REVIEW PAPER
Intestinal diverticula – discussion of the current state of knowledge
1
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Corresponding author
Błażej Szymczuk
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Med Og Nauk Zdr. 2024;30(4):283-288
KEYWORDS
TOPICS
Biomedyczne aspekty zdrowia i chorobyZdrowie publiczneEpidemiologiaZdrowie środowiskoweŻywność i żywienieProfilaktyka chorób cywilizacyjnychPromocja zdrowia i edukacja zdrowotna
ABSTRACT
Introduction and objective:
Diverticula of the colon are defined as pouch-like protrusions of the intestinal wall through the muscular layer at sites of reduced resistance. Diverticula of the sigmoid colon are one of the most common pathologies of the large intestine detected during colonoscopy. In Western countries, the prevalence of diverticula is increasing. Over time, inflammation and bleeding associated with the presence of diverticula may occur. The aim of the study is to present the current state of knowledge on the epidemiology, diagnosis, and treatment methods of diverticular disease of the large intestine.
Review methods:
The literature review was conducted using the PubMed database. Phrases were searched for in English: „diverticular disease”, „diverticula”, „diverticula treatment” and „diverticula etiology”.
Brief description of the state of knowledge:
Risk factors for the occurrence of diverticula of the large intestine include, among others, a low-fibre diet, frequent alcohol consumption, smoking, and obesity. The presence of symptoms such as bloating, abdominal pain, change in bowel habits, bleeding, acute inflammation, or perforation of diverticula is referred to as diverticular disease. The diagnosis of diverticula of the large intestine is most commonly based on computed tomography of the abdomen and pelvis and colonoscopy. The treatment of symptomatic diverticula of the colon is challenging and includes pharmacotherapy, dietary modifications, and in some cases, endoscopic or surgical treatment.
Summary:
Diverticular disease of the large intestine poses a significant and growing clinical problem. The selection of appropriate diagnostic and treatment techniques, ensuring patient safety, depends on many factors and presents a major challenge for the treating team.
Diverticula of the colon are defined as pouch-like protrusions of the intestinal wall through the muscular layer at sites of reduced resistance. Diverticula of the sigmoid colon are one of the most common pathologies of the large intestine detected during colonoscopy. In Western countries, the prevalence of diverticula is increasing. Over time, inflammation and bleeding associated with the presence of diverticula may occur. The aim of the study is to present the current state of knowledge on the epidemiology, diagnosis, and treatment methods of diverticular disease of the large intestine.
Review methods:
The literature review was conducted using the PubMed database. Phrases were searched for in English: „diverticular disease”, „diverticula”, „diverticula treatment” and „diverticula etiology”.
Brief description of the state of knowledge:
Risk factors for the occurrence of diverticula of the large intestine include, among others, a low-fibre diet, frequent alcohol consumption, smoking, and obesity. The presence of symptoms such as bloating, abdominal pain, change in bowel habits, bleeding, acute inflammation, or perforation of diverticula is referred to as diverticular disease. The diagnosis of diverticula of the large intestine is most commonly based on computed tomography of the abdomen and pelvis and colonoscopy. The treatment of symptomatic diverticula of the colon is challenging and includes pharmacotherapy, dietary modifications, and in some cases, endoscopic or surgical treatment.
Summary:
Diverticular disease of the large intestine poses a significant and growing clinical problem. The selection of appropriate diagnostic and treatment techniques, ensuring patient safety, depends on many factors and presents a major challenge for the treating team.
REFERENCES (41)
1.
Schieffer KM, Kline BP, Yochum GS, et al. Pathophysiology of diverticular disease. Expert RevGastroenterol Hepatol. 2018;12(7):683–692. https://doi.org/10.1080/174741....
2.
Brian West A. The pathology of diverticulosis: classical concepts and mucosal changes indiverticula. J Clin Gastroenterol. 2006;40(3):126–131. https://doi.org/10.1097/01.mcg....
3.
Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management ofdiverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther. 2015;42(6):664–684.https://doi.org/10.1111/apt.13....
4.
Tursi A. Diverticulosis today: unfashionable and still under-researched. Therap Adv Gastroenterol.2016;9(2):213–228. https://doi.org/10.1177/175628....
5.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lowergastrointestinal diseases. Gastroenterology. 2009;136(3):741–754. https://doi.org/10.1053/j.gast....
6.
Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, andPancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162(2):621–644. https://doi.org/10.1053/j.gast....
7.
Yamada E, Inamori M, Uchida E, et al. Association between the location of diverticular disease andthe irritable bowel syndrome: a multicenter study in Japan. Am J Gastroenterol. 2014;109(12):1900–1905. https://doi.org/10.1038/ajg.20....
8.
Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health andprevention. Aliment Pharmacol Ther. 2003;18(3):71–74. https://doi.org/10.1046/j.0953....
9.
Blachut K, Paradowski L, Garcarek J. Prevalence and distribution of the colonic diverticulosis.Review of 417 cases from Lower Silesia in Poland. Rom J Gastroenterol. 2004;13(4):281–285.
10.
Peery AF, Sandler RS. Diverticular disease: reconsidering conventional wisdom. ClinGastroenterol Hepatol. 2013;11(12):1532–1537. https://doi.org/10.1016/j.cgh.....
11.
Rezapour M, Ali S, Stollman N. Diverticular Disease: An Update on Pathogenesis andManagement. Gut Liver. 2018;12(2):125–132. https://doi.org/10.5009/gnl165....
12.
Bailey J, Dattani S, Jennings A. Diverticular Disease: Rapid Evidence Review. Am Fam Physician.2022;106(2):150–156.
13.
Schultz JK, Azhar N, Binda GA, et al. European Society of Coloproctology: guidelines for themanagement of diverticular disease of the colon. Colorectal Dis. 2020;22(2):5–28. https://doi.org/10.1111/codi.1....
14.
Gralnek IM, Neeman Z, Strate LL. Acute Lower Gastrointestinal Bleeding. N Engl J Med. 2017;376(11):1054–1063. https://doi.org/10.1056/NEJMcp....
15.
Yamamichi N, Shimamoto T, Takahashi Y, et al. Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formation. PLoS One. 2015;10(4):e0123688. https://doi.org/10.1371/journa....
16.
Crowe FL, Appleby PN, Allen NE, et al. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): prospective study of British vegetarians and non-vegetarians. BMJ. 2011;343:d4131. https://doi.org/10.1136/bmj.d4....
17.
Wedel T, Barrenschee M, Lange C, et al. Morphologic Basis for Developing Diverticular Disease,Diverticulitis, and Diverticular Bleeding. Viszeralmedizin. 2015;31(2):76–82. https://doi.org/10.1159/000381....
18.
Daniels L, Budding AE, de Korte N, et al. Fecal microbiome analysis as a diagnostic test fordiverticulitis. Eur J Clin Microbiol Infect Dis. 2014;33(11):1927–1936. https://doi.org/10.1007/s10096....
19.
Kvasnovsky CL, Leong LEX, Choo JM, et al. Clinical and symptom scores are significantlycorrelated with fecal microbiota features in patients with symptomatic uncomplicated diverticular disease: a pilot study. Eur J Gastroenterol Hepatol. 2018;30(1):107–112. https://doi.org/10.1097/MEG.00....
20.
Jones RB, Fodor AA, Peery AF, et al. An Aberrant Microbiota is not Strongly Associated withIncidental Colonic Diverticulosis. Sci Rep. 2018;8(1):4951.https://doi.org/10.1038/s41598....
21.
Painter NS. Diverticular disease of the colon--a disease of western civilisation. Dis Mon. 1970:3–57.
22.
Rosemar A, Ivarsson ML, Börjesson L, et al. Increased concentration of tissue-degrading matrixmetalloproteinases and their inhibitor in complicated diverticular disease. Scand J Gastroenterol. 2007;42(2):215–220. https://doi.org/10.1080/003655....
23.
Bassotti G, Battaglia E, Bellone G, et al. Interstitial cells of Cajal, enteric nerves, and glial cells incolonic diverticular disease. J Clin Pathol. 2005;58(9):973–977. https://doi.org/10.1136/jcp.20....
24.
Kruis W, Germer CT, Böhm S, et al. German guideline diverticular disease/diverticulitis: Part I: Methods, pathogenesis, epidemiology, clinical characteristics (definitions), natural course, diagnosis and classification. United European Gastroenterol J. 2022;10(9):923–939. https://doi.org/10.1002/ueg2.1....
25.
You H, Sweeny A, Cooper ML, et al. The management of diverticulitis: a review of the guidelines.Med J Aust. 2019;211(9):421–427. https://doi.org/10.5694/mja2.5....
26.
Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician. 2013 May 1;87(9):612–20. PMID: 23668524.
27.
Tursi A, Marinelli A, Laera F, et al. Complicated diverticulitis mimicking colonic carcinoma: combined approach with endoscopy and budesonide. BMJ Case Rep. 2019;12(12):e230608. https://doi.org/10.1136/bcr-20....
28.
Lahat A, Yanai H, Menachem Y, et al. The feasibility and risk of early colonoscopy in acutediverticulitis: a prospective controlled study. Endoscopy. 2007;39(6):521–524. https://doi.org/10.1055/s-2007....
29.
Lahat A, Necula D, Yavzori M, et al. Prolonged Recurrent Abdominal Pain is Associated With Ongoing Underlying Mucosal Inflammation in Patients who had an Episode of Acute Complicated Diverticulitis. J Clin Gastroenterol. 2019;53(5):e178-e185. https://doi.org/10.1097/MCG.00....
30.
Stollman N, Smalley W, Hirano I; AGA Institute Clinical Guidelines Committee. AmericanGastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology. 2015;149(7):1944–1949. https://doi.org/10.1053/j.gast....
31.
Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis.Dis Colon Rectum. 2014;57(3):284–294. https://doi.org/10.1097/DCR.00....
32.
Greenlee HB, Pienkos EJ, Vanderbilt PC, et al. Proceedings: Acute large bowel obstruction.Comparison of county, Veterans Administration, and community hospital populations. Arch Surg. 1974;108(4):470–476. https://doi.org/10.1001/archsu....
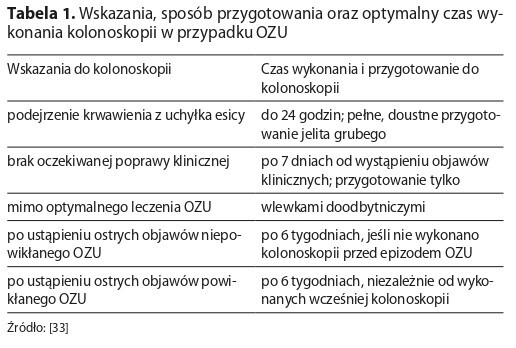
33.
Tursi A, Papa V, Lopetuso LR, Vetrone LM, Gasbarrini A, Papa A. When to Perform a Colonoscopy in Diverticular Disease and Why: A Personalized Approach. J Pers Med. 2022 Oct 14;12(10):1713. doi:10.3390/jpm12101713. PMID: 36294852; PMCID: PMC9605603.
34.
Wan D, Krisko T. Diverticulosis, Diverticulitis, and Diverticular Bleeding. Clin Geriatr Med. 2021;37(1):141–154. https://doi.org/10.1016/j.cger....
35.
Kupcinskas J, Strate LL, Bassotti G, et al. Pathogenesis of Diverticulosis and Diverticular Disease.J Gastrointestin Liver Dis. 2019;28(4):7–10. https://doi.org/10.15403/jgld-....
36.
Loosen SH, Paffenholz P, Luedde T, et al. Diverticular disease is associated with an increasedincidence rate of depression and anxiety disorders. Int J Colorectal Dis. 2021;36(11):2437–2443. https://doi.org/10.1007/s00384....
37.
Rezapour M, Stollman N. Diverticular Disease in the Elderly. Curr Gastroenterol Rep. 2019;21(9). https://doi.org/10.1007/s11894....
38.
Peery AF, Shaukat A, Strate LL. AGA Clinical Practice Update on Medical Management of ColonicDiverticulitis: Expert Review. Gastroenterology. 2021;160(3):906–911. e1. https://doi.org/10.1053/j.gast....
39.
Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lowergastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53(8):850–868. https://doi.org/10.1055/a-1496....
40.
Currie A, Christmas C, Aldean H, et al. Systematic review of self-expanding stents in themanagement of benign colorectal obstruction. Colorectal Dis. 2014;16(4):239–245. https://doi.org/10.1111/codi.1....
41.
van Hooft JE, Veld JV, Arnold D, et al. Self-expandable metal stents for obstructing colonic andextracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2020. Endoscopy. 2020;52(5):389–407. https://doi.org/10.1055/a-1140....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.