Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Ocena wpływu pandemii COVID-19 na poziom realizacji świadczeń zdrowotnych w Polsce – przegląd doniesień naukowych
1
Instytut Zdrowia Publicznego, Wydział Nauk o Zdrowiu, Uniwersytet Jagielloński Collegium Medicum, Polska
Autor do korespondencji
Magdalena Agata Mrożek-Gąsiorowska
Instytut Zdrowia Publicznego, Wydział Nauk o Zdrowiu, Uniwersytet Jagielloński Collegium Medicum, ul. Skawińska 8, 31-066 Kraków, Polska
Instytut Zdrowia Publicznego, Wydział Nauk o Zdrowiu, Uniwersytet Jagielloński Collegium Medicum, ul. Skawińska 8, 31-066 Kraków, Polska
Med Og Nauk Zdr. 2023;29(4):251-261
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Pandemia COVID-19 miała ogromny wpływ na system ochrony zdrowia. Celem pracy jest ocena wpływu pandemii na stopień realizacji różnego rodzaju świadczeń zdrowotnych w Polsce, przeprowadzona na podstawie analizy dostępnych doniesień naukowych.
Metody przeglądu:
Przeszukanie bazy Medline przeprowadzono 1 sierpnia 2023 roku. Do przeglądu włączono wszystkie odnalezione badania – niezależnie od ich rodzaju, okresu obserwacji, ocenianej interwencji/świadczenia zdrowotnego oraz populacji/grupy pacjentów, do której kierowane były dane świadczenia zdrowotne.
Opis stanu wiedzy:
Odnaleziono 46 badań. Badania te opierają się albo na danych ogólnopolskich, przede wszystkim pochodzących z bazy Narodowego Funduszu Zdrowia, albo na danych z dokumentacji medycznej placówek. Większość prac dotyczy pierwszych okresów pandemii w Polsce, tj. 2020 roku lub wybranych miesięcy 2020 roku (32 prace). Badania dotyczą głównie leczenia szpitalnego wybranych chorób, a także podstawowej opieki zdrowotnej, stomatologii, programów profilaktycznych, ratownictwa medycznego i poszczególnych świadczeń, takich jak operacje zaćmy, endoprotezoplastyka oraz przeszczepy. Brak badań dla niektórych świadczeń, m.in. rehabilitacji, opieki długoterminowej, opieki psychiatrycznej i wielu poszczę
Podsumowanie:
Pandemia COVID-19 znacznie ograniczyła stopień realizacji większości świadczeń zdrowotnych (74% badań). Spadek liczby udzielanych świadczeń często wynosił kilkadziesiąt procent (a w niektórych przypadkach nawet 100%), szczególnie gdy analizowany był krótki okres, np. obejmujący wybraną falę pandemii, gdy działalność wielu placówek była niemal całkowicie zawieszona. Konieczna jest analiza długoterminowa, uwzględniająca wszystkie zakresy świadczeń, która pozwoli wskazać obszary wymagające najpilniejszej interwencji.
Pandemia COVID-19 miała ogromny wpływ na system ochrony zdrowia. Celem pracy jest ocena wpływu pandemii na stopień realizacji różnego rodzaju świadczeń zdrowotnych w Polsce, przeprowadzona na podstawie analizy dostępnych doniesień naukowych.
Metody przeglądu:
Przeszukanie bazy Medline przeprowadzono 1 sierpnia 2023 roku. Do przeglądu włączono wszystkie odnalezione badania – niezależnie od ich rodzaju, okresu obserwacji, ocenianej interwencji/świadczenia zdrowotnego oraz populacji/grupy pacjentów, do której kierowane były dane świadczenia zdrowotne.
Opis stanu wiedzy:
Odnaleziono 46 badań. Badania te opierają się albo na danych ogólnopolskich, przede wszystkim pochodzących z bazy Narodowego Funduszu Zdrowia, albo na danych z dokumentacji medycznej placówek. Większość prac dotyczy pierwszych okresów pandemii w Polsce, tj. 2020 roku lub wybranych miesięcy 2020 roku (32 prace). Badania dotyczą głównie leczenia szpitalnego wybranych chorób, a także podstawowej opieki zdrowotnej, stomatologii, programów profilaktycznych, ratownictwa medycznego i poszczególnych świadczeń, takich jak operacje zaćmy, endoprotezoplastyka oraz przeszczepy. Brak badań dla niektórych świadczeń, m.in. rehabilitacji, opieki długoterminowej, opieki psychiatrycznej i wielu poszczę
Podsumowanie:
Pandemia COVID-19 znacznie ograniczyła stopień realizacji większości świadczeń zdrowotnych (74% badań). Spadek liczby udzielanych świadczeń często wynosił kilkadziesiąt procent (a w niektórych przypadkach nawet 100%), szczególnie gdy analizowany był krótki okres, np. obejmujący wybraną falę pandemii, gdy działalność wielu placówek była niemal całkowicie zawieszona. Konieczna jest analiza długoterminowa, uwzględniająca wszystkie zakresy świadczeń, która pozwoli wskazać obszary wymagające najpilniejszej interwencji.
Introduction and objective:
The COVID-19 pandemic has had a huge impact on the health care system. The aim of the study is to assess the impact of the pandemic on the level of provision of various types of health services in Poland, based on the analysis of available scientific evidence.
Review methods:
A Medline database search was conducted on 1 August, 2023. All studies were included, regardless of the type, observation period, assessed intervention/health service and the population/group of patients to which the health services was addressed.
Brief description of the state of knowledge:
46 studies were found. These studies are based either on nationwide data, mainly from the National Health Fund database, or on data from medical records collected by the healthcare providers. Most of the studies concern the first periods of the COVID-19 pandemic in Poland, i.e. 2020 or selected months of 2020 (32 studies). Research mainly concerns hospital treatment of selected diseases, as well as primary health care, dentistry, preventive programmes, emergency medical services and individual services, such as cataract surgery, arthroplasty and transplants. There are no studies concerning services in the field of, among others: rehabilitation, long-term care, mental health care and many individual types of health services provided within a given scope.
Summary:
The COVID-19 pandemic has significantly limited the degree of provision of most health services (74% studies). The decrease in the number of services provided was often several dozen percent (and in some cases even 100%), especially when a short period was analyzed, e.g. a selected wave of the pandemic, during which the activity of many facilities was almost completely suspended. A long-term analysis is necessary, taking into account all scopes of services, which will allow to identify areas requiring the most urgent intervention.
The COVID-19 pandemic has had a huge impact on the health care system. The aim of the study is to assess the impact of the pandemic on the level of provision of various types of health services in Poland, based on the analysis of available scientific evidence.
Review methods:
A Medline database search was conducted on 1 August, 2023. All studies were included, regardless of the type, observation period, assessed intervention/health service and the population/group of patients to which the health services was addressed.
Brief description of the state of knowledge:
46 studies were found. These studies are based either on nationwide data, mainly from the National Health Fund database, or on data from medical records collected by the healthcare providers. Most of the studies concern the first periods of the COVID-19 pandemic in Poland, i.e. 2020 or selected months of 2020 (32 studies). Research mainly concerns hospital treatment of selected diseases, as well as primary health care, dentistry, preventive programmes, emergency medical services and individual services, such as cataract surgery, arthroplasty and transplants. There are no studies concerning services in the field of, among others: rehabilitation, long-term care, mental health care and many individual types of health services provided within a given scope.
Summary:
The COVID-19 pandemic has significantly limited the degree of provision of most health services (74% studies). The decrease in the number of services provided was often several dozen percent (and in some cases even 100%), especially when a short period was analyzed, e.g. a selected wave of the pandemic, during which the activity of many facilities was almost completely suspended. A long-term analysis is necessary, taking into account all scopes of services, which will allow to identify areas requiring the most urgent intervention.
Mrożek-Gąsiorowska MA. Ocena wpływu pandemii COVID-19 na poziom realizacji świadczeń zdrowotnych w Polsce – przegląd doniesień naukowych. Med Og Nauk Zdr. 2023; 29(4): 251–261. doi: 10.26444/monz/177033
REFERENCJE (78)
1.
Rozporządzenie Rady Ministrów z dnia 31 marca 2020 r. w sprawie ustanowienia określonych ograniczeń, nakazów i zakazów w związku z wystąpieniem stanu epidemii (DzU 2020 poz. 566 z późn. zm.).
2.
Rozporządzenie Rady Ministrów z dnia 13 maja 2022 r. zmieniające rozporządzenie w sprawie ustanowienia określonych ograniczeń, nakazów i zakazów w związku z wystąpieniem stanu epidemii (DzU 2022 poz. 1025 z późn. zm.).
3.
Moynihan R, Sanders S, Michaleff ZA, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021 Mar 16;11(3):e045343. doi:10.1136/bmjopen-2020-045343.
4.
Nimavat N, Hasan MM, Charmode S, et al. COVID-19 pandemic effects on the distribution of healthcare services in India: A systematic review. World J Virol. 2022 Jul 25;11(4):186–197. doi:10.5501/wjv.v11.i4.186.
5.
Gadsden T, Downey LE, Vilas VDR, et al. The impact of COVID-19 on essential health service provision for noncommunicable diseases in the South-East Asia region: A systematic review. Lancet Reg Health Southeast Asia. 2022 Jun;1:100010. doi:10.1016/j.lansea.2022.04.006.
6.
Wan Mohd Yunus WMA, Kauhanen L, Sourander A, et al. Registered psychiatric service use, self-harm and suicides of children and young people aged 0–24 before and during the COVID-19 pandemic: a systematic review. Child Adolesc Psychiatry Ment Health. 2022 Feb 25;16(1):15. doi:10.1186/s13034-022-00452-3.
7.
Zangani C, Ostinelli EG, Smith KA, et al. Impact of the COVID-19 Pandemic on the Global Delivery of Mental Health Services and Telemental Health: Systematic Review. JMIR Ment Health. 2022 Aug 22;9(8):e38600. doi:10.2196/38600.
8.
Duden GS, Gersdorf S, Stengler K. Global impact of the COVID-19 pandemic on mental health services: A systematic review. J Psychiatr Res. 2022 Oct;154:354–377. doi:10.1016/j.jpsychires.2022.08.013.
9.
VanBenschoten H, Kuganantham H, Larsson EC, et al. Impact of the COVID-19 pandemic on access to and utilisation of services for sexual and reproductive health: a scoping review. BMJ Glob Health. 2022 Oct;7(10):e009594. doi:10.1136/bmjgh-2022-009594.
10.
Xu Y, Mandal I, Lam S, et al. Impact of the COVID-19 pandemic on interventional radiology services across the world. Clin Radiol. 2021 Aug;76(8):621–625. doi:10.1016/j.crad.2021.05.001.
11.
Majeed A, Wright T, Guo B, et al. The Global Impact of COVID-19 on Childhood Cancer Outcomes and Care Delivery – A Systematic Review. Front Oncol. 2022 Apr 7;12:869752. doi:10.3389/fonc.2022.869752.
12.
Ferrara P, Dallagiacoma G, Alberti F, et al. Prevention, diagnosis and treatment of cervical cancer: A systematic review of the impact of COVID-19 on patient care. Prev Med. 2022 Nov;164:107264. doi:10.1016/j.ypmed.2022.107264.
13.
Di Cosimo S, Susca N, Apolone G, et al. The worldwide impact of COVID-19 on cancer care: A meta-analysis of surveys published after the first wave of the pandemic. Front Oncol. 2022 Sep 29;12:961380. doi:10.3389/fonc.2022.961380.
14.
Dhada S, Stewart D, Cheema E, et al. Cancer Services During the COVID-19 Pandemic: Systematic Review of Patient's and Caregiver's Experiences. Cancer Manag Res. 2021 Jul 29;13:5875–5887. doi:10.2147/CMAR.S318115.
15.
Nadarajah R, Wu J, Hurdus B, et al. The collateral damage of COVID-19 to cardiovascular services: a meta-analysis. Eur Heart J. 2022 Sep 1;43(33):3164–3178. doi:10.1093/eurheartj/ehac227.
16.
Seidu S, Kunutsor SK, Cos X, et al. Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: A systematic review. Prim Care Diabetes. 2021 Aug;15(4):653–681. doi:10.1016/j.pcd.2021.05.011.
17.
Kiss P, Carcel C, Hockham C, et al. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021 Jan 25;7(1):18–27. doi:10.1093/ehjqcco/qcaa084.
18.
Deng D, Liang A, Chui JN, et al. The COVID-19 pandemic and access to health care in people with chronic kidney disease: A systematic review and meta-analysis. Nephrology (Carlton). 2022 May;27(5):410–420. doi:10.1111/nep.14016.
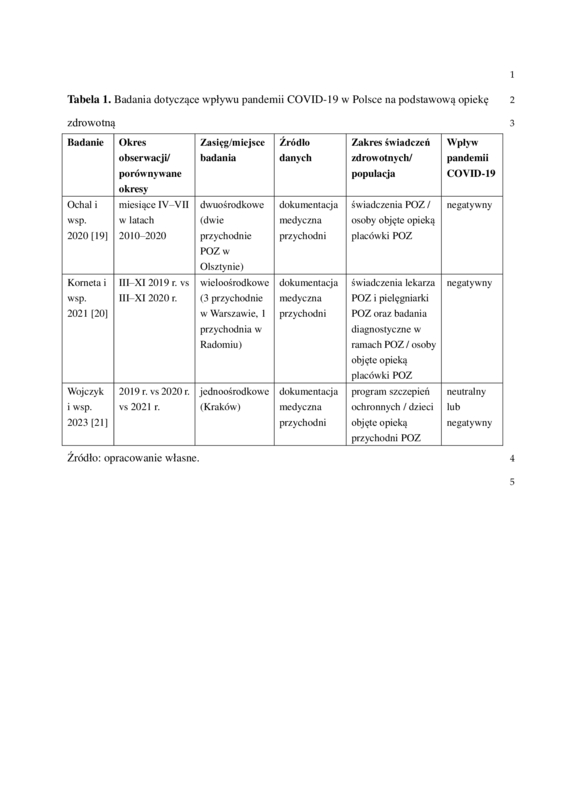
19.
Ochal M, Romaszko M, Glińska-Lewczuk K, et al. Assessment of the Consultation Rate with General Practitioners in the Initial Phase of the COVID-19 Pandemic. Int J Environ Res Public Health. 2020;17(21):7710. doi:10.3390/ijerph17217710.
20.
Korneta P, Kludacz-Alessandri M, Walczak R. The Impact of COVID-19 on the Performance of Primary Health Care Service Providers in a Capitation Payment System: A Case Study from Poland. Int J Environ Res Public Health. 2021;18(4):1407. doi:10.3390/ijerph18041407.
21.
Wojczyk M, Potocka M. Implementation of the preventive vaccination program in the time of the COVID-19 pandemic – single center study. Przegl Epidemiol. 2023;77(1):74–83. doi:10.32394/pe.77.08.
22.
Olszewska A, Paszynska E, Roszak M, et al. Management of the Oral Health of Children During the COVID-19 Pandemic in Poland. Front Public Health. 2021;9:635081. doi:10.3389/fpubh.2021.635081.
23.
Nijakowski K, Cieślik K, Łaganowski K, et al. The Impact of the COVID-19 Pandemic on the Spectrum of Performed Dental Procedures. Int J Environ Res Public Health. 2021;18(7):3421. doi:10.3390/ijerph18073421.
24.
Poniewierza P, Panek G. Cervical Cancer Prevention in the Era of the COVID-19 Pandemic. Medicina (Kaunas). 2022;58(6):732. doi:10.3390/medicina58060732.
25.
Greczka G, Dąbrowski P, Zych M, et al. The impact of the COVID 19 pandemic on the functioning of the Universal Newborn Hearing Screening Program in Poland. Otolaryngol Pol. 2022;76(4):1–5. doi:10.5604/01.3001.0015.9079.
26.
Czuba B, Mlodawski J, Kajdy A, et al. Implementation of the Publicly Funded Prenatal Screening Programme in Poland during the COVID-19 Pandemic: A Cross-Sectional Study. J Clin Med. 2022;11(5):1317. doi:10.3390/jcm11051317.
27.
Marcinkiewicz A. Wpływ pandemii Covid-19 na zasoby i działalność jednostek podstawowych służby medycyny pracy w Polsce. Med Pr. 2022;73(1):19–24. doi:10.13075/mp.5893.01217.
28.
Niedźwiedzka-Stadnik M, Nowakowska-Radziwonka E, Rosińska M, et al. Changes in HIV testing trends in Poland during COVID-19 pandemic. Przegl Epidemiol. 2022;76(2):255–266. doi:10.32394/pe.76.25.
29.
Serwin AB, Kaczyńska J, Flisiak I. The impact of the COVID-19 pandemic on sexually transmitted infections services – experience from Bialystok, Poland. Przegl Epidemiol. 2021;75(2):151–158. doi:10.32394/pe.75.14.
30.
Legutko J, Niewiara Ł, Bartuś S, et al. Decline in the number of coronary angiography and percutaneous coronary intervention procedures in patients with acute myocardial infarction in Poland during the coronavirus disease 2019 pandemic. Kardiol Pol. 2020;78(6):574–576. doi:10.33963/KP.15393.
31.
Budrejko S, Kempa M, Królak T, et al. Procedural volume of cardiac electrotherapy procedures does not have to be reduced during COVID-19 pandemic – one year analysis from a tertiary Polish center. Kardiol Pol. 2021;79(7–8):848–850. doi:10.33963/KP.a2021.0001.
32.
Wranicz JK, Drożdż J, Różycka-Kosmalska M, et al. Impact of the COVID-19 pandemic on the performance of selected cardiac electrotherapy and electrophysiology procedures. Kardiol Pol. 2021;79(4):452–454. doi:10.33963/KP.15884.
33.
Litwinowicz R, Filip G, Kapelak B, et al. Decrease of surgical heart disease treatment during the COVID-19 pandemic (Cardiac Surgery COVID-19 Study – CSC 19 Study). Kardiochir Torakochirurgia Pol. 2022;19(2):70–74. doi:10.5114/kitp.2022.117494.
34.
Gościniak P, Baumert B, Milczarek S, et al. The Impact of the COVID-19 Pandemic on the Organization of Cardio-Hematology Care-A Polish Single Center Experience. Medicina (Kaunas). 2022;58(3):337. doi:10.3390/medicina58030337.
35.
Miękisiak G, Pettersson SD, Szarek D, et al. Acute Stroke Care during COVID-19: National Data. Infect Dis Rep. 2022;14(2):198–204. doi:10.3390/idr14020024.
36.
Miękisiak G, Fercho J, Pettersson SD, et al. Impact of COVID-19 on incidence and treatment of intracranial aneurysms in Poland: a national study. Neurol Neurochir Pol. 2022;56(1):96–100. doi:10.5603/PJNNS.a2022.0006.
37.
Jonik S, Boszko M, Sztemberg E, et al. Heart team consultations for patients with severe coronary artery disease or valvular heart disease in the era of the COVID-19 pandemic: a single-center experience. Front Cardiovasc Med. 2023;10:1203535. doi:10.3389/fcvm.2023.1203535.
38.
Ostrowska M, Kasprzak M, Stolarek W, et al. Comparison of reorganized versus unaltered cardiology departments during the COVID-19 era: A subanalysis of the COV-HF-SIRIO 6 study. Cardiol J. 2023;30(3):344–352. doi:10.5603/CJ.a2023.0002.
39.
Jankowska-Sanetra J, Sanetra K, Konopko M, et al. The impact of first wave of the SARS-CoV-2 2019 pandemic in Poland on characteristics and outcomes of patients hospitalized due to stable coronary artery disease. Cardiol J. 2023;30(3):337–343. doi:10.5603/CJ.a2022.0094.
40.
Malicki J, Martenka P, Dyzmann-Sroka A, et al. Impact of COVID-19 on the performance of a radiation oncology department at a major comprehensive cancer centre in Poland during the first ten weeks of the epidemic. Rep Pract Oncol Radiother. 2020;25(5):820–827. doi:10.1016/j.rpor.2020.08.001.
41.
Szewczyk M, Pazdrowski J, Golusiński P, et al. The impact of the COVID-19 pandemic on the management of head and neck cancer patients at a tertiary care institution in Poland. Contemp Oncol (Pozn). 2021;25(4):264–269. doi:10.5114/wo.2021.111310.
42.
Maluchnik M, Podwójcic K, Więckowska B. Decreasing access to cancer diagnosis and treatment during the COVID-19 pandemic in Poland. Acta Oncol. 2021;60(1):28–31. doi:10.1080/0284186X.2020.1837392.
43.
Kędzierska-Kapuza K, Witkowski G, Baumgart-Gryn K, et al. Impact of COVID-19 on pancreatic cancer surgery: A high-volume Polish center experience. Adv Clin Exp Med. 2022;31(4):389–398. doi:10.17219/acem/144134.
44.
Zapała P, Ślusarczyk A, Rajwa P, et al. Not as black as it is painted? The impact of the first wave of COVID-19 pandemic on surgical treatment of urological cancer patients in Poland – a cross-country experience. Arch Med Sci. 2023;19(1):107–115. doi:10.5114/aoms/130927.
45.
Szarek D, Miękisiak G, Szmuda T, et al. The impact of the COVID-19 pandemic on the number of brain tumor surgeries in Poland: A national database study. Adv Clin Exp Med. 2023. doi:10.17219/acem/161726.
46.
Kurowicki M, Osowiecka K, Szostakiewicz B, et al. The Impact of the COVID-19 Pandemic on the Number of Cancer Patients and Radiotherapy Procedures in the Warmia and Masuria Voivodeship. Curr Oncol. 2023;30(1):1010–1019. doi:10.3390/curroncol30010077.
47.
Piątek S, Urbański F, Karczmarz S, et al. Assessment of Hospital Volume in the Surgical Management of Endometrial and Ovarian Cancer: A Polish Population-Based Study. Med Sci Monit. 2023;29:e938776. doi:10.12659/MSM.938776.
48.
Kaczmarek K, Kalembkiewicz J, Jankowska M, et al. Did the COVID-19 Pandemic Restrict Access to Emergency Urological Services: Assessment of Reorganisation Effectiveness for Hospital Treatment. Int J Environ Res Public Health. 2023;20(4):3735. doi:10.3390/ijerph20043735.
49.
Ratajczak JM, Gawrońska A, Fischer M, et al. Can We Identify Patients in Danger of Delayed Treatment? Management of COVID-19 Pandemic Backlog in Urology Care in Poland. Int J Environ Res Public Health. 2022;19(24):16547. doi:10.3390/ijerph192416547.
50.
Rajwa P, Przydacz M, Krajewski W, et al. Changing patterns of urologic emergency visits and admissions during the COVID-19 pandemic: a retrospective, multicenter, nationwide study. Arch Med Sci. 2020;17(5):1262–1276. doi:10.5114/aoms.2020.98364.
51.
Sękowski K, Grudziąż-Sękowska J, Goryński P, et al. Epidemiological Analysis of Diabetes-Related Hospitalization in Poland before and during the COVID-19 Pandemic, 2014–2020. Int J Environ Res Public Health. 2022;19(16):10030. doi:10.3390/ijerph191610030.
52.
Grudziąż-Sękowska J, Sękowski K, Kobuszewski B. Healthcare Utilization and Adherence to Treatment Recommendations among Children with Type 1 Diabetes in Poland during the COVID-19 Pandemic. Int J Environ Res Public Health. 2022;19(8):4798. doi:10.3390/ijerph19084798.
53.
Kleibert M, Mrozikiewicz-Rakowska B, Bąk PM, et al. Breakdown of Diabetic Foot Ulcer Care during the First Year of the Pandemic in Poland: A Retrospective National Cohort Study. Int J Environ Res Public Health. 2022;19(7):3827. doi:10.3390/ijerph19073827.
54.
Białynicki-Birula R, Siemasz I, Otlewska A, et al. Influence of COVID-19 pandemic on hospitalizations at the tertiary dermatology department in south-west Poland. Dermatol Ther. 2020;33(4):e13738. doi:10.1111/dth.13738.
55.
Czubak-Wrzosek M, Czubak J, Grzelecki D, et al. The Effect of the COVID-19 Pandemic on Total Hip and Knee Arthroplasty Surgical Volume in 2020 in Poland. Int J Environ Res Public Health. 2021;18(16):8830. doi:10.3390/ijerph18168830.
56.
Kazubski K, Tomczyk Ł, Kopczyński B, et al. The Epidemiology of Hip and Knee Primary and Revision Arthroplasties during the COVID-19 Pandemic. Healthcare (Basel). 2021;9(5):519. doi:10.3390/healthcare9050519.
57.
Kazubski K, Tomczyk Ł, Morasiewicz P. Effects of the COVID-19 Pandemic on the Epidemiology of Knee and Shoulder Arthroscopy. Inquiry. 2021;58:469580211056037. doi:10.1177/00469580211056037.
58.
Kuliński P, Tomczyk Ł, Morasiewicz P. Effect of the COVID-19 pandemic on foot surgeries. Adv Clin Exp Med. 2021;30(12):1249–1253. doi:10.17219/acem/140610.
59.
Dmuchowska DA, Pieklarz B, Konopinska J, et al. Impact of Three Waves of the COVID-19 Pandemic on the Rate of Elective Cataract Surgeries at a Tertiary Referral Center: A Polish Perspective. Int J Environ Res Public Health. 2021;18(16):8608. doi:10.3390/ijerph18168608.
60.
Zawierucha J, Prystacki T, Marcinkowski W, et al. How COVID-19 Outbreak Influenced Transplantation in Poland. J Clin Med. 2023;12(2):461. doi:10.3390/jcm12020461.
61.
Czerwiński J, Antoszkiewicz K, Woderska-Jasińska A, et al. The Current Status of Organ Donation and Transplantation in Poland. Poltransplant Activity. Transplant Proc. 2022;54(4):837–847. doi:10.1016/j.transproceed.2022.02.053.
62.
Karolak W, Woźniak-Grygiel E, Łącka M, et al. A Single-Center Experience with Lung Transplants During the COVID-19 Pandemic. Ann Transplant. 2021;26:e929946. doi:10.12659/AOT.929946.
63.
Manla Y, Badarin FA, Bader N, et al. Worldwide and Country-Specific Impact of the COVID-19 Pandemic on Heart Transplantation Volumes: A Longitudinal Analysis of 2020 and 2021. Curr Probl Cardiol. 2023;48(11):101870. doi:10.1016/j.cpcardiol.2023.101870.
64.
Kucap M, Nadolny K, Ładny JR. Retrospective analysis of interventions performed by emergency medical teams in poland before and during the sars cov-2 pandemic. Wiad Lek. 2020;73(8):1659–1662. PMID: 33055329.
65.
Nadolny K, Ładny JR, Zyśko D, et al. Interventions of emergency medical teams in Poland during the SARS-CoV-2 pandemic. Kardiol Pol. 2021;79(1):72–75. doi:10.33963/KP.15632.
66.
Nogueira RG, Qureshi MM, Abdalkader M, et al. SVIN COVID-19 Global Stroke Registry; SVIN COVID-19 Global Stroke Registry. Global Impact of COVID-19 on Stroke Care and IV Thrombolysis. Neurology. 2021;96(23):e2824-e2838. doi:10.1212/WNL.0000000000011885.
67.
Marto JP, Strambo D, Ntaios G, et al. Global COVID-19 Stroke Registry. Safety and Outcome of Revascularization Treatment in Patients With Acute Ischemic Stroke and COVID-19: The Global COVID-19 Stroke Registry. Neurology. 2023;100(7):e739-e750. doi:10.1212/WNL.0000000000201537.
68.
SVIN COVID-19 Global SAH Registry. Global impact of the COVID-19 pandemic on subarachnoid haemorrhage hospitalisations, aneurysm treatment and in-hospital mortality: 1-year follow-up. J Neurol Neurosurg Psychiatry. 2022:jnnp-2022–329200. doi:10.1136/jnnp-2022-329200.
69.
Mularczyk-Tomczewska P, Zarnowski A, Gujski M, et al. Barriers to accessing health services during the COVID-19 pandemic in Poland: A nationwide cross-sectional survey among 109,928 adults in Poland. Front Public Health. 2022;10:986996. doi:10.3389/fpubh.2022.986996.
70.
Mularczyk-Tomczewska P, Żarnowski A, Gujski M, et al. Preventive Health Screening during the COVID-19 Pandemic: A Cross-Sectional Survey among 102,928 Internet Users in Poland. J Clin Med. 2022;11(12):3423. doi:10.3390/jcm11123423.
71.
Kościelecka KE, Kuć AJ, Kubik DM, et al. Impact of the covid-19 pandemic on the availability of medical care among oncological patients. Wiad Lek. 2021;74(7):1542–1551. PMID: 34459750.
72.
Kludacz-Alessandri M, Walczak R, Hawrysz L, et al. The Quality of Medical Care in the Conditions of the COVID-19 Pandemic, with Particular Emphasis on the Access to Primary Healthcare and the Effectiveness of Treatment in Poland. J Clin Med. 2021;10(16):3502. doi:10.3390/jcm10163502.
73.
Mazurek J, Biernat K, Kuciel N, et al. The Use of Medical and Non-Medical Services by the Elderly during the SARS-CoV-2 Pandemic Differs between General and Specialist Practice: A One-Center Study in Poland. Healthcare (Basel). 2020;9(1):8. doi:10.3390/healthcare9010008.
74.
Dalewski B, Palka L, Kiczmer P, et al. The Impact of SARS-CoV-2 Outbreak on the Polish Dental Community's Standards of Care-A Six-Month Retrospective Survey-Based Study. Int J Environ Res Public Health. 2021;18(3):1281. doi:10.3390/ijerph18031281.
75.
Tysiąc-Miśta M, Dziedzic A. The Attitudes and Professional Approaches of Dental Practitioners during the COVID-19 Outbreak in Poland: A Cross-Sectional Survey. Int J Environ Res Public Health. 2020;17(13):4703. doi:10.3390/ijerph17134703.
76.
Rajwa P, Przydacz M, Zapała P, et al. How has the COVID-19 pandemic impacted Polish urologists? Results from a national survey. Cent European J Urol. 2020;73(3):252–259. doi:10.5173/ceju.2020.0252.
77.
Stefura T, Rymarowicz J, Wysocki M, et al. Surgical care in Poland after COVID-19 outbreak: a national survey. Folia Med Cracov. 2020;60(3):33–51. doi:10.24425/fmc.2020.135794.
78.
Kokoszka-Bargieł I, Cyprys P, Rutkowska K, et al. Intensive Care Unit Admissions During the First 3 Months of the COVID-19 Pandemic in Poland: A Single-Center, Cross-Sectional Study. Med Sci Monit. 2020 Sep 26;26:e926974. doi:10.12659/MSM.926974.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.