REVIEW PAPER
Essential public health functions renewed by WHO should be a roadmap for building public health capacity and a resilient health system in Poland
1
Szkoła Zdrowia Publicznego, Centrum medyczne Kształcenia Podyplomowego, Warszawa, Polska
Corresponding author
Dorota Cianciara
Szkoła Zdrowia Publicznego Centrum medyczne Kształcenia Podyplomowego, ul. Kleczewska 61/63, 01-826 Warszawa, Polska
Szkoła Zdrowia Publicznego Centrum medyczne Kształcenia Podyplomowego, ul. Kleczewska 61/63, 01-826 Warszawa, Polska
Med Og Nauk Zdr. 2023;29(2):63-72
KEYWORDS
public healthessential public health operationsessential public health functionsemergency preparednesshealth systems strengthening
TOPICS
ABSTRACT
Introduction and objective:
The COVID-19 pandemic is a public health failure at multiple levels worldwide and in Poland. The aim of the article is to discuss pre-pandemic and current ventures aimed at public health capacity building in Poland, in focus on emergency preparedness and response, and the list of essential public health functions (EPHFs) renewed by WHO.
Review methods:
The assessment was based on legal regulations and publications on the implementation of public health functions published on the websites of the Statistics Poland, ISAP, Polish Academy of Sciences, Ministry of Health, National Institute of Public Health-National Institute of Hygiene, Supreme Audit Office, Council of Ministers, Government Legislation Centre, Sejm of the Republic of Poland and the OECD, PAHO, WHO.
Brief description of the state of knowledge:
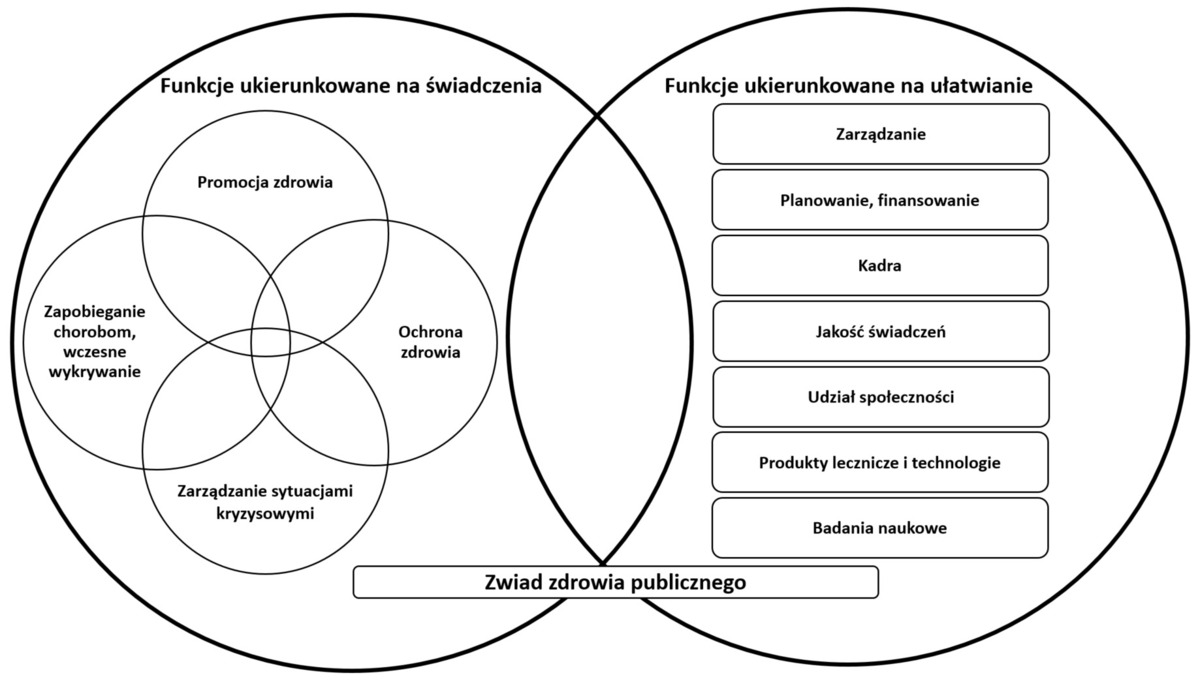
Diagnosis of the public health functioning in Poland based on the concept of essential public health operations (EPHOs) according to the WHO Regional Office for Europe showed shortcomings. The EPHOs functions were not mapped in the Public Health Act. Neither the Act nor the National Health Programmes covered the issues of preparedness and response. Current documents and publications on public health activities do not raise antiepidemic measures. WHO’s renewed essential public health functions (EPHFs) include managing public health emergency and functions new to EPHOs.
Summary:
It is necessary to consider the functions, structure and organization of public health in Poland. It should involve many stakeholders. Renewed EPHFs should be considered in public health capacity building.
The COVID-19 pandemic is a public health failure at multiple levels worldwide and in Poland. The aim of the article is to discuss pre-pandemic and current ventures aimed at public health capacity building in Poland, in focus on emergency preparedness and response, and the list of essential public health functions (EPHFs) renewed by WHO.
Review methods:
The assessment was based on legal regulations and publications on the implementation of public health functions published on the websites of the Statistics Poland, ISAP, Polish Academy of Sciences, Ministry of Health, National Institute of Public Health-National Institute of Hygiene, Supreme Audit Office, Council of Ministers, Government Legislation Centre, Sejm of the Republic of Poland and the OECD, PAHO, WHO.
Brief description of the state of knowledge:
Diagnosis of the public health functioning in Poland based on the concept of essential public health operations (EPHOs) according to the WHO Regional Office for Europe showed shortcomings. The EPHOs functions were not mapped in the Public Health Act. Neither the Act nor the National Health Programmes covered the issues of preparedness and response. Current documents and publications on public health activities do not raise antiepidemic measures. WHO’s renewed essential public health functions (EPHFs) include managing public health emergency and functions new to EPHOs.
Summary:
It is necessary to consider the functions, structure and organization of public health in Poland. It should involve many stakeholders. Renewed EPHFs should be considered in public health capacity building.
REFERENCES (63)
1.
Sachs JD, Karim SSA, Aknin L, et al. TheLancet Commission on lessons for the future from the COVID-19 pandemic. The Lancet 2022; 400(10359):1224–1280. https://doi.org/10.1016/S0140-....
2.
Banco E, Furlong A, Pfahler L. How Bill Gates and partners used their clout to control the global Covid response – with little oversight. Politico 09.14.2022. https://www.politico.com/news/... (access: 2023.05.03).
3.
Jędrzejczyk T, Balwicki Ł. Poland country snapshot: public health agencies and services in the response to COVID-19. European Observatory on Health Systems and Policies. March 2022. https://eurohealthob- servatory.who.int/news-room/articles/item/poland-country-snapshot-public-health-agencies-and-services-in-the-response-to-covid-19 (access:2023.05.03).
4.
Fiałek B. On the verge of Poland’s fifth wave of covid-19, healthcare staff are overworked and disenchanted. BMJ. 2022;376:o234. http://dx.doi.org/10.1136/bmj.....
5.
Mularczyk-Tomczewska P, Zarnowski A, Gujski M, et al. Barriers to accessing health services during the COVID-19 pandemic in Poland: A nationwide cross-sectional survey among 109,928 adults inPoland. Frontiers in Public Health 2022;10. https://doi.org/10.3389/ fpubh.2022.986996.
6.
Marcinkiewicz A. The impact of the COVID-19 pandemic on the resources and activities of basic occupational health services in Poland. Med Pr. 2022;73(1):19–24. https://doi.org/10.13075/mp.58....
7.
Główny Urząd Statystyczny. Trwanie życia w 2021 r. Warszawa 29.07.2022. https://stat.gov.pl/obszary-te... (access: 2023.05.03).
8.
Chrobak K, Burek W. Ustawodawstwo covidowe w świetle hierarchii źródeł prawa w Polsce – wybrane aspekty. Rocznik Administracji Publicznej. 2022(8):25–39. https://doi.org/10.4467/244978....
9.
Piotrowski R. Demokracja w czasie pandemii. Uwagi o doświadczeniach polskich. In: Prawo w czasie pandemii COVID-19. Warszawa: Wydawnictwo naukowe Scholar; 2021. p. 11–27. https://www.google.pl/books/ edition/Prawo_w_czasie_pandemii_COVID_19/bVukEAAAQBAJ?hl=pl&gbpv=1&printsec=frontcover (access: 2023.05.03).
10.
Owsiak K. Władze samorządowe wobec presji na wydatki związane z kryzysem pandemicznym. In: Zioło M, editor. Finanse publiczne, Warszawa: Polska Akademia Nauk; 2021. p. 63–81. https://publikacje.pan. pl/chapter/121863/rozdzial-4-wladze-samorzadowe-wobec-presji-na-wydatki-zwiazane-z-kryzysem-pandemicznym-br (access:2023.05.03).
11.
Martin-Moreno JM, Lobo-Valbuena B, Martin-Gorgojo A. Integra- ting Essential Public Health Functions in Health Systems Ensuring Health Security. [w:] Siddiqi S, Mataria A, Rouleau KD, Iqbal M. Ma- king Health Systems Work in Low and Middle Income Countries. Cambridge: Cambridge University Press; 2023. p. 496–510. https://doi. org/10.1017/9781009211086.
12.
Włodarczyk WC, Juszczyk G. Zdrowie publiczne 3.0. Wnioski po pan- demii COVID-19, perspektywa globalna. Policy paper. Warszawa: Narodowy Instytut Zdrowia Publicznego-Państwowy Zakład Higieny; 2022.
13.
Cianciara D, Szmigiel A, Pruszyński J. Recovery from COVID-19 crisis in public health perspective. Journal of Education, Health and Sport 2022;12(7):933–949. https://doi.org/10.12775/JEHS.....
14.
Brownson RC, Burke TA, Colditz GA, Samet JM. Reimagining Public Health in the Aftermath of a Pandemic. Am J Public Health. 2020;110(11):1605–1610. https://doi.org/10.2105/AJPH.2....
15.
S.674 – Public Health Infrastructure Saves Lives Act. https://www.congress.gov/bill/... (access:2023.05.03).
16.
House of Commons. Health and Social Care and Science and Tech- nology Committees. Coronavirus: lessons learned to date. 12 October 2021:32. https://committees.parliament....- ments/78687/default/ (access:2023.05.03).
17.
World Health Organization. Zero draft of the WHO CA+ for the con- sideration of the Intergovernmental Negotiating Body at its fourth meeting. WHO convention, agreement or other international instrument on pandemic prevention, preparedness and response (“WHO CA+”). February 2023. https://apps.who.int/gb/inb/pd... (access:2023.05.03).
18.
World Health Organization. 21st century health challenges. Can the essential public health functions make a difference? Discussion Paper. WHO, Geneva; 2021. https://www.who.int/publicatio... item/9789240038929 (access:2023.05.03).
19.
WHO Regional Office for Europe. Regional Committee for Eu- rope. Resolution European Action Plan for Strengthening Public Health Capacities and Services. Sixty-second session Malta, 10–13 September 2012. EUR/RC62/R5. https://apps.who.int/iris/bit- stream/handle/10665/336533/62rs05e-EAPPublicHealth-122086. pdf?sequence=1&isAllowed=y (access:2023.05.03).
20.
WHO Regional Office for Europe. Regional Committee for Europe. European Action Plan for Strengthening Public Health Capacities and Services.Sixty-second session Malta, 10–13 September 2012. https://apps.who.int/iris/bits... (ac- cess:2023.05.03).
21.
Martin-Moreno JM. Self-assessment tool for the evaluation of es- sential public health operations in the WHO European Region, WHO Regional Office for Europe, Copenhagen; 2015. https://apps. who.int/iris/bitstream/handle/10665/344398/9789289050999-eng. pdf?sequence=1&isAllowed=y (access:2023.05.03).
22.
Harris M, Ruseva M, Mircheva D, et al. Self-assessments of the essential public health operations in the WHO European Region 2007–2015 Experiences and lessons from seven Member States. WHO Regional Office for Europe, Copenhagen; 2017. https://apps.who.int/iris/bits... am/handle/10665/351404/WHO-EURO-2017-4786-44549-63086-eng. pdf?sequence=1&isAllowed=y (access:2023.05.03).
23.
Najwyższa Izba Kontroli. Ochrona ludności w ramach zarządzania kryzysowego i obrony cywilnej. Informacja o wynikach kontroli. KPB.430.009.2017 Nr ewid. 147/2018/P/17/039/KPB. War- szawa, 12.09.2018. https://www.nik.gov.pl/plik/id... (access:2023.05.03).
24.
WHO Regional Office for Europe. Midterm progress report on im- plementation of the European Action Plan for Strengthening Public Health Capacities and Services. Regional Committee for Euro- pe EUR/RC66/19 66th session Copenhagen, 12–15 September 2016. https://apps.who.int/iris/bits... 160568.pdf?sequence=1&isAllowed=y (access:2023.05.03).
25.
Mok EA, Gostin LO, Gupta MD, et al. Implementing Public Health Re- gulations in Developing Countries: Lessons from the OECD Countries. J. Law, Med. & Ethics 2010; 38(3):508–519. https://doi.org/10.1111/j.1748- 720X.2010.00509.x.
26.
Lee Y, Kim SY. Public health law coverage in support of the health- -related sustainable development goals (SDGs) among 33 Western Pacific countries. Global Health. 2019;15:29. https://doi.org/10.1186/ s12992-019-0472-z.
27.
Rządowe Centrum Legislacji. Projekt ustawy o zdrowiu publicznym. 28.03.2015. https://legislacja.rcl.gov.pl/... (access:2023.05.03).
28.
Rządowe Centrum Legislacji. Projekt ustawy o zdrowiu publicznym. Raport z konsultacji publicznych i opiniowania dot. projektu ustawy o zdrowiu publicznym (Pt II). https://legislacja.rcl.gov.pl/... (access:2023.05.03).
29.
SEJM RP. Rządowy projekt ustawy o zdrowiu publicznym. https://www. sejm.gov.pl/sejm7.nsf/PrzebiegProc.xsp?nr=3675 (access:2023.05.03).
30.
Ustawa z dnia 11 września 2015 r. o zdrowiu publicznym. DzU 2015 poz.1916 z późń.zm.
31.
Rozporządzenie Ministra Zdrowia z dnia 21 grudnia 2016 r. w sprawie rocznej informacji o zrealizowanych lub podjętych zadaniach z zakresu zdrowia publicznego. DzU 2016, poz. 2216.
32.
Główny Urząd Statystyczny. Wydatki na ochronę zdrowia w latach 2019–2021. Warszawa: GUS; 29.07.2022. https://stat.gov.pl/obszary-te...- tach-2019–2021,27,2.html (access:2023.05.03).
33.
OECD. Health expenditure and financing. https://stats.oecd.org/ viewhtml.aspx?datasetcode=SHA&lang=en (access:2023.05.03).
34.
Izdebski H. Zakres przedmiotowy ustawy o zdrowiu publicznym – propozycje zmian. PL13 – Predefined Project: „Reducing social inequalities in health” co-financed by the Norwegian Financial Mechanism Final conference 6–7 April 2017. http://bazawiedzy.pzh.gov.pl/n... w zdrowiu (access:2023.05.03).
35.
Dercz M. Ogólne podstawy prawne zdrowia publicznego w Polsce – stan obecny i postulowany. PL13 – Predefined Project: „Reducing social inequalities in health” co-financed by the Norwegian Financial Mechanism Final conference 6–7 April 2017. http://bazawiedzy.pzh. gov.pl/nierownosci-w-zdrowiu (access:2023.05.03).
36.
Rozporządzenie Rady Ministrów z dnia 4 sierpnia 2016 r. w sprawie Narodowego Programu Zdrowia na lata 2016–2020. DzU 2016 poz. 1492.
37.
Rozporządzenie Rady Ministrów z dnia 30 marca 2021 r. w sprawie Narodowego Programu Zdrowia na lata 2021–2025. DzU 2021 poz. 642.
38.
Najwyższa Izba Kontroli. Realizacja zadań Narodowego Progra- mu Zdrowia na lata 2016–2020. Informacja o wynikach kontroli. KZD.430.001.2020 Nr ewid. 2/2020/P/19/060/KZD. https://www.nik. gov.pl/kontrole/P/19/060/LLO/ (access:2023.05.03).
39.
Cianciara D, Sugay L, Urban E, et al, editors. Sektorowa Rama Kwalifikacji dla Zdrowia Publicznego (SRK ZP). Instytut Badań Edukacyjnych, Warszawa; 2020. https://kwalifikacje.edu.pl/wp... (access:2023.05.03).
40.
WHO Regional Office for Europe, ASPHER. Roadmap to professio nalizing the public health workforce in the European Region. WHO, Copenhagen; 2022: 73–74. https://www.aspher.org/downloa... who-euro-2022-4808-44517-63144-eng.pdf (access:2023.05.03).
41.
Ministerstwo Zdrowia. Zdrowa Przyszłość. Ramy strategiczne roz- woju systemu ochrony zdrowia na lata 2021–2027, z perspektywą do 2030. Załącznik do uchwały nr 196/2021 Rady Ministrów z dnia 27 grudnia 2021 r. https://www.gov.pl/web/zdrowie... do-2030 (access:2023.05.03).
42.
Rządowe Centrum Legislacji. Projekt ustawy o niektórych zawodach medycznych. 21.01.2022. https://legislacja.rcl.gov.pl/... katalog/12849352#12849352 (access:2023.05.03).
43.
Sejm RP. Rządowy projekt ustawy o niektórych zawo- dach medycznych https://www.sejm.gov.pl/sejm9..... xsp?symbol=RPL&Id=RM-0610-33-23 (access:2023.05.03).
44.
Rozporządzenie Ministra Nauki i Szkolnictwa Wyższego z dnia 12 lipca 2007 r. w sprawie standardów kształcenia dla poszczególnych kierunków oraz poziomów kształcenia, a także trybu tworzenia i warunków, jakie musi spełniać uczelnia, by prowadzić studia międzykierunkowe oraz makrokierunki. Standardy kształcenia dla kierunku studiów: Zdrowie publiczne. Załącznik nr 117. DzU 2007 nr 164 poz. 1166.
45.
Rozporządzenie Ministra Nauki i Szkolnictwa Wyższego z dnia 2 li- stopada 2011 r. w sprawie Krajowych Ram Kwalifikacji dla Szkolnictwa Wyższego. DzU 2011 nr 253 poz. 1520.
46.
Rozporządzenie Ministra Nauki i Szkolnictwa Wyższego z dnia 14 listopada 2018 r. w sprawie charakterystyk drugiego stopnia efektów uczenia się dla kwalifikacji na poziomach 6–8 Polskiej Ramy Kwalifikacji. DzU 2018 poz. 2218.
47.
Ministerstwo Zdrowia. Mapy potrzeb zdrowotnych. Studenci i absolwenci kierunków medycznych. https://basiw.mz.gov.pl/mapy-i... (access:2023.05.03).
48.
Domagała A. Forum absolwentów i pracodawców – zdrowie publiczne z perspektywy ukończonych studiów wyższych i rynku pracy. Relacja z dyskusji panelowej w trakcie konferencji z okazji 30-lecia IZP UJCM. Zdrowie Publiczne i Zarządzanie 2021;19(3–4):173–179. https://doi.org/10.4467/208426....
49.
Hanke W, Heitzman J, Juszczyk G, Samoliński B, et al, editors. Polskie Zdrowie 2.0. Rekomendacje strategiczne na lata 2023–2027. Zasadnicze wzmocnienie zdrowia publicznego. Policy brief II.1. Komitet Zdrowia Publicznego, Polska Akademia Nauk, Warszawa: 2023. https://pan.pl/ wp-content/uploads/2023/03/Polskie-Zdrowie-2.0_Brief-nr-II.1_Za- sadnicze-wzmocnienie-zdrowia-publicznego-1.pdf (access:2023.05.03).
50.
Rao R, Hawkins M, Ulrich T, et al. The Evolving Role of Public Health in Medical Education. Front Public Health. 2020 Jun 26;8:251. https:// doi.org/10.3389/fpubh.2020.00251.
51.
Vargas C, Whelan J, Brimblecombe J, et al. Co-creation, co-design and co-production for public health: a perspective on definitions and distinctions. Public Health Res Pract. 2022 Jun 15;32(2):3222211. https:// doi.org/10.17061/phrp3222211.
52.
World Health Organization. Resolution WHA69.1. Strengthening essen- tial public health functions in support of the achievement of universal health coverage. Sixty-ninth World Health Assembly. Resolutions and decisions, annexes. Geneva 23–28 May 2016: 3–6. https://apps.who.int/ gb/ebwha/pdf_files/WHA69-REC1/A69_2016_REC1-en.pdf#page=1 (access:2023.05.03).
53.
Martin-Moreno JM, Harris M, Jakubowski E, et al. Defining and Asses- sing Public Health Functions: A Global Analysis. Annu Rev Public Health. 2016. 37:12.1–12.21. https://doi.org/ annurev-publhealth-032315-021429.
54.
World Health Organization. Essential public health functions, health systems and health security: developing conceptual clarity and a WHO roadmap for action. WHO, Geneva 2018. https://apps. who.int/iris/bitstream/handle/10665/272597/9789241514088-eng. pdf?sequence=1&isAllowed=y (access:2023.05.03).
55.
Pan American Health Organization. The Essential Public Health Fun- ctions in the Americas: A Renewal for the 21st Century. Conceptual Framework and Description. Washington D.C.; 2020. https://iris.paho. org/handle/10665.2/53124 (access:2023.05.03).
56.
Báscolo E, Houghton N, Del Riego A, et al. Contributions of the New Framework for Essential Public Health Functions to Addressing the COVID-19 Pandemic Am J Public Health 2022;112(S6):615-S620. https://doi.org/10.2105/AJPH.2....
57.
Zhang Y, McDarby G, Seifeldin R, et al. Towards applying the essential public health functions for building health systems resilience: A renewed list and key enablers for operationalization. Front Public Health. 2023;10:1107192. https://doi.org/10.3389/fpubh.....
58.
World Health Organization. National workforce capacity to implement the essential public health functions including a focus on emergency preparedness and response Action plan (2022–2024) for aligning WHO and partner contributions. WHO, Geneva 2022. https://www.who.int/publicatio... (access:2023.05.03).
59.
Hunter MB, Ogunlayi F, MiddletonJ, et al. Strengthening capacity through competency-based education and training to deliver the essential public health functions: reflection on roadmap to build public health workforce. BMJ Global Health 2023;8:e011310. http://dx.doi. org/10.1136/bmjgh-2022-011310.
60.
World Health Organization. Technical brief. Essential public health fun- ctions A sustainable approach to ensure multi-sectoral actions for population health. October 2022. https://cdn.who.int/media/docs... (access:2023.05.03).
61.
McDarby G, Mustafa S, Y Zhang Y, et al. Essential Public Health Functions in Ireland: Perspectives to strengthen capacities and stewardship, Eur J Public Health 2022; 32(Suppl 3); ckac129.207. https:// doi.org/10.1093/eurpub/ckac129.207.
62.
McNicholas T, Hendrick L, McDarby G, et al. A novel approach to utilizing the essential public health functions in Ireland's health system recovery and reform. Front Public Health. 2023;11:1074356. https://doi. org/10.3389/fpubh.2023.1074356.
63.
Espinosa MF, Andriukaitis VP, Kickbusch I, et al. Realising the right to health for all people – UHC is the umbrella to deliver health for all. Lancet Glob Health 2023: S2214-09X(23)00202–4. https://doi.org/10.1016/ S2214-109X(23)00202-4.
Share
RELATED ARTICLE