RESEARCH PAPER
Women's awareness of possibilities of prophylaxis and physiotherapy used in the case of pelvic floor disorders
1
Zakład Biomechaniki i Kinezjologii, Wydział Nauk o Zdrowiu Uniwersytet Jagielloński Collegium Medicum, Polska
Corresponding author
Agnieszka Mazur-Biały
Zakład Biomechaniki i Kinezjologii, Wydział Nauk o Zdrowiu Uniwersytet Jagielloński Collegium Medicum, ul. Skawińska 8, 31-066, Kraków, Polska
Zakład Biomechaniki i Kinezjologii, Wydział Nauk o Zdrowiu Uniwersytet Jagielloński Collegium Medicum, ul. Skawińska 8, 31-066, Kraków, Polska
Med Og Nauk Zdr. 2024;30(3):252-258
KEYWORDS
urinary incontinencepelvic floor musclesurogynecological physiotherapywomen's awarenesspelvic floor prolaps
TOPICS
ABSTRACT
Introduction and objective:
Urinary incontinence (UI) and pelvic organ prolapse (POP) are common problems affecting a high percentage of women in Poland. The aim of the study was to assess preventive behaviours and the use of physiotherapyamong women qualified for surgical treatment due to UI or POP. The quality of life of patients with these dysfunctions was also assessed.
Material and methods:
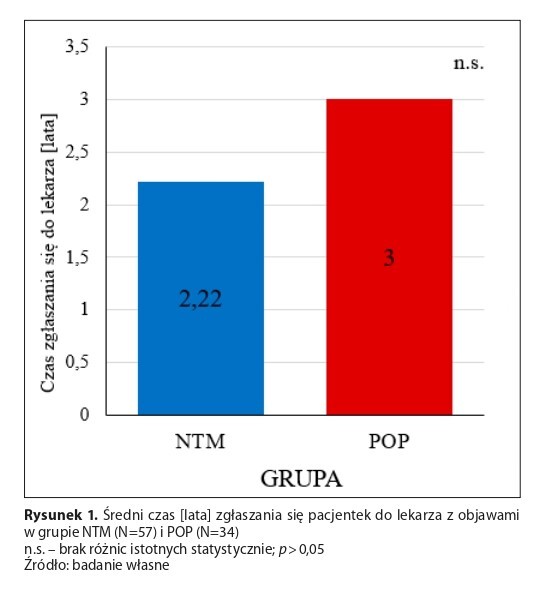
The survey included 165 patients aged 55.45±15.49 staying at the Department of Gynaecology. The study involved 34 patients hospitalized for organ prolapse (POP), 57 for urinary incontinence (UI) and 74 women hospitalized for other gynaecological reasons (Con). The research tools included an original questionnaire and standardized questionnaires assessing the severity of symptoms and quality of life in women with pelvic floor disorders: ICIQ FLUTS LF, ICIQ LUTSqol, and PFDI-20
Results:
Patients with UI were characterized by the lowest quality of life compared to women from POP or CON group, but the differences were not significant (p>0.05). Among women who consulted their urogynaecological problems with a doctor, only 24% were referred to a urogynaecological physiotherapist (31% with POP and 17% with UI). Only 8.8% of patients decided to have physiotherapy consultation (11.8% with POP and 7% with UI). 78% of all participants had never exercised their pelvic floor muscles (77% with UI, 73.5% with POP, and 83.5% from Con). Among women who reported exercising their pelvic floor muscles, 86% (UI) and 91.2% (POP), as well as 93% (Con), presented incorrect exercise patterns.
Conclusions:
Summing up, the research has shown that women›s awareness of the possibilities of preventive measures and physiotherapy for pelvic floor disorders, in this case UI and POP, is insufficient and further educational activities are necessary to improve this situation.
Urinary incontinence (UI) and pelvic organ prolapse (POP) are common problems affecting a high percentage of women in Poland. The aim of the study was to assess preventive behaviours and the use of physiotherapyamong women qualified for surgical treatment due to UI or POP. The quality of life of patients with these dysfunctions was also assessed.
Material and methods:
The survey included 165 patients aged 55.45±15.49 staying at the Department of Gynaecology. The study involved 34 patients hospitalized for organ prolapse (POP), 57 for urinary incontinence (UI) and 74 women hospitalized for other gynaecological reasons (Con). The research tools included an original questionnaire and standardized questionnaires assessing the severity of symptoms and quality of life in women with pelvic floor disorders: ICIQ FLUTS LF, ICIQ LUTSqol, and PFDI-20
Results:
Patients with UI were characterized by the lowest quality of life compared to women from POP or CON group, but the differences were not significant (p>0.05). Among women who consulted their urogynaecological problems with a doctor, only 24% were referred to a urogynaecological physiotherapist (31% with POP and 17% with UI). Only 8.8% of patients decided to have physiotherapy consultation (11.8% with POP and 7% with UI). 78% of all participants had never exercised their pelvic floor muscles (77% with UI, 73.5% with POP, and 83.5% from Con). Among women who reported exercising their pelvic floor muscles, 86% (UI) and 91.2% (POP), as well as 93% (Con), presented incorrect exercise patterns.
Conclusions:
Summing up, the research has shown that women›s awareness of the possibilities of preventive measures and physiotherapy for pelvic floor disorders, in this case UI and POP, is insufficient and further educational activities are necessary to improve this situation.
REFERENCES (25)
1.
Tim S, Mazur-Bialy AI. The Most Common Functional Disorders and Factors Affecting Female Pelvic Floor. Life (Basel). 2021;11(12):1397. https://doi.org/10.3390/life11....
2.
Petros P. The integral theory paradigm in practice-addressing a major health crisis in bladder/bowel/pain management. Ann Transl Med. 2024;12(2):22. doi:10.21037/atm-23-1755.
3.
Pietrus M, Białoń M, Ludwin I, et al. Etiologia i czynniki ryzyka zaburzeń statyki kobiecego narządu rodnego oraz nietrzymania moczu. Curr Gynecol Oncol. 2019;17(2):69–77. https://doi.org/10.15557/CGO.2....
4.
Milsom I, Altman D, Cartwright R, et al. Epidemiology Of Urinary Incontinence (UI) And Other Lower Urinary Tract Symptoms (LUTS), Pelvic Organ Prolapse (POP) And Anal (AI) Incontinence. In: Cardozo L, Rovner E, Wagg A, et al. Incontinence 7th edition. ICUD ICS; 2023. p. 30.
5.
Ciepiela K, Michalczuk K, Michałek T, et al. Pacjent NTM w systemie opieki zdrowotnej 2023. 12 edycja raportu. OCI Sp. z o.o; 2023. p. 5, 7, 9, 55.
6.
Mack I, Hahn H, Gödel C, et al. Global Prevalence of Fecal Incontinence in Community-Dwelling Adults: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2024;22(4):712–731.e8. doi:10.1016/j.cgh.2023.09.004.
7.
Brown HW, Hegde A, Huebner M, et al. International urogynecology consultation chapter 1 committee 2: Epidemiology of pelvic organ prolapse: prevalence, incidence, natural history, and service needs. Int Urogynecol J. 2022;33(2):173–187. https://doi.org/10.1007/s00192....
8.
Radziszewski P, Baranowski W, Nowak-Markwitz, et al. Wytyczne Zespołu Ekspertów odnośnie postępowania diagnostyczno-terapeutycznego u kobiet z nietrzymaniem moczu i pęcherzem nadreaktywnym. Ginekol Pol. 2010;81:789–793.
9.
Burkhard FC, Bosch JLHR, Cruz F, et al. Pelvic floor muscle training (PFMT). In: Burkhard FC, Bosch JLHR, Cruz F, et al. EUA Guidelines on Urinary Incontinence in Adults, European Association of Urology; 2020. p. 26–30.
10.
Jóźwik M, Szymanowski P, Marciniak W. Interdyscyplinarne wytyczne Polskiego Towarzystwa Uroginekologicznego odnośnie diagnostyki i leczenia wysiłkowego nietrzymania moczu u kobiet; 2014. https://ptug.pl/rekomendacje/i... (access: 2024.27.05).
11.
Mazur-Bialy AI, Kołomańska-Bogucka D, Opławski M, et al. Physiotherapy for Prevention and Treatment of Fecal Incontinence in Women-Systematic Review of Methods. J Clin Med. 2020;9(10):3255. https://doi.org/10.3390/jcm910....
12.
World Health Organization. Ageing and health; 2022. https://www.who.int/news-room/... (access: 2024.04.06).
13.
Swenson CW, Masteling M, DeLancey JO, et al. Aging effects on pelvic floor support: a pilot study comparing young versus older nulliparous women. Int Urogynecol J. 2020;31(3):535–543. doi:10.1007/s00192-019-04063-z.
14.
Peinado Molina RA, Hernández Martínez A, Martínez Vázquez S, et al. Influence of pelvic floor disorders on quality of life in women. Front Public Health. 2023;11:1180907. https://10.3389/fpubh.2023.118....
15.
Wągrodzka P, Dębowska W, Dębowska M, Szulc A. Quality of life and sexual function of women of reproductive age with urinary incontinence problems. Psychiatria Spersonalizowana. 2023;2(2):69–75. doi:10.5114/psychs.2023.131975.
16.
Kanadys K, Szczekala K, Stadnicka G, Woźnica E, Wiktor H. Analysis of quality of life in women treated for incontinence dependent on sociodemographic factors. Pielegniarstwo XXI wieku. 2020;19(1):8–14. https://doi.org/10.2478/pielxx....
17.
Tim S, Mazur-Biały A. Jakość życia i wiedza kobiet na temat metod fizjoterapeutycznych stosowanych w leczeniu nietrzymania moczu – co zmieniło się na przestrzeni lat? Naumowicz M, editor. Medycyna, zdrowie a styl życia. Człowiek wobec wyzwań współczesnego świata II. Łódź-Kielce: ArchaeGraph; 2021. p. 127–142.
18.
Połocka-Molińska M, Jakóbczak B, Plagens-Rotman. Wpływ nietrzymania moczu na jakość życia kobiet. Pol Prz Nauk Zdr. 2017;2(51):161–167. https://doi.org/10.20883/ppnoz....
19.
Kalata U, Pomian A, Jarkiewicz M, et al. Influence of Stress Urinary Incontinence and Pelvic Organ Prolapse on Depression, Anxiety, and Insomnia-A Comparative Observational Study. J Clin Med. 2023;13(1):185. doi:10.3390/jcm13010185.
20.
Toye F, Barker KL. A meta-ethnography to understand the experience of living with urinary incontinence: ‹is it just part and parcel of life?›. BMC Urol. 2020;20(1):1. https://doi.org/10.1186/s12894....
21.
Gugała B, Głaz J, Drelich A. Zapotrzebowanie na edukację w zakresie profilaktyki nietrzymania moczu u kobiet. Prz Med Uniw Rzesz Inst Leków. 2011;3:340–347.
22.
Steibliene V, Aniuliene R, Aniulis P, et al. Affective Symptoms and Health-Related Quality of Life Among Women with Stress Urinary Incontinence: Cross-Sectional Study. Neuropsychiatr Dis Treat. 2020;16:535–544. doi:10.2147/NDT.S236234.
23.
Barnaś E, Barańska E, Gawlik B, et al. Czynniki najbardziej wpływające na jakość życia kobiet z nietrzymaniem moczu. Hygeia Public Health. 2015;50(4):643–648.
24.
Mazur-Bialy AI, Kołomańska-Bogucka D, Nowakowski C, Tim S. Urinary Incontinence in Women: Modern Methods of Physiotherapy as a Support for Surgical Treatment or Independent Therapy. J Clin Med. 2020;9(4):1211. doi:10.3390/jcm9041211.
25.
Gozdan AM, Krajewska-Kułak E, Okurowska-Zawada B. Stan wiedzy kobiet na temat wpływu fizjoterapii uroginekologicznej na leczenie nietrzymania moczu. Bejda G, editor, Lewko J, Krajewska-Kułak E. Zachowania prozdrowotne jako element aktywności życiowej człowieka. Białystok: Uniwersytet Medyczny w Białymstoku; 2023. p. 151–172.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.