RESEARCH PAPER
Stress level among patients with cervical spine pain
1
Instytut Nauk o Zdrowiu, Katedra Rehabilitacji i Odnowy Biologicznej, Uniwersytet Pomorski w Słupsku, Polska
Corresponding author
Jakub Pawłowski
Instytut Nauk o Zdrowiu, Katedra Rehabilitacji i Odnowy Biologicznej, Uniwersytet Pomorski w Słupsku, Arciszewskiego 22A, 76-200, Słupsk
Instytut Nauk o Zdrowiu, Katedra Rehabilitacji i Odnowy Biologicznej, Uniwersytet Pomorski w Słupsku, Arciszewskiego 22A, 76-200, Słupsk
Med Og Nauk Zdr. 2024;30(3):247-251
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Stress can have a significant impact on pain experiences. The body’s physiological stress response is manifested by an increase in muscle tension, which in a long-term process may lead to tension-type dysfunctions in the muscles and the osteoarticular system. Long-term emotional stress can, over time, lead to anxiety and depression, and even trigger autoimmune diseases. That is why it is so important to understand this correlation, which may allow taking preventive measures to control emotional stress and reduce the feeling of pain in the cervical region, thereby improving own well-being. The aim of the study is to assess the level of stress in patients with cervical spine pain.
Material and methods:
The study included 100 patients with cervical spine pain from the Pomeranian Voivodeship. A selfadministered questionnaire, the Visual Analogue Scale (VAS), and the Perceived Stress Scale (PSS) were used as research tools.
Results:
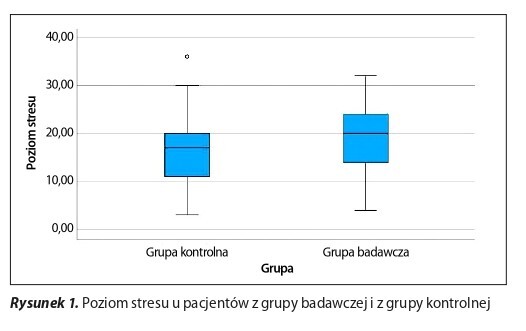
Patients declaring pain in the cervical spine (n = 100) were characterised by significantly higher levels of stress, compared to patients in the control group without pain (n = 64). In addition, 48.78% (n = 80) of respondents declaring to have a comorbid condition were characterised by significantly higher stress intensity, compared to 51.22% (n = 84) of those without comorbid conditions.
Conclusions:
The level of perceived stress is associated with increased cervical spine pain and having comorbidities; therefore a multidisciplinary and holistic approach should be expected in the treatment of this type of patient.
Stress can have a significant impact on pain experiences. The body’s physiological stress response is manifested by an increase in muscle tension, which in a long-term process may lead to tension-type dysfunctions in the muscles and the osteoarticular system. Long-term emotional stress can, over time, lead to anxiety and depression, and even trigger autoimmune diseases. That is why it is so important to understand this correlation, which may allow taking preventive measures to control emotional stress and reduce the feeling of pain in the cervical region, thereby improving own well-being. The aim of the study is to assess the level of stress in patients with cervical spine pain.
Material and methods:
The study included 100 patients with cervical spine pain from the Pomeranian Voivodeship. A selfadministered questionnaire, the Visual Analogue Scale (VAS), and the Perceived Stress Scale (PSS) were used as research tools.
Results:
Patients declaring pain in the cervical spine (n = 100) were characterised by significantly higher levels of stress, compared to patients in the control group without pain (n = 64). In addition, 48.78% (n = 80) of respondents declaring to have a comorbid condition were characterised by significantly higher stress intensity, compared to 51.22% (n = 84) of those without comorbid conditions.
Conclusions:
The level of perceived stress is associated with increased cervical spine pain and having comorbidities; therefore a multidisciplinary and holistic approach should be expected in the treatment of this type of patient.
REFERENCES (14)
1.
Kalkowski K. Wpływ umysłu na zdrowie i ciało, czyli psychosomatyka i radzenie sobie ze stresem. Tutoring Gedanensis. 2021;6(1):5–12.
2.
Cooper CL, Campbell Quick J. The Handbook of stress and Health: A Guide to Research and Practice. 1st Ed. John Wiley & Sons, Ltd. Wiley Blackwell, United Kingdom; 2017. p. 210–211.
3.
Abdallah C, Geha P. Chronic Pain and Chronic Stress: Two Sides of the Same Coin?. Chronic Stress (Thousand Oaks). 2017; 1: 1–10.
4.
Spector A, Quinn K, Wang I, Gliedt J, Fillingim R, Cruz-Almeida Y. More Problems, More Pain: The Role of chronic Life Stressors and Racial/Ethnic Identity on Chronic Pain Among Middle-Aged and Older Adults in the United States. Chronic Stress (Thousand Oaks). 2023; 7: 1–10.
6.
Rakowski A. Terapia manualna holistyczna. Centrum Terapii Manualnej. Poznań, 2023.
7.
Szpala M, Skorupińska A, Kostorz K. Występowanie zespołów bólowych kręgosłupa – przyczyny i leczenie. Pomeranian J Life Sci. 2017;63 (3): 78.
8.
Toman M, Rutkowska M, Dąbrowska-Galas M, Król T, Michalik P, Michalski T. Dolegliwości bólowe odcinka szyjnego kręgosłupa wśród studentów fizjoterapii. Pol Prz Nauk Zdr. 2019; 2(59): 109–110.
10.
Finkelstein J. Neck and Arm Pain and Related Symptoms. Cervical Spine Disorders. The Workplace Safety and Insurance Appeals Tribunal. https://www.wsiat.on.ca/en/Med.... (dostęp 2024.04.01).
11.
Rąglewska P, Dembiński J, Straburzyńska-Lupa A. Psychosomatic background of cervical spine pain assessed during the Covid-19 pandemic period. Res Physiother Rev. 2023; 27(2): 31–39.
12.
Ahmad A, Zakaria R. Pain in Times of Stress. Malays J Med Sci. 2015; 22 (Dec): 52–61.
13.
Stephen S, Brand C, Olivier B. Neck pain and disability: are they related to dysfunctional breathing and stress? Physiother Can. 2021; 20;74(2): 158–164 https://doi.org/10.3138%2Fptc-..., https://pubmed.ncbi.nlm.nih.go....
14.
Ortego G, Villafañe JH, Doménech- García V, Berjano P, Bertozzi L, Herrero PJ. Is there a relatioship between psychological stress or anxiety and chronic nonspecific neck-arm pain in adults? A systematic review and meta-analysis. 2016;90(Nov): 70–81.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.