Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Krótkołańcuchowe kwasy tłuszczowe i ich wpływ na zdrowie człowieka – artykuł przeglądowy
1
5th year student, Faculty of Medicine, Medical University, Lublin, Poland
2
6th year student, Faculty of Medicine, Medical University, Lublin, Poland
3
Department of Cosmetology and Aesthetic Medicine, Medical University, Lublin, Poland
Autor do korespondencji
Med Og Nauk Zdr. 2024;30(3):181-185
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Krótkołańcuchowe kwasy tłuszczowe (ang. short-chain fatty acids, SCFA) to substancje, które są naturalnie wytwarzane i metabolizowane w organizmie człowieka. Niosą one liczne korzystne dla organizmu skutki i mogą wspomóc leczenie wielu chorób. W niniejszym artykule dokonano przeglądu aktualnego stanu wiedzy na temat SCFA, analizując ich produkcję, mechanizm działania i potencjalne zastosowanie w medycynie.
Metody przeglądu:
Niniejsza praca bazuje na analizie literatury dostępnej w bazie danych PubMed. Wykorzystane do przeglądu artykuły wyselekcjonowano z użyciem następujących słów kluczowych: „krótkołańcuchowe kwasy tłuszczowe”, „mikrobiom jelit”, „maślan”.
Opis stanu wiedzy:
Krótkołańcuchowe kwasy tłuszczowe są substancjami wytwarzanymi przez bakterie komensalne zamieszkujące jelito grube. Trzy główne SCFA to: maślan, propionian i octan. Są one produktami zachodzącego w przewodzie pokarmowym bakteryjnego metabolizmu błonnika pokarmowego. SCFA mają właściwości przeciwzapalne, modulują mikrobiotę jelitową i układ odpornościowy, pomagają utrzymać zdrowie jelit, w tym integralność bariery nabłonkowej jelit. Podjęto wiele prób zastosowania SCFA do leczenia różnych chorób, przy czym stwierdzono nieliczne działania niepożądane. Badania opierały się głównie na interwencjach dietetycznych, polegających na dostarczaniu błonnika, probiotyków i sfermentowanej żywności zawierającej SCFA. Obiecujące wyniki zaobserwowano w odniesieniu do terapii otyłości, cukrzycy, chorób zapalnych jelit, zaburzeń lipidowych i chorób sercowo-naczyniowych.
Podsumowanie:
Podsumowując, SCFA są niezbędne dla utrzymania ludzkiego zdrowia. Ich unikalna bioaktywność, naturalne występowanie i bezpieczeństwo mogą prowadzić do ich szerszego zastosowania w medycynie.
Krótkołańcuchowe kwasy tłuszczowe (ang. short-chain fatty acids, SCFA) to substancje, które są naturalnie wytwarzane i metabolizowane w organizmie człowieka. Niosą one liczne korzystne dla organizmu skutki i mogą wspomóc leczenie wielu chorób. W niniejszym artykule dokonano przeglądu aktualnego stanu wiedzy na temat SCFA, analizując ich produkcję, mechanizm działania i potencjalne zastosowanie w medycynie.
Metody przeglądu:
Niniejsza praca bazuje na analizie literatury dostępnej w bazie danych PubMed. Wykorzystane do przeglądu artykuły wyselekcjonowano z użyciem następujących słów kluczowych: „krótkołańcuchowe kwasy tłuszczowe”, „mikrobiom jelit”, „maślan”.
Opis stanu wiedzy:
Krótkołańcuchowe kwasy tłuszczowe są substancjami wytwarzanymi przez bakterie komensalne zamieszkujące jelito grube. Trzy główne SCFA to: maślan, propionian i octan. Są one produktami zachodzącego w przewodzie pokarmowym bakteryjnego metabolizmu błonnika pokarmowego. SCFA mają właściwości przeciwzapalne, modulują mikrobiotę jelitową i układ odpornościowy, pomagają utrzymać zdrowie jelit, w tym integralność bariery nabłonkowej jelit. Podjęto wiele prób zastosowania SCFA do leczenia różnych chorób, przy czym stwierdzono nieliczne działania niepożądane. Badania opierały się głównie na interwencjach dietetycznych, polegających na dostarczaniu błonnika, probiotyków i sfermentowanej żywności zawierającej SCFA. Obiecujące wyniki zaobserwowano w odniesieniu do terapii otyłości, cukrzycy, chorób zapalnych jelit, zaburzeń lipidowych i chorób sercowo-naczyniowych.
Podsumowanie:
Podsumowując, SCFA są niezbędne dla utrzymania ludzkiego zdrowia. Ich unikalna bioaktywność, naturalne występowanie i bezpieczeństwo mogą prowadzić do ich szerszego zastosowania w medycynie.
Introduction and objective:
Short-chain fatty acids (SCFA) are substances that are naturally produced and metabolised in the human body. They exert many beneficial effects on the system and could help treat many diseases. This paper reviews the current state of knowledge on SCFA, analysing their production, mechanism of action and potential use in medicine.
Review methods:
The review is based on an analysis of literature available in the PubMed database using the key words: ‹short-chain fatty acids, ‹gut microbiome›, ‹butyrate›.
Brief description of the state of knowledge:
Short-chain fatty acids are common substances produced by commensal bacteria residing in the large intestine. Three major SCFA are: butyrate, propionate and acetate, products of bacterial metabolism of dietary fibre that naturally occur in the gastrointestinal tract. SCFA have anti-inflammatory properties, modulate the gut microbiota and the immune system, help maintain the health of the gut, including the integrity of the intestinal epithelial barrier. Many attempts have been made to incorporate SCFA into the treatment of various diseases, and few adverse effects have been documented. The studies primarily focused on diet interventions with dietary fiber, probiotics and fermented foods containing SCFA. Promising results have been observed regarding, inter alia, the therapy of obesity, diabetes, inflammatory bowel diseases, lipid disorders and cardiovascular diseases.
Summary:
Short-chain fatty acids are vital for the mainteance of human health. Their unique bioactivity, natural occurrence and safety could potentially lead to their wider application in medicine.
Short-chain fatty acids (SCFA) are substances that are naturally produced and metabolised in the human body. They exert many beneficial effects on the system and could help treat many diseases. This paper reviews the current state of knowledge on SCFA, analysing their production, mechanism of action and potential use in medicine.
Review methods:
The review is based on an analysis of literature available in the PubMed database using the key words: ‹short-chain fatty acids, ‹gut microbiome›, ‹butyrate›.
Brief description of the state of knowledge:
Short-chain fatty acids are common substances produced by commensal bacteria residing in the large intestine. Three major SCFA are: butyrate, propionate and acetate, products of bacterial metabolism of dietary fibre that naturally occur in the gastrointestinal tract. SCFA have anti-inflammatory properties, modulate the gut microbiota and the immune system, help maintain the health of the gut, including the integrity of the intestinal epithelial barrier. Many attempts have been made to incorporate SCFA into the treatment of various diseases, and few adverse effects have been documented. The studies primarily focused on diet interventions with dietary fiber, probiotics and fermented foods containing SCFA. Promising results have been observed regarding, inter alia, the therapy of obesity, diabetes, inflammatory bowel diseases, lipid disorders and cardiovascular diseases.
Summary:
Short-chain fatty acids are vital for the mainteance of human health. Their unique bioactivity, natural occurrence and safety could potentially lead to their wider application in medicine.
Czachajda M, Góral A, Duszyńska K, Dolepski K, Żuk K, Firlej E. Short-chain fatty acids and their impact on human health- a review. Med Og
Nauk Zdr. 2024; 30(3): 181–185. doi: 10.26444/monz/190750
REFERENCJE (41)
1.
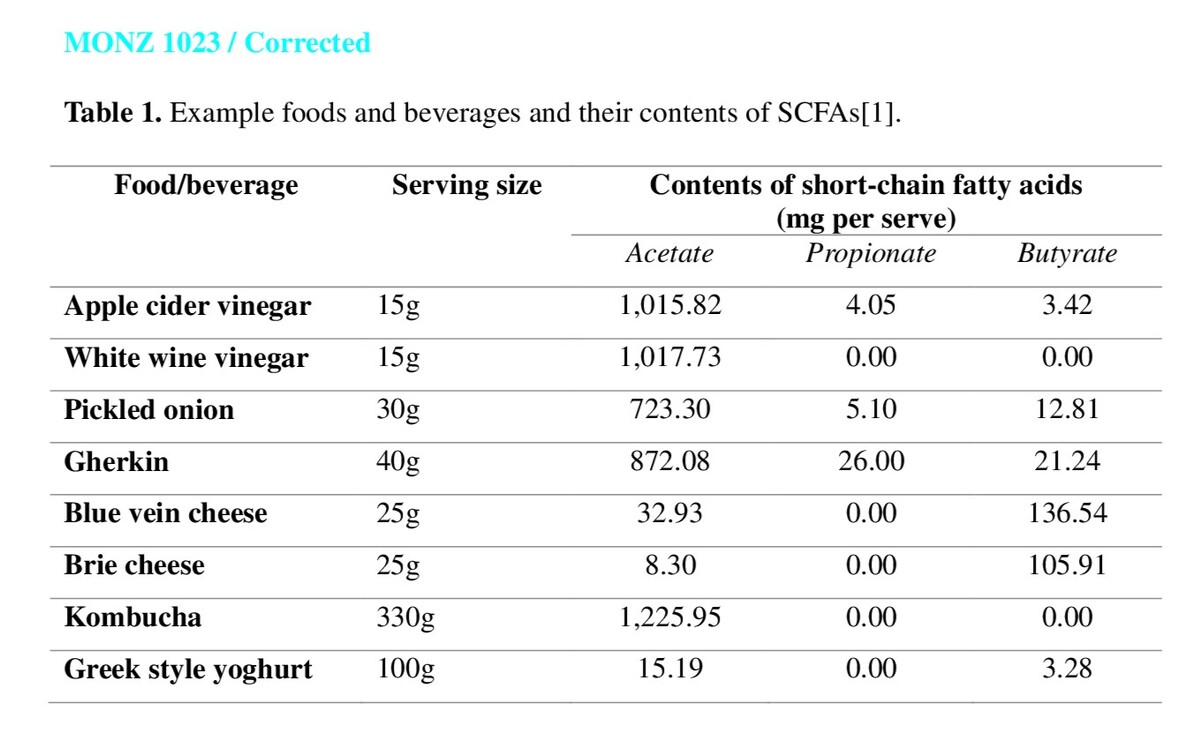
Gill PA, Bogatyrev A, van Zelm MC, et al. Delivery of Acetate to the Peripheral Blood after Consumption of Foods High in Short-Chain Fatty Acids. Mol Nutr Food Res. 2021;65(4):1–10. doi:10.1002/mnfr.202000953.
2.
Hu T, Wu Q, Yao Q, et al. Short-chain fatty acid metabolism and multiple effects on cardiovascular diseases. Ageing Res Rev. 2022;81:101706. doi:10.1016/J.ARR.2022.101706.
3.
Blaak EE, Canfora EE, Theis S, et al. Short chain fatty acids in human gut and metabolic health. Benef Microbes. 2020;11(5):411–455. doi:10.3920/ BM2020.0057.
4.
Xiong RG, Zhou DD, Wu SX, et al. Health Benefits and Side Effects of Short-Chain Fatty Acids. Foods. 2022;11(18). doi:10.3390/foods11182863.
5.
Igudesman D, Crandell JL, Corbin KD, et al. Associations of Dietary Intake with the Intestinal Microbiota and Short-Chain Fatty Acids Among Young Adults with Type 1 Diabetes and Overweight or Obesity. J Nutr. 2023;153(4):1178–1188. doi:10.1016/J.TJNUT.2022.12.017.
6.
Gilley SP, Ruebel ML, Sims C, et al. Associations between maternal obesity and offspring gut microbiome in the first year of life. Pediatr Obes. 2022;17(9):1–23. doi:10.1111/ijpo.12921.
7.
You X, Dadwal UC, Lenburg ME, et al. Murine Gut Microbiome Metaanalysis Reveals Alterations in Carbohydrate Metabolism in Response to Aging. 2022;(April):1–17.
8.
Merenstein D, Fraser CM, Roberts RF, et al. Bifidobacterium animalis subsp. lactis BB-12 Protects against Antibiotic-Induced Functional and Compositional Changes in Human Fecal Microbiome. Nutrients. 2021;13(8). doi:10.3390/NU13082814.
9.
Venegas DP, De La Fuente MK, Landskron G, et al. Short chain fatty acids (SCFAs)mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;10(MAR). doi:10.3389/fimmu.2019.00277.
10.
Frossi B, Carli M De, Calabrò A. Coeliac Disease and Mast Cells. Int J Mol Sci. 2019;20(14). doi:10.3390/IJMS20143400.
11.
Barbara G, Barbaro MR, Fuschi D, et al. Inflammatory and Microbiota- Related Regulation of the Intestinal Epithelial Barrier. Front Nutr. 2021;8. doi:10.3389/FNUT.2021.718356.
12.
Cardoso-Silva D, Delbue D, Itzlinger A, et al. Intestinal Barrier Function in Gluten-Related Disorders. Nutrients. 2019;11(10). doi:10.3390/ NU11102325.
13.
Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11(9):821–834. doi:10.1080/17474124.2017.1343143.
14.
Jabri B, Abadie V. IL-15 functions as a danger signal to regulate tissue-resident T cells and tissue destruction. Nat Rev Immunol. 2015;15(12):771–783. doi:10.1038/NRI3919.
15.
Ho H en, Chun Y, Jeong S, et al. Multidimensional study of the oral microbiome, metabolite, and immunologic environment in peanut allergy. J Allergy Clin Immunol. 2021;148(2):627–632.e3. doi:10.1016/j. jaci.2021.03.028.
16.
Facchin S, Vitulo N, Calgaro M, et al. Microbiota changes induced by microencapsulated sodium butyrate in patients with inflammatory bowel disease. Neurogastroenterol Motil. 2020;32(10):13–25. doi:10.1111/ nmo.13914.
17.
Kaliciak I, Drogowski K, Garczyk A, et al. Influence of Gluten-Free Diet on Gut Microbiota Composition in Patients with Coeliac Disease: A Systematic Review. Nutrients. 2022;14(10). doi:10.3390/NU14102083.
18.
1Gill PA, Muir JG, Gibson PR, et al. A randomized dietary intervention to increase colonic and peripheral blood SCFAs modulates the blood B- and T-cell compartments in healthy humans. Am J Clin Nutr. 2022;116(5):1354–1367. doi:10.1093/ajcn/nqac246.
19.
Bander Z Al, Nitert MD, Mousa A, et al. The gut microbiota and inflammation: An overview. Int J Environ Res Public Health. 2020;17(20):1–22. doi:10.3390/ijerph17207618.
20.
Wastyk HC, Fragiadakis GK, Perelman D, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184(16):4137–4153.e14. doi:10.1016/j.cell.2021.06.019.
21.
Feng Y, Zhu J, Wang Q, et al. White common bean extract remodels the gut microbiota and ameliorates type 2 diabetes and its complications: A randomized double-blinded placebo-controlled trial. Front Endocrinol (Lausanne). 2022;13(October):1–13. doi:10.3389/fendo.2022.999715.
22.
Pham NHT, Joglekar M V, Wong WKM, et al. Short-chain fatty acids and insulin sensitivity: a systematic review and meta-analysis. Nutr Rev. 2023;82(2):193–209. doi:10.1093/nutrit/nuad042.
23.
Medawar E, Beyer F, Thieleking R, et al. Prebiotic diet changes neural correlates of food decision-making in overweight adults: a randomised controlled within-subject cross-over trial. Gut. Published online 2023:298–310. doi:10.1136/gutjnl-2023-330365.
24.
Song J, Li Q, Everaert N, et al. Dietary Inulin Supplementation Modulates Short-Chain Fatty Acid Levels and Cecum Microbiota Composition and Function in Chickens Infected With Salmonella. Front Microbiol. 2020;11:584380. doi:10.3389/FMICB.2020.584380/FULL.
25.
Akinsuyi OS, Roesch LFW. Meta-Analysis Reveals Compositional and Functional Microbial Changes Associated with Osteoporosis. Microbiol Spectr. 2023;11(3):1–15. doi:10.1128/spectrum.00322-23.
26.
Zhang Q, Li G, Zhao W, et al. Efficacy of Bifidobacterium animalis subsp. lactis BL-99 in the treatment of functional dyspepsia: a randomized placebo-controlled clinical trial. Nat Commun. 2024;15(1). doi:10.1038/s41467-023-44292-x.
27.
Liu L, Sadaghian Sadabad M, Gabarrini G, et al. Riboflavin Supplementation Promotes Butyrate Production in the Absence of Gross Compositional Changes in the Gut Microbiota. Antioxidants Redox Signal. 2023;38(4):282–297. doi:10.1089/ars.2022.0033.
28.
Rahayu ES, Mariyatun M, Manurung NEP, et al. Effect of probiotic Lactobacillus plantarum Dad-13 powder consumption on the gut microbiota and intestinal health of overweight adults. World J Gastroenterol. 2021;126(1):107–128. doi:10.3748/WJG.V27.I1.107.
29.
Birkeland E, Gharagozlian S, Birkeland KI, et al. Prebiotic effect of inulin-type fructans on faecal microbiota and short-chain fatty acids in type 2 diabetes: a randomised controlled trial. Eur J Nutr. 2020;59(7):3325–3338. doi:10.1007/s00394-020-02282-5.
30.
Wernlund PG, Hvas CL, Dahlerup JF, et al. Casein glycomacropeptide is well tolerated in healthy adults and changes neither high-sensitive C-reactive protein, gut microbiota nor faecal butyrate: A restricted randomised trial. Br J Nutr. 2021;125(12):1374–1385. doi:10.1017/S0007114520003736.
31.
So D, Whelan K, Rossi M, et al. Dietary fiber intervention on gut microbiota composition in healthy adults: A systematic review and meta-analysis. Am J Clin Nutr. 2018;107(6):965–983. doi:10.1093/ajcn/nqy041.
32.
Brignardello J, Fountana S, Posma JM, et al. Characterization of diet-dependent temporal changes in circulating short-chain fatty acid concentrations: A randomized crossover dietary trial. Am J Clin Nutr. 2022;116(5):1368–1378. doi:10.1093/ajcn/nqab211.
33.
Ojo O, Feng QQ, Ojo OO, et al. The role of dietary fibre in modulating gut microbiota dysbiosis in patients with type 2 diabetes: A systematic review and meta-analysis of randomised controlled trials. Nutrients. 2020;12(11):1–21. doi:10.3390/nu12113239.
34.
Seethaler B, Nguyen NK, Basrai M, et al. Short-chain fatty acids are key mediators of the favorable effects of the Mediterranean diet on intestinal barrier integrity: data from the randomized controlled LIBRE trial. Am J Clin Nutr. 2022;116(4):928–942. doi:10.1093/ajcn/nqac175.
35.
Pietrzak A, Banasiuk M, Szczepanik M, et al. Sodium Butyrate Effectiveness in Children and Adolescents with Newly Diagnosed Inflammatory Bowel Diseases—Randomized Placebo-Controlled Multicenter Trial. Nutrients. 2022;14(16). doi:10.3390/NU14163283.
36.
Zheng J, An Y, Du Y, et al. Effects of short-chain fatty acids on blood glucose and lipid levels in mouse models of diabetes mellitus: a systematic review and network meta-analysis. Pharmacol Res. 2023;199(August 2023):107041. doi:10.1016/j.phrs.2023.107041.
37.
Xu D, Feng M, Chu YF, et al. The Prebiotic Effects of Oats on Blood Lipids, Gut Microbiota, and Short-Chain Fatty Acids in Mildly Hypercholesterolemic Subjects Compared With Rice: A Randomized, Controlled Trial. Front Immunol. 2021;12(December):1–16. doi:10.3389/fimmu.2021.787797.
38.
Zhou T, Sun D, Li X, et al. Genetically determined SCFA concentration modifies the association of dietary fiber intake with changes in bone mineral density during weight loss: The Preventing Overweight Using Novel Dietary Strategies (POUNDS LOST) trial. Am J Clin Nutr. 2021;114(1):42–48. doi:10.1093/ajcn/nqab037.
39.
Tilves C, Yeh HC, Maruthur N, et al. Increases in Circulating and Fecal Butyrate are Associated With Reduced Blood Pressure and Hypertension: Results From the SPIRIT Trial. J Am Heart Assoc. 2022;11(13). doi:10.1161/JAHA.121.024763.
40.
Neyrinck AM, Rodriguez J, Taminiau B, et al. Constipation Mitigation by Rhubarb Extract in Middle-Aged Adults Is Linked to Gut Microbiome Modulation: A Double-Blind Randomized Placebo-Controlled Trial. Int J Mol Sci. 2022;23(23). doi:10.3390/ijms232314685.
41.
Alvandi E, Wong WKM, Joglekar MV, et al. Short-chain fatty acid concentrations in the incidence and risk-stratification of colorectal cancer: a systematic review and meta-analysis. BMC Med. 2022;20(1):1–11. doi:10.1186/s12916-022-02529-4.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.