Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Predyktory nieprzestrzegania zaleceń terapeutycznych w grupie pacjentów w podeszłym wieku z niewydolnością serca i zespołem kruchości przyjętych na szpitalny oddział ratunkowy
1
Emergency Department, Regional Specialist Hospital, Wrocław, Poland
2
Institute of Health Sciences, University of Opole, Poland
Autor do korespondencji
Milena Marciniak
Emergency Department, Regional Specialist Hospital, Kamieńskiego 73a, 51-124 Wrocław, Poland
Emergency Department, Regional Specialist Hospital, Kamieńskiego 73a, 51-124 Wrocław, Poland
Med Og Nauk Zdr. 2025;31(1):40-48
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Niewydolność serca (HF), będąca najczęstszym schorzeniem sercowo-naczyniowym, jest głównym wyzwaniem w starzejącym się społeczeństwie. Celem badania była analiza występowania zespołu słabości i przestrzegania zaleceń terapeutycznych u pacjentów w podeszłym wieku z HF hospitalizowanych w szpitalnym oddziale ratunkowym (SOR). Nasze badanie miało na celu w szczególności identyfikację predyktorów nieprzestrzegania zaleceń terapeutycznych w tej grupie.
Materiał i metody:
Przeprowadziliśmy ankietę wśród 110 pacjentów z niewydolnością serca hospitalizowanych w SOR-ze. Do jej skonstruowania zastosowane zostały skale Adherence in Chronic Diseases Scale (ACDS) i Tilburg Frailty Indicator (TFI).
Wyniki:
Prawie jeden na czterech pacjentów (N = 24; 21,8%) wykazywał niski poziom przestrzegania zaleceń terapeutycznych, podczas gdy 60% badanych (N = 66) przestrzegało ich w stopniu średnim. Obecność zespołu słabości zaobserwowano u ponad połowy pacjentów (N = 76; 69,1%). Im wyższy poziom słabości w sferze fizycznej, psychicznej i społecznej, tym niższy poziom przestrzegania zaleceń. Predyktory nieprzestrzegania zaleceń terapeutycznych obejmowały psychiczne komponenty słabości i liczbę hospitalizacji z powodu zaostrzeń niewydolności serca w ciągu ostatnich 2 lat. Analiza regresji wykazała, że im większe nasilenie słabości psychicznej i im większa liczba hospitalizacji, tym niższy wynik ACDS, a tym samym mniejsze przestrzeganie zaleceń dotyczących leczenia.
Wnioski:
W celu utrzymania motywacji i przestrzegania procesu leczenia pacjentom należy zapewnić wsparcie psychologiczne. Warto podkreślić rolę rodziny i lekarza rodzinnego w zapobieganiu dekompensacji HF i ponownej hospitalizacji tych pacjentów.
Niewydolność serca (HF), będąca najczęstszym schorzeniem sercowo-naczyniowym, jest głównym wyzwaniem w starzejącym się społeczeństwie. Celem badania była analiza występowania zespołu słabości i przestrzegania zaleceń terapeutycznych u pacjentów w podeszłym wieku z HF hospitalizowanych w szpitalnym oddziale ratunkowym (SOR). Nasze badanie miało na celu w szczególności identyfikację predyktorów nieprzestrzegania zaleceń terapeutycznych w tej grupie.
Materiał i metody:
Przeprowadziliśmy ankietę wśród 110 pacjentów z niewydolnością serca hospitalizowanych w SOR-ze. Do jej skonstruowania zastosowane zostały skale Adherence in Chronic Diseases Scale (ACDS) i Tilburg Frailty Indicator (TFI).
Wyniki:
Prawie jeden na czterech pacjentów (N = 24; 21,8%) wykazywał niski poziom przestrzegania zaleceń terapeutycznych, podczas gdy 60% badanych (N = 66) przestrzegało ich w stopniu średnim. Obecność zespołu słabości zaobserwowano u ponad połowy pacjentów (N = 76; 69,1%). Im wyższy poziom słabości w sferze fizycznej, psychicznej i społecznej, tym niższy poziom przestrzegania zaleceń. Predyktory nieprzestrzegania zaleceń terapeutycznych obejmowały psychiczne komponenty słabości i liczbę hospitalizacji z powodu zaostrzeń niewydolności serca w ciągu ostatnich 2 lat. Analiza regresji wykazała, że im większe nasilenie słabości psychicznej i im większa liczba hospitalizacji, tym niższy wynik ACDS, a tym samym mniejsze przestrzeganie zaleceń dotyczących leczenia.
Wnioski:
W celu utrzymania motywacji i przestrzegania procesu leczenia pacjentom należy zapewnić wsparcie psychologiczne. Warto podkreślić rolę rodziny i lekarza rodzinnego w zapobieganiu dekompensacji HF i ponownej hospitalizacji tych pacjentów.
Introduction and objective:
Heart failure (HF), the most common cardiovascular condition, is a major challenge in an aging society. The aim of the study was to analyze the occurrence of frailty syndrome and adherence to therapeutic recommendations in elderly patients with HF hospitalized in a hospital emergency department (ED). The study also aimed to identify predictors of non-adherence to treatment recommendations in this group.
Material and methods:
110 heart failure patients hospitalized in ED were surveyed. The Adherence in Chronic Diseases Scale (ACDS) scale and the Tilburg Frailty Indicator (TFI) were used.
Results:
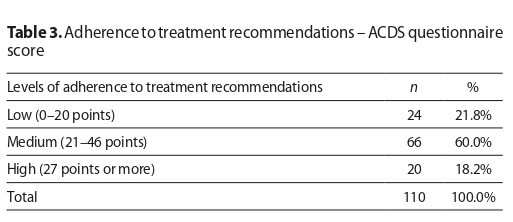
Almost one in 4 patients (n=24; 21.8%) demonstrated low adherence to the prescribed treatment recommendations, while 60% of subjects (n=66) showed intermediate levels of adherence. The presence of frailty syndrome was observed in more than half of the patients (n=76; 69.1%). The higher the levels of frailty in the physical, psychological and social domains, the lower the level of treatment adherence. The predictors of non-adherence to treatment recommendations included the psychological components of frailty and the number of hospitalizations for heart failure exacerbations in the past 2 years. Regression analysis shows that the greater the severity of psychological frailty and the greater the number of hospitalizations, the lower the ACDS score, and thus the worse the adherence to treatment recommendations.
Conclusions:
Psychological support should be provided to patients to maintain motivation and adherence to the treatment process. The role of the family and family physician in the prevention of HF decompensation and rehospitalization of these patients should be emphasized.
Heart failure (HF), the most common cardiovascular condition, is a major challenge in an aging society. The aim of the study was to analyze the occurrence of frailty syndrome and adherence to therapeutic recommendations in elderly patients with HF hospitalized in a hospital emergency department (ED). The study also aimed to identify predictors of non-adherence to treatment recommendations in this group.
Material and methods:
110 heart failure patients hospitalized in ED were surveyed. The Adherence in Chronic Diseases Scale (ACDS) scale and the Tilburg Frailty Indicator (TFI) were used.
Results:
Almost one in 4 patients (n=24; 21.8%) demonstrated low adherence to the prescribed treatment recommendations, while 60% of subjects (n=66) showed intermediate levels of adherence. The presence of frailty syndrome was observed in more than half of the patients (n=76; 69.1%). The higher the levels of frailty in the physical, psychological and social domains, the lower the level of treatment adherence. The predictors of non-adherence to treatment recommendations included the psychological components of frailty and the number of hospitalizations for heart failure exacerbations in the past 2 years. Regression analysis shows that the greater the severity of psychological frailty and the greater the number of hospitalizations, the lower the ACDS score, and thus the worse the adherence to treatment recommendations.
Conclusions:
Psychological support should be provided to patients to maintain motivation and adherence to the treatment process. The role of the family and family physician in the prevention of HF decompensation and rehospitalization of these patients should be emphasized.
Marciniak M, Szwamel K. Predictors of non-adherence to treatment recommendations in a group of elderly patients with heart failure and
frailty syndrome admitted to an emergency department. Med Og Nauk Zdr. 2025; 31(1): 40–48. doi: 10.26444/monz/202527
REFERENCJE (26)
1.
Bartolik K, Bukowski H, Czech M, et al. Heart failure in Poland. Realities, costs, suggestions for improvement. Institute for Responsible Innovation, 2020.
2.
Nessler J, Krawczyk K, Leszek P, et al. Expert opinion of the Heart Failure Association of the Polish Society of Cardiology, the College of Family Physicians in Poland, and the Polish Society of Family Medicine on the peri discharge management of patients with heart failure. Kardiol Pol. 2023;81(7–8):824–844. https://doi.org/10.33963/kp.a2....
3.
Lelonek M. Heart failure – perioperative period key to management. Folia Cardiol. 2018;13(4):371–377. https://doi.org/10.5603/FC.201....
4.
Lelonek M, Pawlak A, Nessler J, et al. Heart Failure in Poland 2014–2021. Heart Failure Assoc Polish Society Cardiol. 2023.
5.
Jankowska-Polańska B, Uchmanowicz I. Adherence to treatment recommendations in heart failure. Heart Vascular Dis. 2016;13(3):227–234.
6.
Denfeld QE, Winters-Stone K, Mudd JO, et al. The prevalence of frailty in heart failure: a systematic review and meta-analysis. Int J Cardiol. 2017;236:283–289. https://doi.org/10.1016/j.ijca....
7.
Brigola AG, Rossetti ES, Santos BRD, et al. Relationship between cognition and frailty in elderly: A systematic review. Dement Neuropsychol. 2015;9(2):110–119. https://doi.org/10.1590/1980-5....
8.
Park C, Ko FC. The Science of Frailty: Sex Differences. Clin Geriatr Med. 2021;37(4):625–638 https://doi.org/10.1016/j.cger....
9.
Talha KM, Pandey A, Fudim M, et al. Frailty and heart failure: State-of-the-art review. J Cachexia Sarcopenia Muscle. 2023;14(5):1959–1972. https://doi.org/10.1002/jcsm.1....
10.
Pandey A, Kitzman D, Reeves G. Frailty Is Intertwined With Heart Failure: Mechanisms, Prevalence, Prognosis, Assessment, and Management. JACC: Heart Fail. 2019;7(12):1001–1011. https://doi.org/10.1016/j.jchf....
11.
Sobczyńska M, Główczyńska R, Opolski G. Frailty syndrome increases frequency of complications in patients undergoing invasive cardiology procedures and open-heart surgeries. Folia Cardiol. 2017;12(6):557–564. https://doi.org/10.5603/FC.201....
12.
Aggarwal B, Pender A, Mosca L, et al. Factors associated with medication adherence among heart failure patients and their caregivers. J Nurs Educ Pract. 2015;5(3):22–27. https://doi.org/10.5430/jnep.v....
13.
Wu JR, Moser DK. Medication Adherence Mediates the Relationship Between Heart Failure Symptoms and Cardiac Event-Free Survival in Patients with Heart Failure. J Cardiovasc Nurs. 2018;33(1):40–46. https://doi.org/10.1097/JCN.00....
14.
Ruppar TM, Cooper PS, Mehr DR, et al. Medication Adherence Interventions Improve Heart Failure Mortality and Readmission Rates: Systematic Review and Meta-Analysis of Controlled Trials. J Am Heart Assoc. 2016;5(6):e002606. https://doi.org/10.1161/JAHA.1....
15.
Kubica A, Kosobucka A, Michalski P, et al. Adherence in Chronic Diseases Scale — a new tool to monitor implementation of a treatment plan. Folia Cardiol. 2017;12(1):19–26. https://doi.org/10.5603/FC.a20....
16.
Uchmanowicz I, Jankowska-Polańska B, Uchmanowicz B, et al. Validity and Reliability of the Polish Version of the Tilburg Frailty Indicator (TFI). J Frailty Aging. 2016;5(1):27–32 http://dx.doi.org/10.14283/jfa....
17.
Gaciong Z, Kardas P. Therapeutic nonadherence: from causes to practical solutions: a handbook for physicians and medical students. Polpharma Scientific Foundation: Index Copernicus International, 2015.
18.
Dewan P, Jackson A, Jhund PS, et al. The prevalence and importance of frailty in heart failure with reduced ejection fraction – an analysis of PARADIGM-HF and ATMOSPHERE. Eur J Heart Fail. 2020;22(11):2123–2133. https://doi.org/10.1002/ejhf.1....
19.
Davis MR, Lee CS, Corcoran A, et al. Gender differences in the prevalence of frailty in heart failure: A systematic review and meta-analysis. Int J Cardiol. 2021;333:133–140. https://doi.org/10.1016/j.ijca....
20.
Jankowska-Polańska B, Dudek K, Szymanska-Chabowska A, et al. The influence of frailty syndrome on medication adherence among elderly patients with hypertension. Clin Interv Aging. 2016;11:1781–1790. https://doi.org/10.2147/CIA.S1....
21.
Conforto R, Rizzo V, Russo R, Mazza E, Maurotti S, Pujia C, Succurro E, Arturi F, Ferro Y, Sciacqua A, Pujia A, Montalcini T. Advances in body composition and gender differences in susceptibility to frailty syndrome: Role of osteosarcopenic obesity. Metabolism. 2024;161:156052. https://doi.org/10.1016/j.meta....
22.
Taguchi CK, Menezes PL, Melo ACS, Santana LS, Conceição WRS, Souza GF, Araújo BCL, Silva ARD. Frailty syndrome and risks for falling in the elderly community. Codas. 2022;34(6):20210025. https://doi.org/10.1590/2317–1....
23.
Bonikowska I, Szwamel K, Uchmanowicz I. Adherence to Medication in Older Adults with Type 2 Diabetes Living in Lubuskie Voivodeship in Poland: Association with Frailty Syndrome. J Clin Med. 2022;11(6):1707. https://doi.org/10.3390/jcm110....
24.
Hood SR, Giazzon AJ, Seamon G, et al. Association Between Medication Adherence and the Outcomes of Heart Failure. Pharmacotherapy. 2018;38(5):539–545. https://doi.org/10.1002/phar.2....
25.
Poletti V, Pagnini F, Banfi P, et al. The Role of Depression on Treatment Adherence in Patients with Heart Failure–a Systematic Review of the Literature. Curr Cardiol Rep. 2022;24(12):1995–2008. https://doi.org/10.1007/s11886....
26.
Jankowska-Polańska B, Kuśnierz M, Dudek K, et al. Impact Of Cognitive Function On Compliance With Treatment In Heart Failure. J Educ Health Sport. 2017;7(2):392–420. http://dx.doi.org/10.5281/zeno....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.