Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Uchyłki jelita – omówienie aktualnego stanu wiedzy
1
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Autor do korespondencji
Błażej Szymczuk
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Pracownia Endoskopii Przewodu Pokarmowego Uniwersyteckiego Centrum Klinicznego im. prof. K. Gibińskiego, Śląski Uniwersytet Medyczny, Katowice, Polska
Med Og Nauk Zdr. 2024;30(4):283-288
SŁOWA KLUCZOWE
DZIEDZINY
Biomedyczne aspekty zdrowia i chorobyZdrowie publiczneEpidemiologiaZdrowie środowiskoweŻywność i żywienieProfilaktyka chorób cywilizacyjnychPromocja zdrowia i edukacja zdrowotna
STRESZCZENIE
Wprowadzenie i cel:
Uchyłki okrężnicy definiowane są jako workowate uwypuklenia ściany jelita przechodzące przez warstwę mięśniową w tzw. miejscach zmniejszonej oporności. Uchyłki esicy stanowią jedną z najczęstszych patologii jelita grubego stwierdzanych w trakcie kolonoskopii. W krajach zachodnich częstość występowania uchyłków rośnie. Z czasem może dochodzić do zapalenia oraz krwawień związanych z występowaniem uchyłków. Celem pracy jest przedstawienie aktualnego stanu wiedzy na temat epidemiologii, diagnostyki oraz metod leczenia choroby uchyłkowej jelita grubego.
Metody przeglądu:
Do przeglądu piśmiennictwa użyto bazy PubMed. Wyszukiwano frazy w języku angielskim: „diverticular disease”, „diverticula”, „diverticula treatment”, „diverticula etiology”.
Opis stanu wiedzy:
Czynnikami ryzyka wystąpienia uchyłków jelita grubego są m.in. dieta uboga w błonnik, częste spożywanie alkoholu, palenie tytoniu oraz otyłość. Wystąpienie takich objawów jak wzdęcia, ból brzucha, zmiana rytmu wypróżnień, krwawienie, ostre zapalenie czy perforacja uchyłków określane jest mianem choroby uchyłkowej. Rozpoznanie uchyłków jelita grubego ustalane jest najczęściej na podstawie tomografii komputerowej jamy brzusznej i miednicy oraz kolonoskopii. Leczenie objawowych uchyłków okrężnicy jest trudne i obejmuje farmakoterapię, modyfikacje dietetyczne, a w niektórych przypadkach leczenie endoskopowe lub chirurgiczne.
Podsumowanie:
Choroba uchyłkowa jelita grubego stanowi istotny i narastający problem kliniczny. Dobór właściwych technik diagnostyki i leczenia, gwarantujący bezpieczeństwo pacjenta, uzależniony jest od wielu czynników i stanowi duże wyzwanie dla zespołu leczącego. Leczenie powikłanej choroby uchyłkowej obejmuje modyfikacje diety oraz stylu życia, a także małoinwazyjne zabiegi chirurgiczne oraz endoskopowe.
Uchyłki okrężnicy definiowane są jako workowate uwypuklenia ściany jelita przechodzące przez warstwę mięśniową w tzw. miejscach zmniejszonej oporności. Uchyłki esicy stanowią jedną z najczęstszych patologii jelita grubego stwierdzanych w trakcie kolonoskopii. W krajach zachodnich częstość występowania uchyłków rośnie. Z czasem może dochodzić do zapalenia oraz krwawień związanych z występowaniem uchyłków. Celem pracy jest przedstawienie aktualnego stanu wiedzy na temat epidemiologii, diagnostyki oraz metod leczenia choroby uchyłkowej jelita grubego.
Metody przeglądu:
Do przeglądu piśmiennictwa użyto bazy PubMed. Wyszukiwano frazy w języku angielskim: „diverticular disease”, „diverticula”, „diverticula treatment”, „diverticula etiology”.
Opis stanu wiedzy:
Czynnikami ryzyka wystąpienia uchyłków jelita grubego są m.in. dieta uboga w błonnik, częste spożywanie alkoholu, palenie tytoniu oraz otyłość. Wystąpienie takich objawów jak wzdęcia, ból brzucha, zmiana rytmu wypróżnień, krwawienie, ostre zapalenie czy perforacja uchyłków określane jest mianem choroby uchyłkowej. Rozpoznanie uchyłków jelita grubego ustalane jest najczęściej na podstawie tomografii komputerowej jamy brzusznej i miednicy oraz kolonoskopii. Leczenie objawowych uchyłków okrężnicy jest trudne i obejmuje farmakoterapię, modyfikacje dietetyczne, a w niektórych przypadkach leczenie endoskopowe lub chirurgiczne.
Podsumowanie:
Choroba uchyłkowa jelita grubego stanowi istotny i narastający problem kliniczny. Dobór właściwych technik diagnostyki i leczenia, gwarantujący bezpieczeństwo pacjenta, uzależniony jest od wielu czynników i stanowi duże wyzwanie dla zespołu leczącego. Leczenie powikłanej choroby uchyłkowej obejmuje modyfikacje diety oraz stylu życia, a także małoinwazyjne zabiegi chirurgiczne oraz endoskopowe.
Introduction and objective:
Diverticula of the colon are defined as pouch-like protrusions of the intestinal wall through the muscular layer at sites of reduced resistance. Diverticula of the sigmoid colon are one of the most common pathologies of the large intestine detected during colonoscopy. In Western countries, the prevalence of diverticula is increasing. Over time, inflammation and bleeding associated with the presence of diverticula may occur. The aim of the study is to present the current state of knowledge on the epidemiology, diagnosis, and treatment methods of diverticular disease of the large intestine.
Review methods:
The literature review was conducted using the PubMed database. Phrases were searched for in English: „diverticular disease”, „diverticula”, „diverticula treatment” and „diverticula etiology”.
Brief description of the state of knowledge:
Risk factors for the occurrence of diverticula of the large intestine include, among others, a low-fibre diet, frequent alcohol consumption, smoking, and obesity. The presence of symptoms such as bloating, abdominal pain, change in bowel habits, bleeding, acute inflammation, or perforation of diverticula is referred to as diverticular disease. The diagnosis of diverticula of the large intestine is most commonly based on computed tomography of the abdomen and pelvis and colonoscopy. The treatment of symptomatic diverticula of the colon is challenging and includes pharmacotherapy, dietary modifications, and in some cases, endoscopic or surgical treatment.
Summary:
Diverticular disease of the large intestine poses a significant and growing clinical problem. The selection of appropriate diagnostic and treatment techniques, ensuring patient safety, depends on many factors and presents a major challenge for the treating team.
Diverticula of the colon are defined as pouch-like protrusions of the intestinal wall through the muscular layer at sites of reduced resistance. Diverticula of the sigmoid colon are one of the most common pathologies of the large intestine detected during colonoscopy. In Western countries, the prevalence of diverticula is increasing. Over time, inflammation and bleeding associated with the presence of diverticula may occur. The aim of the study is to present the current state of knowledge on the epidemiology, diagnosis, and treatment methods of diverticular disease of the large intestine.
Review methods:
The literature review was conducted using the PubMed database. Phrases were searched for in English: „diverticular disease”, „diverticula”, „diverticula treatment” and „diverticula etiology”.
Brief description of the state of knowledge:
Risk factors for the occurrence of diverticula of the large intestine include, among others, a low-fibre diet, frequent alcohol consumption, smoking, and obesity. The presence of symptoms such as bloating, abdominal pain, change in bowel habits, bleeding, acute inflammation, or perforation of diverticula is referred to as diverticular disease. The diagnosis of diverticula of the large intestine is most commonly based on computed tomography of the abdomen and pelvis and colonoscopy. The treatment of symptomatic diverticula of the colon is challenging and includes pharmacotherapy, dietary modifications, and in some cases, endoscopic or surgical treatment.
Summary:
Diverticular disease of the large intestine poses a significant and growing clinical problem. The selection of appropriate diagnostic and treatment techniques, ensuring patient safety, depends on many factors and presents a major challenge for the treating team.
Szymczuk B, Milczarek J, Iwan M, Wosiewicz P, Ostrowski B. Uchyłki jelita – omówienie aktualnego stanu wiedzy. Med Og Nauk Zdr. 2024; 30(4): 283–288. doi: 10.26444/monz/195443
REFERENCJE (41)
1.
Schieffer KM, Kline BP, Yochum GS, et al. Pathophysiology of diverticular disease. Expert RevGastroenterol Hepatol. 2018;12(7):683–692. https://doi.org/10.1080/174741....
2.
Brian West A. The pathology of diverticulosis: classical concepts and mucosal changes indiverticula. J Clin Gastroenterol. 2006;40(3):126–131. https://doi.org/10.1097/01.mcg....
3.
Tursi A, Papa A, Danese S. Review article: the pathophysiology and medical management ofdiverticulosis and diverticular disease of the colon. Aliment Pharmacol Ther. 2015;42(6):664–684.https://doi.org/10.1111/apt.13....
4.
Tursi A. Diverticulosis today: unfashionable and still under-researched. Therap Adv Gastroenterol.2016;9(2):213–228. https://doi.org/10.1177/175628....
5.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lowergastrointestinal diseases. Gastroenterology. 2009;136(3):741–754. https://doi.org/10.1053/j.gast....
6.
Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal, Liver, andPancreatic Diseases in the United States: Update 2021. Gastroenterology. 2022;162(2):621–644. https://doi.org/10.1053/j.gast....
7.
Yamada E, Inamori M, Uchida E, et al. Association between the location of diverticular disease andthe irritable bowel syndrome: a multicenter study in Japan. Am J Gastroenterol. 2014;109(12):1900–1905. https://doi.org/10.1038/ajg.20....
8.
Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health andprevention. Aliment Pharmacol Ther. 2003;18(3):71–74. https://doi.org/10.1046/j.0953....
9.
Blachut K, Paradowski L, Garcarek J. Prevalence and distribution of the colonic diverticulosis.Review of 417 cases from Lower Silesia in Poland. Rom J Gastroenterol. 2004;13(4):281–285.
10.
Peery AF, Sandler RS. Diverticular disease: reconsidering conventional wisdom. ClinGastroenterol Hepatol. 2013;11(12):1532–1537. https://doi.org/10.1016/j.cgh.....
11.
Rezapour M, Ali S, Stollman N. Diverticular Disease: An Update on Pathogenesis andManagement. Gut Liver. 2018;12(2):125–132. https://doi.org/10.5009/gnl165....
12.
Bailey J, Dattani S, Jennings A. Diverticular Disease: Rapid Evidence Review. Am Fam Physician.2022;106(2):150–156.
13.
Schultz JK, Azhar N, Binda GA, et al. European Society of Coloproctology: guidelines for themanagement of diverticular disease of the colon. Colorectal Dis. 2020;22(2):5–28. https://doi.org/10.1111/codi.1....
14.
Gralnek IM, Neeman Z, Strate LL. Acute Lower Gastrointestinal Bleeding. N Engl J Med. 2017;376(11):1054–1063. https://doi.org/10.1056/NEJMcp....
15.
Yamamichi N, Shimamoto T, Takahashi Y, et al. Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formation. PLoS One. 2015;10(4):e0123688. https://doi.org/10.1371/journa....
16.
Crowe FL, Appleby PN, Allen NE, et al. Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): prospective study of British vegetarians and non-vegetarians. BMJ. 2011;343:d4131. https://doi.org/10.1136/bmj.d4....
17.
Wedel T, Barrenschee M, Lange C, et al. Morphologic Basis for Developing Diverticular Disease,Diverticulitis, and Diverticular Bleeding. Viszeralmedizin. 2015;31(2):76–82. https://doi.org/10.1159/000381....
18.
Daniels L, Budding AE, de Korte N, et al. Fecal microbiome analysis as a diagnostic test fordiverticulitis. Eur J Clin Microbiol Infect Dis. 2014;33(11):1927–1936. https://doi.org/10.1007/s10096....
19.
Kvasnovsky CL, Leong LEX, Choo JM, et al. Clinical and symptom scores are significantlycorrelated with fecal microbiota features in patients with symptomatic uncomplicated diverticular disease: a pilot study. Eur J Gastroenterol Hepatol. 2018;30(1):107–112. https://doi.org/10.1097/MEG.00....
20.
Jones RB, Fodor AA, Peery AF, et al. An Aberrant Microbiota is not Strongly Associated withIncidental Colonic Diverticulosis. Sci Rep. 2018;8(1):4951.https://doi.org/10.1038/s41598....
21.
Painter NS. Diverticular disease of the colon--a disease of western civilisation. Dis Mon. 1970:3–57.
22.
Rosemar A, Ivarsson ML, Börjesson L, et al. Increased concentration of tissue-degrading matrixmetalloproteinases and their inhibitor in complicated diverticular disease. Scand J Gastroenterol. 2007;42(2):215–220. https://doi.org/10.1080/003655....
23.
Bassotti G, Battaglia E, Bellone G, et al. Interstitial cells of Cajal, enteric nerves, and glial cells incolonic diverticular disease. J Clin Pathol. 2005;58(9):973–977. https://doi.org/10.1136/jcp.20....
24.
Kruis W, Germer CT, Böhm S, et al. German guideline diverticular disease/diverticulitis: Part I: Methods, pathogenesis, epidemiology, clinical characteristics (definitions), natural course, diagnosis and classification. United European Gastroenterol J. 2022;10(9):923–939. https://doi.org/10.1002/ueg2.1....
25.
You H, Sweeny A, Cooper ML, et al. The management of diverticulitis: a review of the guidelines.Med J Aust. 2019;211(9):421–427. https://doi.org/10.5694/mja2.5....
26.
Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician. 2013 May 1;87(9):612–20. PMID: 23668524.
27.
Tursi A, Marinelli A, Laera F, et al. Complicated diverticulitis mimicking colonic carcinoma: combined approach with endoscopy and budesonide. BMJ Case Rep. 2019;12(12):e230608. https://doi.org/10.1136/bcr-20....
28.
Lahat A, Yanai H, Menachem Y, et al. The feasibility and risk of early colonoscopy in acutediverticulitis: a prospective controlled study. Endoscopy. 2007;39(6):521–524. https://doi.org/10.1055/s-2007....
29.
Lahat A, Necula D, Yavzori M, et al. Prolonged Recurrent Abdominal Pain is Associated With Ongoing Underlying Mucosal Inflammation in Patients who had an Episode of Acute Complicated Diverticulitis. J Clin Gastroenterol. 2019;53(5):e178-e185. https://doi.org/10.1097/MCG.00....
30.
Stollman N, Smalley W, Hirano I; AGA Institute Clinical Guidelines Committee. AmericanGastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology. 2015;149(7):1944–1949. https://doi.org/10.1053/j.gast....
31.
Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis.Dis Colon Rectum. 2014;57(3):284–294. https://doi.org/10.1097/DCR.00....
32.
Greenlee HB, Pienkos EJ, Vanderbilt PC, et al. Proceedings: Acute large bowel obstruction.Comparison of county, Veterans Administration, and community hospital populations. Arch Surg. 1974;108(4):470–476. https://doi.org/10.1001/archsu....
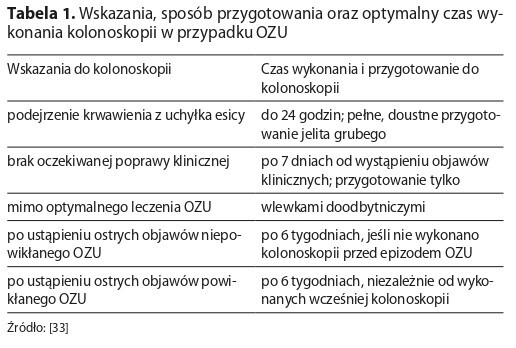
33.
Tursi A, Papa V, Lopetuso LR, Vetrone LM, Gasbarrini A, Papa A. When to Perform a Colonoscopy in Diverticular Disease and Why: A Personalized Approach. J Pers Med. 2022 Oct 14;12(10):1713. doi:10.3390/jpm12101713. PMID: 36294852; PMCID: PMC9605603.
34.
Wan D, Krisko T. Diverticulosis, Diverticulitis, and Diverticular Bleeding. Clin Geriatr Med. 2021;37(1):141–154. https://doi.org/10.1016/j.cger....
35.
Kupcinskas J, Strate LL, Bassotti G, et al. Pathogenesis of Diverticulosis and Diverticular Disease.J Gastrointestin Liver Dis. 2019;28(4):7–10. https://doi.org/10.15403/jgld-....
36.
Loosen SH, Paffenholz P, Luedde T, et al. Diverticular disease is associated with an increasedincidence rate of depression and anxiety disorders. Int J Colorectal Dis. 2021;36(11):2437–2443. https://doi.org/10.1007/s00384....
37.
Rezapour M, Stollman N. Diverticular Disease in the Elderly. Curr Gastroenterol Rep. 2019;21(9). https://doi.org/10.1007/s11894....
38.
Peery AF, Shaukat A, Strate LL. AGA Clinical Practice Update on Medical Management of ColonicDiverticulitis: Expert Review. Gastroenterology. 2021;160(3):906–911. e1. https://doi.org/10.1053/j.gast....
39.
Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lowergastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53(8):850–868. https://doi.org/10.1055/a-1496....
40.
Currie A, Christmas C, Aldean H, et al. Systematic review of self-expanding stents in themanagement of benign colorectal obstruction. Colorectal Dis. 2014;16(4):239–245. https://doi.org/10.1111/codi.1....
41.
van Hooft JE, Veld JV, Arnold D, et al. Self-expandable metal stents for obstructing colonic andextracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2020. Endoscopy. 2020;52(5):389–407. https://doi.org/10.1055/a-1140....
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.