Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Wybrane czynniki ryzyka rozwoju raka odbytu i odbytnicy
1
Students’ Scientific Club, Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Silesian Medical University, Katowice, Poland
2
Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Silesian Medical University, Katowice, Poland
Autor do korespondencji
Martyna Szymańska
Student Scientific Club at odbytnicy the Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
Student Scientific Club at odbytnicy the Department of Environmental Medicine and Epidemiology, Faculty of Medical Sciences in Zabrze, Medical University of Silesia, Katowice, Poland
Med Og Nauk Zdr. 2025;31(1):6-12
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Złośliwe nowotwory odbytu i odbytnicy stanowią poważny problem zdrowotny na świecie, w tym w Polsce. W 2021 roku nowotwory złośliwe odbytnicy stanowiły 4,1% przypadków u mężczyzn i 2,4% u kobiet, a rak odbytu i kanału odbytu 0,5% wszystkich nowotworów. Nowotwory te zaliczane są do grupy nowotworów jelita grubego (C18-C21) według ICD-10 są one trzecim najczęstszym nowotworem u mężczyzn i drugim u kobiet na świecie. Celem pracy było opisanie wybranych czynników ryzyka rozwoju raka odbytu i odbytnicy na podstawie dostępnej literatury
Metody przeglądu:
Przeprowadzono przegląd literatury. Poszukiwano artykułów dotyczących raka odbytu i odbytnicy. Wyszukiwanie przeprowadzono w dwóch bazach danych: Google Scholar i PubMed, używając słów kluczowych takich jak: „rak”, „rak odbytu”, „rak odbytnicy”, „czynniki ryzyka”, „HPV”, „mikrobiota jelitowa”, „zaparcia”, „błonnik”, „otyłość”, „aktywność fizyczna”, „rak jelita grubego”. Przeanalizowano 34 artykuły naukowe z lat 2013–2023. Nie stosowano ograniczeń językowych, a wybór literatury został przeprowadzony samodzielnie na podstawie zgodności z tematem badania
Opis stanu wiedzy:
Czynnikami mogącymi zwiększać ryzyko rozwoju nowotworów odbytu lub odbytnicy jest starszy wiek, występowanie nowotworów w rodzinie, palenie tytoniu, infekcja wirusem HPV, otyłość, niski poziom aktywności fizycznej, zaparcia, nieprawidłowy skład mikrobioty oraz nieodpowiednia dieta.
Podsumowanie:
Rak odbytu i odbytnicy, mimo że tworzą się w miejscach bliskich anatomicznie, są to dwa odrębne schorzenia różniące się pod względem etiopatogenezy, czynników ryzyka, rokowań oraz metod leczenia. Chociaż rak brzegu odbytu i kanału odbytu jest stosunkowo rzadkim nowotworem złośliwym, w połączeniu z rakiem odbytnicy stanowi poważne zagrożenie zdrowotne. Jednak nowotworom tym można zapobiegać poprzez świadome wybory dotyczące stylu życia.
Złośliwe nowotwory odbytu i odbytnicy stanowią poważny problem zdrowotny na świecie, w tym w Polsce. W 2021 roku nowotwory złośliwe odbytnicy stanowiły 4,1% przypadków u mężczyzn i 2,4% u kobiet, a rak odbytu i kanału odbytu 0,5% wszystkich nowotworów. Nowotwory te zaliczane są do grupy nowotworów jelita grubego (C18-C21) według ICD-10 są one trzecim najczęstszym nowotworem u mężczyzn i drugim u kobiet na świecie. Celem pracy było opisanie wybranych czynników ryzyka rozwoju raka odbytu i odbytnicy na podstawie dostępnej literatury
Metody przeglądu:
Przeprowadzono przegląd literatury. Poszukiwano artykułów dotyczących raka odbytu i odbytnicy. Wyszukiwanie przeprowadzono w dwóch bazach danych: Google Scholar i PubMed, używając słów kluczowych takich jak: „rak”, „rak odbytu”, „rak odbytnicy”, „czynniki ryzyka”, „HPV”, „mikrobiota jelitowa”, „zaparcia”, „błonnik”, „otyłość”, „aktywność fizyczna”, „rak jelita grubego”. Przeanalizowano 34 artykuły naukowe z lat 2013–2023. Nie stosowano ograniczeń językowych, a wybór literatury został przeprowadzony samodzielnie na podstawie zgodności z tematem badania
Opis stanu wiedzy:
Czynnikami mogącymi zwiększać ryzyko rozwoju nowotworów odbytu lub odbytnicy jest starszy wiek, występowanie nowotworów w rodzinie, palenie tytoniu, infekcja wirusem HPV, otyłość, niski poziom aktywności fizycznej, zaparcia, nieprawidłowy skład mikrobioty oraz nieodpowiednia dieta.
Podsumowanie:
Rak odbytu i odbytnicy, mimo że tworzą się w miejscach bliskich anatomicznie, są to dwa odrębne schorzenia różniące się pod względem etiopatogenezy, czynników ryzyka, rokowań oraz metod leczenia. Chociaż rak brzegu odbytu i kanału odbytu jest stosunkowo rzadkim nowotworem złośliwym, w połączeniu z rakiem odbytnicy stanowi poważne zagrożenie zdrowotne. Jednak nowotworom tym można zapobiegać poprzez świadome wybory dotyczące stylu życia.
Introduction and objective:
Malignant tumours of the anus and rectum represent a serious health issue in Poland and worldwide. In Poland in 2021, malignant rectal cancers accounted for 4.1% of cases in men and 2.4% in women, while cancers of the anus and anal canal made up 0.5% of all cancers. These tumours are classified within the group of colorectal cancers (C18-C21) according to ICD-10. Globally, they are the third most common cancer in men and the second most common in women. The aim of this article is to describe selected risk factors for the development of anal and rectal cancer based on available literature
Review methods:
A literature review was conducted, focusing on articles related to anal and rectal cancer. The search was performed in two databases: Google Scholar and PubMed, using such key words as: cancer, anal cancer, rectal cancer, risk factors, HPV, microbiota, gut microbiota, constipation, fibre, obesity, physical activity, colorectal cancer. A total of 34 scientific articles from 2013–2023 were analyzed. No language restrictions were applied, and the selection of literature was made independently based on its relevance to the research topic.
Brief description of the state of knowledge:
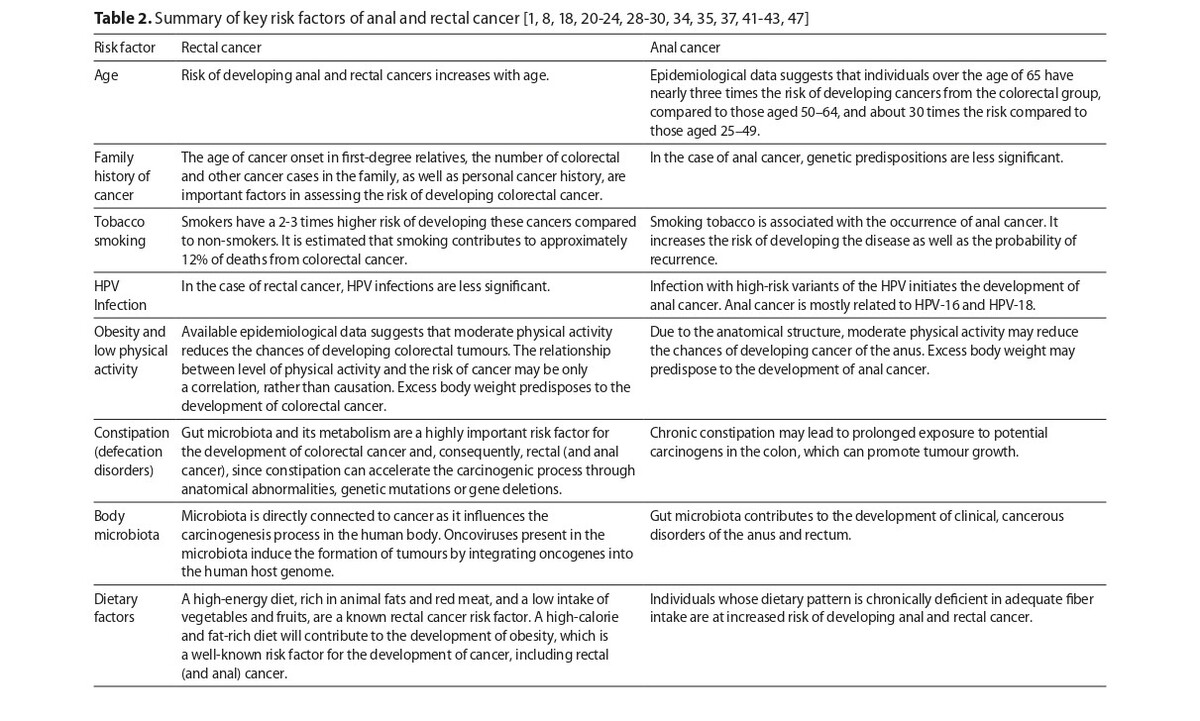
Factors that may increase the risk of developing anal or rectal cancers include age, a family history of cancer, smoking, HPV infection, obesity, low levels of physical activity, constipation, microbiota composition, and diet.
Summary:
Despite their close anatomical proximity, anal and rectal cancers are two distinct conditions that differ in terms of etiopathogenesis, risk factors, prognosis, and treatment methods. Although cancer of the anal margin and anal canal is relatively rare, when combined with rectal cancer, they pose significant health risks. However, these cancers can be prevented by a properly informed healthy lifestyle
Malignant tumours of the anus and rectum represent a serious health issue in Poland and worldwide. In Poland in 2021, malignant rectal cancers accounted for 4.1% of cases in men and 2.4% in women, while cancers of the anus and anal canal made up 0.5% of all cancers. These tumours are classified within the group of colorectal cancers (C18-C21) according to ICD-10. Globally, they are the third most common cancer in men and the second most common in women. The aim of this article is to describe selected risk factors for the development of anal and rectal cancer based on available literature
Review methods:
A literature review was conducted, focusing on articles related to anal and rectal cancer. The search was performed in two databases: Google Scholar and PubMed, using such key words as: cancer, anal cancer, rectal cancer, risk factors, HPV, microbiota, gut microbiota, constipation, fibre, obesity, physical activity, colorectal cancer. A total of 34 scientific articles from 2013–2023 were analyzed. No language restrictions were applied, and the selection of literature was made independently based on its relevance to the research topic.
Brief description of the state of knowledge:
Factors that may increase the risk of developing anal or rectal cancers include age, a family history of cancer, smoking, HPV infection, obesity, low levels of physical activity, constipation, microbiota composition, and diet.
Summary:
Despite their close anatomical proximity, anal and rectal cancers are two distinct conditions that differ in terms of etiopathogenesis, risk factors, prognosis, and treatment methods. Although cancer of the anal margin and anal canal is relatively rare, when combined with rectal cancer, they pose significant health risks. However, these cancers can be prevented by a properly informed healthy lifestyle
Szymańska M, Hanys K, Mroczek A, Kryszczyszyn-Musialik K, Kasperczyk J. Selected Risk Factors of Anal and Rectal Cancer. Med Og Nauk Zdr.
2025; 31(1): 6–12. doi: 10.26444/monz/202949
REFERENCJE (49)
1.
Freier B, Dagiel J, Więckowska B. Treatment pathway model in colorectal cancers. In: Więckowska B, editor. Medical treatment in Poland – analysis and models. Ministry of Health; 2015. p. 207–234.
2.
Didkowska JA, Wojciechowska U, Barańska K, et al. Cancer in Poland in 2021. Ministerstwo Zdrowia; 2023.
3.
Zyśk R, Wysocki P, Wyrwicz L. Colorectal cancer — the social significance of changes in the epidemiology and treatment options in poland. Oncol Clin Pract. 2014;10:212–223.
4.
Socha J, Bujko K. Carcinoma of the anal canal and anal margin. Oncol Clin Pract. 2021;16(6):331–337. https://doi.org/10.5603 OCP.2020.0036.
5.
World Health Organization. International classification of diseases 11th revision, 2022. https://icd.who.int/en (access: 2024.10.22).
6.
Wojciechowska U, Barańska K, Miklewska M, et al. Cancer incidence and mortality in Poland in 2020. Nowotwory. J Oncol. 2023;73(3):129–145. https://doi.org/10.5603/NJO.20....
8.
Gondal TA, Chaudhary N, Bajwa H, et al. Anal Cancer: The Past, Present and Future. Current Oncology. 2023;30(3):3232–3250. https:// doi.org/10.3390/curroncol30030246.
9.
Roberts JR, Siekas LL, Kaz AM. Anal intraepithelial neoplasia: A review of diagnosis and management. World J Gastrointest Oncol. 2017;9(2):50–61. https://doi.org/10.4251/wjgo.v....
10.
Brogden DRL, Walsh U, Pellino G, et al. Evaluating the efficacy of treatment options for anal intraepithelial neoplasia: a systematic review. Int J Colorectal Dis. 2020;36:213–226. https://doi.org/10.1007/s00384- 020-03740-6.
11.
Marcinkowska D, Glinkowski S, Spych M. Anal cancer – a multidisciplinary medical challenge. Diagnosis and treatment. Nowa medycyna. 2022;2:49–57. https://doi.org/10.25121/NM.20....
12.
Sasaki A, Nakajima T, Egashira H, et al. Condyloma acuminatum of the anal canal, treated with endoscopic submucosal dissection. World J Gastroenterol. 2016;22(8):2636–2641. https://doi.org/10.3748/wjg. v22.i8.2636.
13.
Kozierkiewicz A, Topór-Mądry R, Kowalczyk A, et al. Effectiveness and costs of rectal cancer therapy in Poland; a regional approach. Nowotwory. J Oncol. 2015;65(4):271–280. https://doi.org/10.5603/ NJO.2015.0056.
14.
Fernandes MC, Gollub MJ, Brown G. The importance of MRI for rectal cancer evaluation. Surgical Oncology. 2022;43:101739. https://doi.org/10.1016/j.suro....
15.
Wilkinson N. Management of Rectal Cancer. Surgical Clinics of North America. 2020;100(3):615–628. https://doi.org/10.1016 j.suc.2020.02.014.
16.
Bujko K, Potemski P, Rutkowski A, et al. Rectal cancer (C20). Oncol Clin Pract. 2021;16(6):338–357. https://doi.org/10.5603/OCP.20....
17.
Stopińska K, Mielcarska S. Najnowsze metody leczenia raka jelita grubego i odbytnicy. In: Bałabuszek K, Mroczek A, Pawlick M, editors. New diagnostic and therapeutics methods; 2019. p. 45–51.
18.
Rawla P, Sunkara T, Barsouk A. Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Gastroenterology Rev. 2019;14(2):89–103. https://doi.org/10.5114/pg.201....
19.
Goodarzi E, Beiranvand R, Naemi H, et al. Worldwide incidence and mortality of colorectal cancer and human development index (HDI): an ecological study. WCRJ. 2019;6:e1433. https://doi.org/10.32113/ wcrj_201911_1433.
20.
Sawicki T, Ruszkowska M, Danielewicz A, et al. A Review of Colorectal Cancer in Terms of Epidemiology, Risk Factors, Development, Symptoms and Diagnosis. Cancers. 2021;13(9):2025. https://doi. org/10.3390/cancers13092025.
21.
Thélin C, Sikka S. Epidemiology of Colorectal Cancer — Incidence, Lifetime Risk Factors Statistics and Temporal Trends. In: Ettarh R, editor. Screening for Colorectal Cancer with Colonoscopy. Rijeka: IntechOpen; 2015. p. 61–78. https://doi.org/10.5772/61945.
22.
Menon G, Carr S, Kasi A. Familial Adenomatous Polyposis. 2024; https://www.ncbi.nlm.nih.gov/b... (access: 2024.10.22).
23.
Sninsky JA, Shore BM, Lupu GV, Crockett SD. Risk Factors for Colorectal Polyps and Cancer. Gastrointestinal Endoscopy Clinics of North America. 2022;32(2):195–213. https://doi.org/10.1016/j.giec....
24.
Soheili M, Keyvani H, Soheili M, Nasseri S. Human papilloma virus: A review study of epidemiology, carcinogenesis, diagnostic methods, and treatment of all HPV-related cancers. Medical Journal of The Islamic Republic of Iran. 2021;35(35). https://doi.org/10.47176/mjiri....
25.
Williamson AL. Recent Developments in Human Papillomavirus (HPV) Vaccinology. Viruses. 2023;15(7):1440–1440. https://doi.org/10.3390/ v15071440.
26.
Petca A, Borislavschi A, Zvanca M, Petca RC, Sandru F, Dumitrascu M. Non-sexual HPV transmission and role of vaccination for a better future (Review). Experimental and Therapeutic Medicine. 2020;20(6):1–1. https://doi.org/10.3892/etm.20....
27.
Blomberg M, Friis S, Munk C, et al. Genital warts and risk of cancer: a Danish study of nearly 50 000 patients with genital warts. The Journal of Infectious Diseases. 2012;205(10):1544–1553. https://doi.org/10.1093/ infdis/jis228.
28.
Rosalik K, Tarney C, Han J. Human Papilloma Virus Vaccination. Viruses. 2021;13(6):1091. https://doi.org/10.3390/v13061....
29.
Łacko A. Is there a sufficient evidence to confirm that physical activity decreases cancer risk and improves outcomes? Nowotwory. J Oncol. 2016;66(3):254–257. https://doi.org/10.5603/NJO.20....
30.
Maciejewska-Cebulak M. The influence of the overweight and obesityon cancer development. Forum Med Rodzinnej. 2017;11(2):73–79.
31.
Binkowska-Borgosz I, Starzyńska T, Błogowski W. Obesity and gastrointestinal neoplasms. Postepy Hig Med Dosw (Online). 2014;68:1193–1198. https://doi.org/10.5604/173226....
32.
Daniluk J. Chronic constipation — an underestimated clinical concern. Gastroenterologia Kliniczna. Postępy i Standardy. 2018;10(1):1–13.
33.
Staller K, Olén O, Söderling J, et al. Chronic constipation as a risk factor for colorectal cancer: Results from a nationwide, case-control study. Clin Gastroenterol Hepatol. 2022;20(8):1867–1876.e2. https:// doi.org/10.1016/j.cgh.2021.10.024.
34.
Wang L-W, Ruan H, Wang B-M, et al. Microbiota regulation in constipation and colorectal cancer. World J Gastrointest Oncol. 2023;15(5):776–786. https://doi.org/10.4251/wjgo.v....
35.
Wu L, Wu H, Huang F, et al. Causal association between constipation and risk of colorectal cancer: a bidirectional two-sample mendelian randomization study. Front Oncol. 2023;13:1282066. https://doi. org/10.3389/fonc.2023.1282066.
36.
Guérin A, Mody R, Fok B, et al. Risk of developing colorectal cancer and benign colorectal neoplasm in patients with chronic constipation. Aliment Pharmacol Ther. 2014; 40(1): 83–92. https://doi.org/10.1111/ apt.12789.
37.
Yang L, Li A, Wang Y, et al. Intratumoural microbiota: roles in cancer initiation, development and therapeutic efficacy. Sig Transduct Target Ther. 2023; 8: 35. https://doi.org/10.1038/s41392....
38.
Pant A, Maiti TK, Mahajan D, et al. Human Gut Microbiota and Drug Metabolism. Microb Ecol. 2022;86:97–111. https://doi.org/10.1007/ s00248-022-02081-x.
39.
Chen Y, Zhou J, Wang L. Role and Mechanism of Gut Microbiota in Human Disease. Front Cell Infect Microbiol. 2021;11:625913. https://doi.org/10.3389/fcimb.....
40.
Garrett WS. Cancer and the microbiota. Science. 2015;348(6230):80–86. https://doi.org/10.1126/scienc....
41.
Roberts DC, Chidambaram S, Kinross JM. The role of the colonic microbiota and bile acids in colorectal cancer. Curr Opin Gastroenterol. 2021;38(2):179–188. https://doi.org/10.1097/MOG.00....
42.
Borycka-Kiciak K, Strus M, Pietrzak P, et al. Clinical and microbiological aspects of the use of lactobacillus rhamnosus PL1 strains in proctological patients with symptoms of chronic proctitis. Pol Przegl Chir. 2017;89(3): 16–22. https://doi.org/10.5604/01.300....
43.
World Cancer Research Fund International and American Institute for Cancer Research. Diet, Nutrition, Physical Activity and Cancer: a Global Perspective; A summary of the Third Expert Report 2018. https://www. wcrf.org/diet-activity-and-cancer/global-cancer-update-programme/ resources-and-toolkits/ (access: 2024.10.22).
44.
European Commission. Health Promotion and Disease Prevention Knowledge Gateway 2023. https://knowledge4policy.ec.eu... health-promotion-knowledge-gateway/dietary-fibre_en (access: 2024.10.22).
45.
Kaczmarek-Borowska B, Synoś K, Zielińska K. Preliminary reports on the impact of diet on the type of cancer. Problemy Nauk Stosowanych. 2018;8:163–176.
46.
Veettil SK, Wong TY, Loo YS, et al. Role of Diet in Colorectal Cancer Incidence: Umbrella Review of Meta-analyses of Prospective Observational Studies. JAMA Netwo Open. 2021; 4(2): e2037341– e2037341. https://doi.org/10.1001/jamane....
47.
Hu J, Wang J, Li Y, et al. Use of Dietary Fibers in Reducing the Risk of Several Cancer Types: An Umbrella Review. Nutrients. 2023;15(11):2545–3805. https://doi.org/10.3390/nu1511....
49.
Yang W, Liu L, Masugi Y, et al. Calcium intake and risk of colorectal cancer according to expression status of calcium-sensing receptor (CASR). Gut. 2017;67(8):1475–483. https://doi.org/10.1136/gutjnl....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.