S. Physiological and pharmacological perspectives of melatonin. Archives of Physiology and Biochemistry. 2020; https://doi.org/10 .1080/13813455.2020.1770799.
7.
Anghel L, Baroiu L, Popazu CR, et al. Benefits and adverse events of melatonin use in the elderly (Review). Exp Ther Med. 2022; 23(3): 219. https://doi.org/10.3892/etm.20....
8.
Begemann K, Neumann AM, Oster H. Regulation and function of extra-SCN circadian oscillators in the brain. Acta Physiologica. 2020; 229(1): e13446. https://doi.org/10.1111/apha.1....
9.
Doghramji K. Melatonin and its receptors: a new class of sleep-promoting agents. Journal of Clinical Sleep Medicine. 2007; 3(5supll): S17-S23. https://doi.org/10.5664/jcsm.2....
10.
Cegieła U, Jawiec W, Pytlik M. Leki Nasenne i Uspokajające. W: Kompendium Farmakologii pod. red. W. Jańca. Wydawnictwo Lekarskie PZWL. Warszawa; 2021. s.102–106.
11.
Crooke A, Guzman-Aranguez A, Mediero A, et al. Effect of Melatonin and Analogues on Corneal Wound Healing: Involvement of Mt2 Melatonin Receptor. Current Eye Research. 2015; 40(1): 56–65. https://doi. org/10.3109/02713683.2014.914540.
12.
Liu J, Clough SJ, Hutchinson AJ, et al. MT1 and MT2 melatonin receptors: a therapeutic perspective. Annual review of pharmacology and toxicology. 2016; 56: 361–383. https://doi.org/10.1146/annure...- -pharmtox-010814–124742.
13.
Gobbi G, Comai S. Differential function of melatonin MT1 and MT2 Receptors in REM and NREM sleep. Frontiers in Endocrinology. 2019;87 https://doi.org/10.3389/fendo.....
14.
Cecon E, Liu L, Jockers R. Melatonin receptor structures shed new light on melatonin research. Journal of pineal research. 2019; 67(4): e12606.https://doi.org/10.1111/jpi.12....
15.
Danielczyk K, Dzięgiel P. Receptory melatoninowe MT1 oraz ich rola w onkostatycznym działaniu melatoniny. Postepy Hig Med Dosw.(online). 2009; 63: 425–434.
16.
Emet M, Ozcan H, Ozel L, et al. A review of melatonin, its receptors and drugs. The Eurasian journal of medicine. 2016; 48(2): 135–141. https://doi.org/10.5152/eurasi....
17.
Gawęda M. Wpływ bodźców świetlnych i nieświetlnych na zegar biologiczny. Kosmos. 2000; 49(1–2): 19–25.
18.
Greveling A, Wenzel AF. Melatonina, nowy cudowny środek? Wydawnictwo Lekarskie PZWL. Warszawa, 1997.
19.
Emet M, Uzkeser M, Guclu S, et al. Sleep Disorders in Shift Workers in the Emergency Department and Efficacy of Melatonin. Eurasian Journal of Emergency Medicine. 2016; 15(1): 48–53. https://doi.org/10.5152/eajem.....
20.
Kun X, Cai Hong H, Subramanian P. Melatonin and sleep. Biological Rhythm Research. 2019; 50(3): 490–493. https://doi.org/10.1080/0929 1016.2018.1443554.
21.
Chrustek A, Olszewska-Słonina D. Melatonin as a powerful antioxidant. Acta Pharmaceutica. 2021; 71(3): 335–54. https://doi.org/10.2478/acph-2....
22.
Opie LH, Lecour S. Melatonin has multiorgan effects. European Heart Journal- Cardiovascular Pharmacotherapy. 2016; 2(4): 258–265. https://doi.org/10.1093/ehjcvp....
23.
Wardas J, Kosmowska B. Zaburzenia fazy snu REM jako wczesny marker choroby Parkinsona. Kosmos. 2020; 69(3): 509–521. https:// doi.org/10.36921/kos.2020_2687.
24.
Brzęczek M, Słonka K, Hyla-Klekot L. Melatonina– hormon o plejotropowym działaniu. Pediatria i Medycyna Rodzinna. 2016; 12(2):127–133.
25.
Gursoy AY, Kiseli M, Caglar GS. Melatonin in aging women. Climacteric. 2015; 18(6): 790–796. https://doi.org/10.3109/136971....
26.
Andersen LPH, Gogenur I, Rosenberg J, et al. The safety of melatonin in humans. Clin Drug Investig. 2016; 36: 169–175. https://doi.org/10.1007/ s40261–015–0368–5.
27.
Arendt J. Melatonin: countering chaotic time cues. Frontiers in endocrinology. 2019; 10(391). https://doi.org/10.3389/fendo.....
28.
Wei S, Smits GM, Tang X, et al. Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials. Sleep Medicine. 2020; 68: 1–8. https:// doi.org/10.1016/j.sleep.2019.02.017.
29.
Papagiannidou E, Skene DJ, Ioannides C. Potential drug interactions with melatonin. Physiology & behavior. 2014; 131: 17–24. https://doi. org/10.1016/j.physbeh.2014.04.016.
30.
Imenshahidi M, Karimi G, Hosseinzadeh H. Effects of melatonin on cardiovascular risk factors and metabolic syndrome: a comprehensive review. Naunyn-Schmiedeberg›s Arch Pharmacol. 2020; 393: 521–536. https://doi.org/10.1007/s00210....
31.
Ferlazzo N, Andolina G, Cannata A, et al. Is melatonin the cornucopia of the 21st century?. Antioxidants. 2020; 9(11): 1088. https://doi. org/10.3390/antiox9111088.
32.
Sun H, Gusdon AM, Qu S. Effects of melatonin on cardiovascular diseases: progress in the past year. Current opinion in lipidology. 2016;27(4): 408–413. https://doi.org/10.1097/MOL.00....
34.
Awgul S, Uździcki A, Żelazny P, i wsp. Farmakologiczne leczenie bezsenności- obecnie dostępne terapie oraz nowe kierunki badań. Farm Współ. 2018; 11: 207–214.
35.
Šonka K, Šóš P, Susta M. Past and present in drug treatment of sleep disorders. Neuroendocrinology Letters. 2014; 35(3): 186–197.
36.
Carocci A, Catalano A, Sinicropi MS. Melatonergic drugs in development. Clin Pharmacol. 2014; 6: 127–137 https://doi.org/10.2147/ CPAA.S36600.
38.
Wang YQ, Jiang YJ, Zou MS, et al. Antidepressant actions of melatonin and melatonin receptor agonist: Focus on pathophysiology and treatment. Behavioural brain research. 2021; 113724. https://doi. org/10.1016/j.bbr.2021.113724.
39.
Simpson D, Curran MP. Ramelteon. Drugs. 2008; 68: 1901–1919. https:// doi.org/10.2165/00003495–200868130–00011.
40.
Kuriyama A, Honda M, Hayashino Y. Ramelteon for the treatment of insomnia in adults: a systematic review and meta-analysis. Sleep medicine. 2014; 15(4): 385–92. https://doi.org/10.1016/j.slee....
41.
Berezińska M, Lorenc-Duda A, Zawilska JB. Ramelteon– lek nasenny nowej generacji. Farm Pol. 2010; 66(3): 173–178.
42.
Dhillon S, Clarke M. Tasimelteon: First Global Approval. Drugs. 2014; 74: 505–511. https://doi.org/10.1007/s40265....
43.
Lockley SW, Dressman MA, Licamele L, et al. Tasimelteon for non-24- -hour sleep–wake disorder in totally blind people (SET and RESET): two multicentre, randomised, double-masked, placebo-controlled phase 3 trials. The Lancet. 2015; 386(10005): 1754–1764. https://doi.org/10.1016/ S0140–6736(15)60031–9.
44.
Johnsa DJ, Neville MW. Tasimelteon: a melatonin receptor agonist for non-24-hour sleep-wake disorder. Annals of Pharmacotherapy. 2014; 48(12): 1636–1641. https://doi.org/10.1177/106002....
45.
Lavedan C, Forsberg M, Gentile AJ. Tasimelteon: a selective and unique receptor binding profile. Neuropharmacology. 2015; 91: 142–147. https://doi.org/10.1016/j.neur....
46.
Torres R, Dressman MA, Kramer WG, et al. Absolute bioavailability of tasimelteon. American Journal of Therapeutics. 2015; 22(5): 355–360. https://doi.org/10.1097/MJT.00....
47.
Białecka M. Agomelatyna w ocenie farmakologa i neurologa- bezpieczeństwo I zastosowanie kliniczne. Neuropsychiatria. Przegląd kliniczny. 2021; 13(1–2): 6–14. https://doi.org/10.24292/01.NP....
48.
Landowski J. Agomelatyna- oryginalny lek przeciwdepresyjny. Psychiatria. 2012; 9(1): 11–20.
49.
Rybakowski J. Koncepcja melatoninowa patogenezy i leczenia depresji. Farmakoter Psychiatr Neurol. 2008; 3: 133–140.
50.
Cegieła U, Jawiec W, Pytlik M. Leki Przeciwlękowe, Przeciwpsychotyczne i Przeciwdepresyjne. W: Kompendium Farmakologii pod. red. W. Jańca. Wydawnictwo Lekarskie PZWL. Warszawa; 2021. s.52–94.
51.
Siwek M, Wasik A, Krupa A. Agomelatine– pharmacological properties and use in psychiatric practice. Psychiatr Psychol Klin. 2019; 19(2): 188–203. https://doi.org/10.15557/PiPK.....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.