Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Aktywność fizyczna i jakość snu wśród studentów Uniwersytetu Medycznego we Wrocławiu
1
Department of Physical Education and Sport, Medical University, Wrocław, Poland
2
University of Life Sciences, Institute of Economics and Finance, Warsaw, Poland
3
Department of Econometrics and Statistics, Warsaw University of Life Sciences, Institute of Economics and Finance,
Warsaw, Poland
4
Faculty of Agriculture and Economics, University of Agriculture, Kraków, Poland
Autor do korespondencji
Michał Roman
Szkoła Główna Gospodarstwa Wiejskiego w Warszawie, Nowoursynowska 166, 02-787, Warszawa, Polska
Szkoła Główna Gospodarstwa Wiejskiego w Warszawie, Nowoursynowska 166, 02-787, Warszawa, Polska
Med Og Nauk Zdr. 2023;29(4):309-315
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Cel:
Celem artykułu było przedstawienie aktywności fizycznej i jakości snu wśród ankietowanych respondentów z Polski.
Materiał i metody:
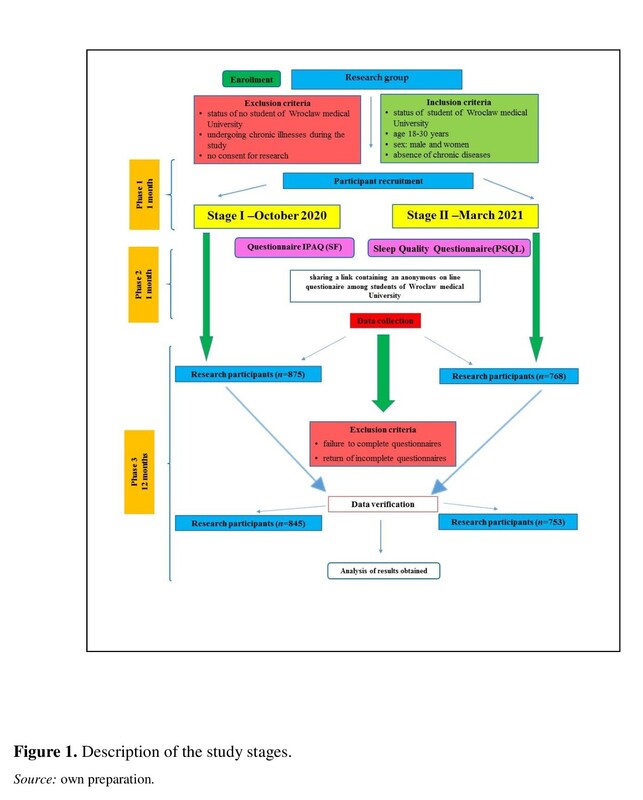
W badaniach udział wzięli studenci Uniwersytetu Medycznego we Wrocławiu. Respondenci zostali wybrani losowo, a w analizie wykorzystano wszystkie zebrane dane. Wykorzystano przygotowaną ankietę, opartą na Międzynarodowym Kwestionariuszu Aktywności Fizycznej (IPAQ). Dane zbierano w 2020 roku (przed pandemią Covid) i w 2021 roku (rok później).
Wyniki:
Badanie przeprowadzono w grupie 1600 dorosłych studentów Uniwersytetu Medycznego we Wrocławiu w okresie październik 2020 – marzec 2021. Uczestnicy odbywali obowiązkowe zajęcia zdalne z wychowania fizycznego w roku akademickim 2020–2021.
Wnioski:
Badane osoby odbywały w roku akademickim 2020/2021 obowiązkowe zajęcia zdalne z wychowania fizycznego. Pomimo ograniczeń związanych z właściwym doborem metod czy respondentów, stwierdza się, że przedstawiony temat zasługuje na dalsze badania empiryczne przez naukowców w zakresie aktywności fizycznej, jakości snu i odpoczynku. Zdaniem autorów artykułu, przedstawione zagadnienia są istotne. Ważne jest również omówienie ograniczeń badania, które czytelnicy powinni wziąć pod uwagę przy ocenie jego wyników. Ograniczeniem badań jest sama analiza, która koncentruje się na rodzaju zastosowanych metod, zakresie badań i ogólnie na trendach badawczych. Kolejnym ograniczeniem jest odpowiedni dobór respondentów w czasie pandemii Covid-19. Pomimo ograniczeń związanych z właściwym doborem metod czy respondentów, stwierdza się, że przedstawiony temat zasługuje na dalsze badania empiryczne przez naukowców w zakresie aktywności fizycznej, jakości snu i odpoczynku. W przyszłości warto przeprowadzić podobne badania dotyczące jakości snu i odpoczynku na większej próbie badawczej. Badania należy przeprowadzić nie tylko w Polsce, ale także w innych krajach (analiza porównawcza).
Celem artykułu było przedstawienie aktywności fizycznej i jakości snu wśród ankietowanych respondentów z Polski.
Materiał i metody:
W badaniach udział wzięli studenci Uniwersytetu Medycznego we Wrocławiu. Respondenci zostali wybrani losowo, a w analizie wykorzystano wszystkie zebrane dane. Wykorzystano przygotowaną ankietę, opartą na Międzynarodowym Kwestionariuszu Aktywności Fizycznej (IPAQ). Dane zbierano w 2020 roku (przed pandemią Covid) i w 2021 roku (rok później).
Wyniki:
Badanie przeprowadzono w grupie 1600 dorosłych studentów Uniwersytetu Medycznego we Wrocławiu w okresie październik 2020 – marzec 2021. Uczestnicy odbywali obowiązkowe zajęcia zdalne z wychowania fizycznego w roku akademickim 2020–2021.
Wnioski:
Badane osoby odbywały w roku akademickim 2020/2021 obowiązkowe zajęcia zdalne z wychowania fizycznego. Pomimo ograniczeń związanych z właściwym doborem metod czy respondentów, stwierdza się, że przedstawiony temat zasługuje na dalsze badania empiryczne przez naukowców w zakresie aktywności fizycznej, jakości snu i odpoczynku. Zdaniem autorów artykułu, przedstawione zagadnienia są istotne. Ważne jest również omówienie ograniczeń badania, które czytelnicy powinni wziąć pod uwagę przy ocenie jego wyników. Ograniczeniem badań jest sama analiza, która koncentruje się na rodzaju zastosowanych metod, zakresie badań i ogólnie na trendach badawczych. Kolejnym ograniczeniem jest odpowiedni dobór respondentów w czasie pandemii Covid-19. Pomimo ograniczeń związanych z właściwym doborem metod czy respondentów, stwierdza się, że przedstawiony temat zasługuje na dalsze badania empiryczne przez naukowców w zakresie aktywności fizycznej, jakości snu i odpoczynku. W przyszłości warto przeprowadzić podobne badania dotyczące jakości snu i odpoczynku na większej próbie badawczej. Badania należy przeprowadzić nie tylko w Polsce, ale także w innych krajach (analiza porównawcza).
Objective:
The aim of the article was to present physical activity and sleep quality among the surveyed respondents from Poland.
Material and methods:
Students of the Medical University of Wrocław participated in the research. The respondents were selected randomly and all collected records were used in the analysis. A prepared questionnaire was used, based on the International Physical Activity Questionnaire (IPAQ). Data was collected in 2020 (before the COVID pandemic) and in 2021 (a year later).
Results:
The study was conducted in a group of 1,600 adult students at Wrocław Medical University between October 2020 – March 2021. The participants were pursuing mandatory remote classes in physical education in the academic year 2020–2021.
Conclusions:
The surveyed individuals were pursuing mandatory remote classes in physical education in the academic year 2020/2021. Despite the limitations related to the correct selection of methods or respondents, it is argued that the presented topic deserves further empirical research by scientists in the field of physical activity, sleep quality, and rest. According to the authors of the article, the presented issues are of importance. It is also important to discuss the limitations of the study, which readers should consider when evaluating its results. The limitation of the research is the analysis itself, that focuses on the type of methods used, scope of the research, and research trends in general. Another limitation is the appropriate selection of respondents during the COVID-19 pandemic. Despite the limitations related to the correct selection of methods or respondents, it is argued that the presented topic deserves further empirical research by scientists in the field of physical activity, sleep quality, and rest. In the future, it is worth conducting similar research on the quality of sleep and rest on a larger research sample. The research should be carried out not only in Poland, but also in other countries (comparative analysis).
The aim of the article was to present physical activity and sleep quality among the surveyed respondents from Poland.
Material and methods:
Students of the Medical University of Wrocław participated in the research. The respondents were selected randomly and all collected records were used in the analysis. A prepared questionnaire was used, based on the International Physical Activity Questionnaire (IPAQ). Data was collected in 2020 (before the COVID pandemic) and in 2021 (a year later).
Results:
The study was conducted in a group of 1,600 adult students at Wrocław Medical University between October 2020 – March 2021. The participants were pursuing mandatory remote classes in physical education in the academic year 2020–2021.
Conclusions:
The surveyed individuals were pursuing mandatory remote classes in physical education in the academic year 2020/2021. Despite the limitations related to the correct selection of methods or respondents, it is argued that the presented topic deserves further empirical research by scientists in the field of physical activity, sleep quality, and rest. According to the authors of the article, the presented issues are of importance. It is also important to discuss the limitations of the study, which readers should consider when evaluating its results. The limitation of the research is the analysis itself, that focuses on the type of methods used, scope of the research, and research trends in general. Another limitation is the appropriate selection of respondents during the COVID-19 pandemic. Despite the limitations related to the correct selection of methods or respondents, it is argued that the presented topic deserves further empirical research by scientists in the field of physical activity, sleep quality, and rest. In the future, it is worth conducting similar research on the quality of sleep and rest on a larger research sample. The research should be carried out not only in Poland, but also in other countries (comparative analysis).
Kosendiak A, Roman M, Gostkowski M, Niedziółka A. Physical Activity and Sleep Quality among Medical University Students. Med Og Nauk
Zdr. 2023; 29(4): 309–315. doi: 10.26444/monz/172587
REFERENCJE (25)
1.
EU Working Group “Sport and Health” EU Physical Activity Guidelines; 2008. Available at: http://ec.europa.eu/sport/what..._ 4th_consolidated_draft_en.pdf (access: 2022.07.21).
2.
U.S Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Available at: http://www.health.gov/ PAGuidelines/ pdf/paguide.pdf (access: 2022.07.21).
3.
World Health Organization: Global recommendations on physical activity for health 2010 http://whqlibdoc.who.int/ publications/2010/9789241599979_eng.pdf/ (access: 2022.07.21).
4.
Plewa M, Markiewicz A. Aktywność fizyczna w profilaktyce i leczeniu otyłości. Endokrynol. Otył. Zab. Przem. Mat. 2006;2(1):30–37. https://journals.viamedica.pl/....
5.
López-Moreno M, Iglesias López MT, Miguel M, Garcés-Rimón M, Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients 2020;12:1–17. http://doi:10.3390/nu12113445.
6.
Luciano F, Cennachi V, Vegro V, Gaspare P. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. European Journal of Sport Science 2021;21,10:1458–1468. http://doi:10.1080/17461391.20....
7.
Idrissi AJ, Lamkaddem A, Benouajjit A, El Bouaazzaoui MB, El Houari F, Alami M, Labyad S, Chahidi A, Benjelloun M, Rabhi S, Kissani N, Zarhbouch B, Ouazzani R, Kadiri F, Alouane R, Elbiaze M, Boujraf S, El Fakir S, Souirti Z, Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Medicine. 2020;74:248–253. http://doi:10.1016/j.sleep.202....
8.
Saguem BN, Nakhli J, Romdhane I, Nasr SB, Predictors of sleep quality in medical students during COVID-19 confinement. L Encéphale. 2021;48:3–12. http://doi:10.1016/j.encep.202....
9.
McDonough DJ, Helgeson MA, Liu W, Gao Z. Effects of a remote, You Tube-delivered exercise intervention on young adults’ physical activity, sedentary behaviour, and sleep during the COVID-19 pandemic: Randomized controlled trial. Journal of Sport and Health Science. 2021;11:145–156. http://doi:10.1016/j.jshs.2021....
10.
Mahfouz MS, Ali SA, Bahari AY, Ajeebi RE, Sabei HJ, Somaily SY, Madkhali YA, Hrooby RH, Shook RN, Association Between Sleep Quality and Physical Activity in Saudi Arabian University Students. Nature and Science of Sleep. 2020;12:775–782. http://doi:10.2147/NSS.S267996.
11.
Bagci Bosi TA, Kanadiking A, Somyürek E, Gerçek G, Tarnikulu HB, Öntaş E, Uzun S. Impact of COVID-19 on eating habits, sleeping behaviour and physical activity status of final-year medical students in Ankara, Turkey. Public Health Nutrition. 2021;9:1–8. http://doi:10.1017/ S1368980021003906.
12.
Mishra J, Panigrahi A, Samanta P, Dash K, Mahapatra P, Beherta MR. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clinical Epidemiology and Global Health. 2022;15:1–5. http://doi:10.101 /j.cegh.2022.101004.
13.
da Silva Santos AM, Rossi FE, dos Santos Nunes de Moura HP, Marreiro de Sousa Junior AV, dos Santos Nunes de Mora HP, Marreiro de Sousa Junior AV, Machado DCD, Neves LM, Brito AS, Moura P, Monteiro PA, Freitas Junior IF, Pereira dos Santos MA, Ribeiro SLG. COVID-19 pandemic impacts physical activity levels and sedentary time but not sleep quality in young badminton 2021;12:969–977. http://doi:10.1007/s11332-021-....
14.
Marelli S, Castelnuovo A, Somma A, Castronovo V, Mombelli S, Bottoni D, Leitner C, Fossati A, Ferini-Strambi L, Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology. 2021;268:8–15. http://doi:0.1007/s00415-020-1....
15.
Werneck AO, Silva DR, Malta DC, Lima MG, Souza-Júnior PRB, Azevedo LO, Barros MBA, Szwarcwald CL, The mediation role of sleep quality in the association between the incidence of unhealthy movement behaviors during the COVID-19 quarantine and mental health. Sleep Medicine. 2020;76:10–15. http://doi:10.1016/j.sleep.202....
16.
López-Bueno R, Calatayud J, Casaña J, Casajús JA, Smith L, Tully MA, Andersen LL, López-Sánchez GF. COVID-19 Confinement and.
17.
Health Risk Behaviours in Spain. Front Psychol. 2020;11:1–10. http:// doi:10.3389/fpsyg.2020.01426.
18.
Luo L, Song N, Yang H, Huang J, Zhou L, Zhang L, Intervention effect of Long-Term Aerobic`Training on Anxiety, Depression, and Sleep. Fronfiers in Psychiatry. 2021;12:1–8. http://doi:10.3389/ fpsyt.2021.720833.
19.
Aguilar-Farias N, Toledo-Vargas M, Miranda-Marquez S, Cortinez- O’Ryan A, Cristi-Montero C, Rodriguez-Rodriguez F, Martino- Fuentealba P, Okely AD, del Pozo Cruz B. Sociodemographic Predictors of Changes in Physical Activity, Screen Time, and Sleep among Toddlers and Preschoolers in Chile during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021;18:2–13. http://doi:10.3390/ijerph18010....
20.
Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attina A, Cinelli G, Leggeri C, Caparello G, Barrea L, Scerbo F, Esposito E, De Lorenzo A.Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. Journal of Translation Medicine. 2020;18:1–15. http:// doi:10.1186/s12967-020-02399-5.
21.
Pinto J, van Zeller M, Amorim P, Pimentel A, Dantas P, Eusébio E, Neves A, Pipa J, Santa Clara E, Santiago T, Viana P, Drummond M. Sleep quality in times of Covid-19 pandemic. Sleep Medicine. 2020;74:81–85. 21. Huang Y, Zhao N, Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional. Psychiatry Research. 2020;288:1–6. http://doi:10.1016/j. psychres.2020.112954.
22.
Segon T, Kerebih H, Gashawu F, Gashawa B, Tesfaye B, Nakie G, Anbesaqw T. Sleep quality and associated factors among nurses working at comprehensive specialized hospitals in Northwest, Ethiopia. Frontiers in Psychiatry. Insights in Sleep Disorders. Peer J. 2022;1–10. http:// doi:10.3389/fpsyt.2022.931588.
23.
Zhou Y, Bo S, Ruan S, Dai Q, Tian Y, Shi X, Deteriorated sleep quality and influencing factors among undergraduates in northern 2022;1–15. http://doi:10.7717/peerj.13833.
24.
Abdolalizadeh A, Nabavi S, Visual Attention and Poor Sleep Quality. Frontiers in Neuroscience 2022;1–12. http://doi:doi.org/10.3389/ fnins.2022.850372.
25.
Campos-Romero S, Barros Araya SC, Masalan-Apip MP, Tobar VG, Arias-Ortiz NE, Bobadilla-Beiza L. Sleep quality in people with type 2 diabetes controlled at the primary level and its association with sociodemographic and clinical characteristics. Enfermería Clínica. 2022;32,1:45–53. http://doi:10.1016/j.enfcle.20....
Udostępnij
ARTYKUŁ POWIĄZANY