RESEARCH PAPER
Social support and the ability to control emotions in women hospitalized due to the risk of premature birth
1
Department of Midwifery, Carpathian State University, Krosno, Poland
2
Chair of Development in Midwifery, Faculty of Health Sciences, Medical University, Lublin
Corresponding author
Med Og Nauk Zdr. 2022;28(1):70-77
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Social support and emotional management during hospitalization due to obstetric com- plications can positively contribute to shaping one’s health condition and coping with difficult news or events. The aim of the study was to assess the level of social support and the ability to control emotions in pregnant women hospitalized due to a risk of preterm labour.
Material and methods:
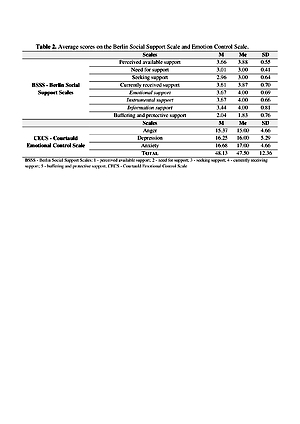
The study was conducted on a group of 120 women using standardized tools: Berlin Social Sup- port Scales (BSSS) and the Courtauld Emotional Control Scale (CECS).
Results:
Statistical analysis showed that age significantly influences the perception of available support (p =0.021) and currently received instrumental support (p=0.038). In the scale of buffering and protective support, the professional status is of significant importance (p=0.031). Financial situation is an important factor in terms of received emotional (p=0.038) and instrumental (p=0.030) support. Planning a pregnancy is important for the perception of available support (p=0.002), currently received support (p =0.006), emotional support (p=0.040) and buffering and protective support (p=0.018). The time of hospitalization affects the perception of information support received (p =0.036). The ability to control emotions depends on the place of residence (p=0.027) and education (p=0.030). The place of residence had an impact on the ability to suppress depression (p=0.015).
Conclusions:
The social dimension of life plays a role in the emotional coping mechanism. Emotional intelligence issues should be included in the care plan for a woman hospitalized due to the risk of preterm labour.
Social support and emotional management during hospitalization due to obstetric com- plications can positively contribute to shaping one’s health condition and coping with difficult news or events. The aim of the study was to assess the level of social support and the ability to control emotions in pregnant women hospitalized due to a risk of preterm labour.
Material and methods:
The study was conducted on a group of 120 women using standardized tools: Berlin Social Sup- port Scales (BSSS) and the Courtauld Emotional Control Scale (CECS).
Results:
Statistical analysis showed that age significantly influences the perception of available support (p =0.021) and currently received instrumental support (p=0.038). In the scale of buffering and protective support, the professional status is of significant importance (p=0.031). Financial situation is an important factor in terms of received emotional (p=0.038) and instrumental (p=0.030) support. Planning a pregnancy is important for the perception of available support (p=0.002), currently received support (p =0.006), emotional support (p=0.040) and buffering and protective support (p=0.018). The time of hospitalization affects the perception of information support received (p =0.036). The ability to control emotions depends on the place of residence (p=0.027) and education (p=0.030). The place of residence had an impact on the ability to suppress depression (p=0.015).
Conclusions:
The social dimension of life plays a role in the emotional coping mechanism. Emotional intelligence issues should be included in the care plan for a woman hospitalized due to the risk of preterm labour.
REFERENCES (20)
1.
Bedaso A, Adams J, Peng W, Sibbritt D. Prevalence and determinants of low social support during pregnancy among Australian women: a community-based cross-sectional study. Reprod Health. 2021; 27; 18(1): 158. https://doi: 10.1186/s12978-021-01210-y.
2.
Asselmann E, Kunas SL, Wittchen HU, Martini J. Maternal personality, social support, and changes in depressive, anxiety, and stress symptoms during pregnancy and after delivery: A prospective-longitudinal study. PLoS One. 2020; 24; 15(8): e0237609. https://doi: 10.1371/journal. pone.0237609.
3.
Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. 2021; 28; 18(1): 162. https:// doi: 10.1186/s12978-021-01209-5.
4.
World Health Organization: Preterm birth. World Health Organiza- tion, https://www.who.int/news-room/... (access: 09/08/2021).
5.
The American College of Obstetricians and Gynecologists: Committee Opinion no. 757 Screening for Perinatal Depression. https://www.acog. org/clinical/clinical-guidance/committee-opinion/articles/2018/11/ screening-for-perinatal-depression (access: 17/11/2021).
6.
Sęk H, Cieślak R, editor. Wsparcie społeczne, stres i zdrowie. 1st ed. Warszawa: PWN; 2011.
7.
Carter SK, Guittar SG. Emotion work among pregnant and birthing women. Midwifery 2014; 30: 1021–1028. https://doi: 10.1016/j.poł.2014.05.003.
8.
Łuszczynska A, Kowalska M, Mazurkiewicz M, Schwarzer R. Berlin Social Support Scales (BSSS): Polish version of BSSS and preeliminary results on its psychometric properties. Psychological Studies. 2006; 44: 17–27.
9.
Juczyński Z. Narzędzia pomiaru w promocji i psychologii zdrowia. Warszawa: Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego; 2009.
10.
Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, Klapp BF, Arck PC. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod. 2007; 22(3): 869–77. https://doi: 10.1093/humrep/del432.
11.
Shishehgar S, Mahmoodi A, Dolatian M, Mahmoodi Z, Bakhtiary M, Alavi Majd H. The Relationship of Social Support and Quality of Life with the Level of Stress in Pregnant Women Using the PATH Model. Iran Red Crescent Med J. 2013; 15(7): 560–5. https://doi: 10.5812/ircmj.12174.
12.
Iwanowicz-Palus G, Mróz, M, Bień A. Quality of life, social support and self-efficacy in women after a miscarriage. Health Qual Life Outcomes 2021; 19(16). https://doi.org/10.1186/s12955....
13.
Ghosh JK, Wilhelm MH, Dunkel-Schetter C, Lombardi CA, Ritz BR. Paternal support and preterm birth, and the moderation of effects of chronic stress: a study in Los Angeles county mothers. Arch Womens Ment Health. 2010; 13(4): 327–38. https://doi: 10.1007/s00737-009-0135-9.
14.
Fu W, Wilhelm LO, Wei Y, Zhou G, Schwarzer R. Emotional intelligence and dyadic satisfaction buffer the negative effect of stress on prenatal anxiety and depressive symptoms in Chinese women who are pregnant with twins. Anxiety Stress Coping. 2020; 33(4): 466–478. https://doi: 10.1080/10615806.2020.1745193.
15.
Tani F, Castagna V. Maternal social support, quality of birth expe-rience, and post-partum depression in primiparous women. J Matern Fetal Neonatal Med. 2017; 30(6): 689–692. https://doi:10.1080/147670 58.2016.1182980.
16.
Skurzak A, Korżyńska-Piętas M, Kicia M, Iwanowicz-Palus GJ. Wsparcie społeczne kobiet ciężarnych. Med Og Nauk Zdr. 2021; 27(1): 65–69. https://doi:10.26444/monz/1319....
17.
Espinosa A, Rudenstine S. The contribution of financial well-being, social support, and trait emotional intelligence on psychological distress. Br J Clin Psychol. 2020; 59(2): 224–240. https://doi:10.1111/bjc.12242.
18.
Zee KS, Bolger N, Higgins ET. Regulatory effectiveness of social sup- port. J Pers Soc Psychol. 2020; 119(6): 1316–1358. https://doi:10.1037/ pspi0000235.
19.
Johnson DR. Emotional intelligence as a crucial component to me- dical education. Int J Med Educ. 2015; 6: 179–83. https://doi:10.5116/ ijme.5654.3044.
20.
Guerra-Bustamante J, León-Del-Barco B, Yuste-Tosina R, López-Ramos VM, Mendo-Lázaro S. Emotional Intelligence and Psychological Well-Being in Adolescents. Int J Environ Res Public Health. 2019; 16(10): 1720. https://doi:10.3390/ijerph1610....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.