RESEARCH PAPER
Polish doctors concerning the phenomenon of second victims. Pilot study among doctors during specialization training
1
Department of Medical Law and Medical Jurisprudence, School of Public Health, Medical Centre for Postgraduate Education, Warsaw, Poland
2
Department of Medical Communication, School of Public Health, Medical Center for Postgraduate Education, Warsaw, Poland
3
Poradnia Rehabilitacyjna,, 22 Wojskowy Szpital Uzdrowiskowo-Rehabilitacyjny, Ciechocinek, Polska
Corresponding author
Iwona Wrześniewska - Wal
Department of Medical Law and Medical Jurisprudence, School of Public Health, Medical Centre for Postgraduate Education, Warsaw, Poland
Department of Medical Law and Medical Jurisprudence, School of Public Health, Medical Centre for Postgraduate Education, Warsaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
A physician who is directly or indirectly involved in an adverse patient event, an unintentional error, or a patient injury, becomes a second victim (SV) and strongly experiences various negative psychological and psychosomatic symptoms. The aim of the study was to analyze the perception of SV by young physicians in Poland.
Material and methods:
A cross-sectional survey was conducted among physicians and dentists pursuing specialty training at the School of Public Health of the Medical Centre for Postgraduate Education in Warsaw, Poland, between March – April 2024. A total of 123 physicians participated in the survey who represented more than 40 medical specialties in various regions of Poland.
Results:
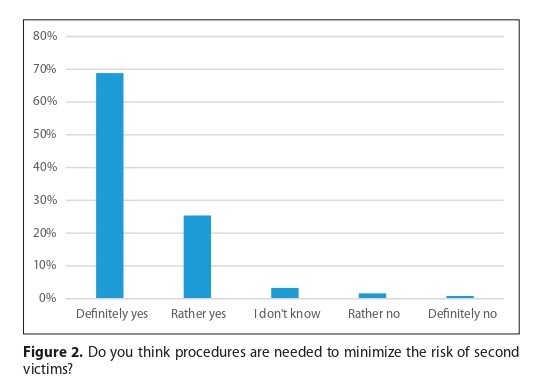
As many as 30% of the physicians felt that there is no room for error in modern medicine. Respondents had no doubt that the implementation of appropriate procedures to minimize risks is necessary (95%). At the same time, 62% of young physicians confirmed that they, or one of their colleagues, had been a second victim. In Poland, no care is provided for SVs (46%). According to those surveyed, a physician who has made a mistake needs legal care (98%) as well as psychological care (83%).The majority of respondents (92%) felt that training on SV was essential.
Conclusions:
Building a culture of safety takes time. Legal and psychological care should be organized in parallel, as should training for medical staff and managers. However, the attitude of the infallibility of young doctors may make it difficult for managers to find an effective tool to support psychological care.
A physician who is directly or indirectly involved in an adverse patient event, an unintentional error, or a patient injury, becomes a second victim (SV) and strongly experiences various negative psychological and psychosomatic symptoms. The aim of the study was to analyze the perception of SV by young physicians in Poland.
Material and methods:
A cross-sectional survey was conducted among physicians and dentists pursuing specialty training at the School of Public Health of the Medical Centre for Postgraduate Education in Warsaw, Poland, between March – April 2024. A total of 123 physicians participated in the survey who represented more than 40 medical specialties in various regions of Poland.
Results:
As many as 30% of the physicians felt that there is no room for error in modern medicine. Respondents had no doubt that the implementation of appropriate procedures to minimize risks is necessary (95%). At the same time, 62% of young physicians confirmed that they, or one of their colleagues, had been a second victim. In Poland, no care is provided for SVs (46%). According to those surveyed, a physician who has made a mistake needs legal care (98%) as well as psychological care (83%).The majority of respondents (92%) felt that training on SV was essential.
Conclusions:
Building a culture of safety takes time. Legal and psychological care should be organized in parallel, as should training for medical staff and managers. However, the attitude of the infallibility of young doctors may make it difficult for managers to find an effective tool to support psychological care.
REFERENCES (32)
2.
Sari AA, Doshmangir L, Sheldon T. A systematic review of the extent, nature, and likely causes of preventable adverse events arising from hospital care. Iran J Public Health. 2010;39(3):1–15.
4.
Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the Healthcare provider “second victim” after adverse patient events. Qual Saf Heal Care. 2009;18:325–30.
5.
Vanhaecht K, Seys D, Russotto S, Strametz R, Mira J, Sigurgeirsdóttir S, Wu AW, et al. An Evidence and Consensus-Based Definition of Second Victim: A Strategic Topic in Healthcare Quality, Patient Safety, Person-Centeredness and Human Resource Management. IJERPH. 2022;19(24):1–10.
6.
Towards Zero Patient Harm in Health Care. Global-Patient-Safety-Action-Plan 2021 – 2030. First Draft August 2020, WHO. https://www.who.int/docs/defau... (accessed: 2025 January 25).
7.
De Bienassis K, Slawomirski L, Klazinga N. The economics of patient safety Part IV: Safety in the workplace. Health Working Paper OECD. https://www.oecd.org/en/public... (accessed: 2025 January 20).
8.
Action against Medical Accidents. A vision of what a “just culture” should look like for patients and healthcare staff. January 2021. AvMA. https://www.avma.org.uk/wp-con... (accessed: 2025 January 20).
9.
A just culture guide. NHS England website https://www.england.nhs.uk/pat... (accessed: 2025 January 20).
10.
Walsh P. What is a “just culture”? Journal of Patient Safety and Risk Management. 2019;24:5–6.
11.
Act of 16 June 2023 on quality in health care and patient safety (Journal of Laws 2023, item 1692, as amended).
12.
Marek Z. Plac-Bobula E. Classifications of medical error. Arch Med Sąd Kryminol. 1994;XLIV(2):197–201.
13.
Centre for Medical Postgraduate Education. Warsaw 2024. https://www.cmkp.edu.pl/akredy... (access 2025 January 20).
14.
Mira JJ, Carrillo I, Lorenzo S, et al. The aftermath of adverse events in Spanish primary care and hospital health professionals. BMC Health Serv Res. 2015;15:151.
15.
Kerkman T, Dijksman LM, Baas MAM, et al. Traumatic Experiences and the Midwifery Profession: A Cross-Sectional Study Among Dutch Midwives. Journal of Midwifery & Women’s Health. 2019;64:435–442.
16.
Shanafelt TD. Special Report: Suicidal Ideation Among American Surgeons. Arch Surg. 2011;146:54.
17.
Baas MAM, Scheepstra KWF, Stramrood CAI, et al. Work-related adverse events leaving their mark: a cross-sectional study among Dutch gynecologists. BMC Psychiatry. 2018;18:73.
18.
Burlison JD, Scott SD, Browne EK, Thompson SG, Hoffman JM. The Second Victim Experience and Support Tool: Validation of an Organizational Resource for Assessing Second Victim Effects and the Quality of Support Resources. J Patient Saf. 2017 Jun;13(2):93–102.
19.
Edrees H, Connors C, Paine L, et al. Implementing the RISE second victim support program at the Johns Hopkins Hospital: a case study. BMJ Open. 2016;6:e011708.
20.
Knudsen T, Abrahamsen C, Jørgensen JS, Schrøder K. Validation of the Danish version of the Second Victim Experience and Support Tool. Scand J Public Health. 2022;50:497–506.
21.
Scarpis E, Castriotta L, Ruscio E, et al. The Second Victim Experience and Support Tool: A Cross-Cultural Adaptation and Psychometric Evaluation in Italy (IT-SVEST). J Patient Saf. 2022;18:88–93.
22.
Koca A, Elhan AH, Genç S, et al. Validation of the Turkish version of the second victim experience and Support Tool (T-SVEST). Heliyon. 2022;8:e10553.
23.
Yan L, Tan J, Chen H, et al. Experience and support of Chinese healthcare professionals as second victims of patient safety incidents: A cross-sectional study. Perspect Psychiatr Care. 2022;58:733–743.
24.
Naya K, Aikawa G, Ouchi A, Ikeda M, Fukushima A, Yamada S, et al. Second victim syndrome in intensive care unit healthcare workers: A systematic review and meta-analysis on types, prevalence, risk factors, and recovery time. PLoS ONE. 2023:18(10):e0292108.
25.
Edrees HH, Morlock L, Wu AW. Do Hospitals Support Second Victims? Collective Insights From Patient Safety Leaders in Maryland. Jt Comm J Qual Patient Saf. 2017;43:471–483.
26.
Vento S, Cainelli F, Vallone A. Defensive medicine: It is time to slow down an epidemic finally. WJCC, 2018;6(11):406–409.
27.
Ozeke O, Ozeke V, Coskun O, Budakoglu II. Second victims in health care: current perspectives. AMEP. 2019;10:593–603.
28.
Plews-Ogan M, May N, Owens J, et al. Wisdom in Medicine: What Helps Physicians After a Medical Error? Acad Med. 2016;91:233–241.
29.
Busch IM, Moretti F, Campagna I, et al. Promoting the Psychological Well-Being of Healthcare Providers Facing the Burden of Adverse Events: A Systematic Review of Second Victim Support Resources. Int J Environ Res Public Health. 2021;18.
30.
Buhlmann M, Ewens B, Rashidi A. Moving on after critical incidents in health care: A qualitative study of the perspectives and experiences of second victims. J Adv Nurs. 2022;78:2960–2972.
31.
Scott SD, McCoig MM. Care at the point of impact: Insights into the second-victim experience. J Healthc Risk Manag. 2016;35(4):6–13.
32.
Wrześniewska-Wal I, Łuków P, Ruiz M, Zgliczyński W. How to reduce claims costs? New quality in health care. 8 December 2022 Warsaw Public Health Congress.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.