Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Obiektywne metody diagnostyki zespołu bólu mięśniowo-powięziowego
1
Szkoła Doktorska Śląskiego Uniwersytetu Medycznego w Katowicach, Polska
2
Śląski Uniwersytet Medyczny w Katowicach, Wydział Nauk o Zdrowiu w Katowicach, Katedra Fizjoterapii, Zakład Medycyny Fizykalnej, Polska
Autor do korespondencji
Tomasz Piętka
Szkoła Doktorska Śląskiego Uniwersytet Medycznego w Katowicach, ul. Medyków 12, 40-752, Katowice, Polska
Szkoła Doktorska Śląskiego Uniwersytet Medycznego w Katowicach, ul. Medyków 12, 40-752, Katowice, Polska
Med Og Nauk Zdr. 2021;27(4):387-394
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
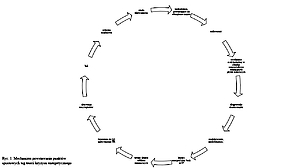
Zespół bólu mięśniowo-powięzio-wego (ang. myofascial pain syndrome, MPS) to istotny problem kliniczny, który pomimo licznych doniesień naukowych po-zostaje nadal nie w pełni wyjaśniony. Dotyczy to szczególnie zagadnień związanych z patomechanizmem oraz tworzeniem standardów diagnostycznych i terapeutycznych. W praktyce klinicznej do najczęściej stosowanych metod rozpoznawania MPS zalicza się badanie palpacyjne. Niemniej jednak bada-nie to obarczone jest ryzykiem dużego błędu. W związku z powyższym podczas diagnostyki MPS potrzeba rzetelnych, powtarzalnych pomiarów, które powinny charakteryzować się wysoką czułością, aby umożliwić wykrycie klinicznie ważnych zmian. Celem artykułu jest przegląd obiektywnych metod diagnostycznych istotnych dla prawidłowego rozpoznania MPS.
Opis stanu wiedzy:
Postęp medycyny klinicznej zależy od umiejętności dokładnego diagnozowania choroby i bezstronnej oceny efektów leczenia. Wydaje się zatem kluczowe opracowanie skutecznych, obiektywnych metod diagnozowania MPS. Obecnie brak jest konsensusu wśród klinicystów dotyczącego schematu diagnostycznego MPS.
Podsumowanie:
Najbardziej rzetelnym badaniem wydaje się badanie palpacyjne wykonane przez doświadczonego terapeutę. Następnie ustalając na jego podstawie kryteria diagnostyczne D.G. Simonsa wraz z podparciem diagnozy za pomocą jednego z obiektywnych narzędzi oceniających zmiany w tkance mięśniowej sugerujące obecność punktu spustowego.
Zespół bólu mięśniowo-powięzio-wego (ang. myofascial pain syndrome, MPS) to istotny problem kliniczny, który pomimo licznych doniesień naukowych po-zostaje nadal nie w pełni wyjaśniony. Dotyczy to szczególnie zagadnień związanych z patomechanizmem oraz tworzeniem standardów diagnostycznych i terapeutycznych. W praktyce klinicznej do najczęściej stosowanych metod rozpoznawania MPS zalicza się badanie palpacyjne. Niemniej jednak bada-nie to obarczone jest ryzykiem dużego błędu. W związku z powyższym podczas diagnostyki MPS potrzeba rzetelnych, powtarzalnych pomiarów, które powinny charakteryzować się wysoką czułością, aby umożliwić wykrycie klinicznie ważnych zmian. Celem artykułu jest przegląd obiektywnych metod diagnostycznych istotnych dla prawidłowego rozpoznania MPS.
Opis stanu wiedzy:
Postęp medycyny klinicznej zależy od umiejętności dokładnego diagnozowania choroby i bezstronnej oceny efektów leczenia. Wydaje się zatem kluczowe opracowanie skutecznych, obiektywnych metod diagnozowania MPS. Obecnie brak jest konsensusu wśród klinicystów dotyczącego schematu diagnostycznego MPS.
Podsumowanie:
Najbardziej rzetelnym badaniem wydaje się badanie palpacyjne wykonane przez doświadczonego terapeutę. Następnie ustalając na jego podstawie kryteria diagnostyczne D.G. Simonsa wraz z podparciem diagnozy za pomocą jednego z obiektywnych narzędzi oceniających zmiany w tkance mięśniowej sugerujące obecność punktu spustowego.
Introduction and objective:
The myofascial pain syndrome (MPS) is an important clinical problem which, despite numerous scientific reports, remains not fully understood. This refers in particular to unclearly stated pathomechanism and undefined diagnostic and therapeutic standards. In daily clinical practice, palpation is the most commonly applied method of myofascial pain syndrome diagnostics. However, this may be associated with inaccurate diagnosis. Therefore, the diagnosis of myofascial pain syndrome requires reliable, repeatable measurements which should be characterized by high sensitivity in order to detect clinically important changes. The aim of this study is to review the objective diagnostic methods essential for the correct diagnosis of myofascial pain syndrome.
Brief description of the state of knowledge:
The progress of clinical medicine depends on the ability to accurately diagnose the disease and objectively assess the effects of the treatment. Therefore, it seems crucial to develop effective, objective methods for diagnosing myofascial pain syndrome. Currently, there is no consensus among clinicians regarding the myofascial pain syndrome diagnostic procedure.
Conclusion:
Manual palpation performed by an experienced physiotherapist seems to be the most reliable examination, followed by establishing the Simons’ diagnostic criteria on its basis, together with supporting the diagnosis using one of the objective tools assessing changes in muscle tissue suggesting the presence of trigger points.
The myofascial pain syndrome (MPS) is an important clinical problem which, despite numerous scientific reports, remains not fully understood. This refers in particular to unclearly stated pathomechanism and undefined diagnostic and therapeutic standards. In daily clinical practice, palpation is the most commonly applied method of myofascial pain syndrome diagnostics. However, this may be associated with inaccurate diagnosis. Therefore, the diagnosis of myofascial pain syndrome requires reliable, repeatable measurements which should be characterized by high sensitivity in order to detect clinically important changes. The aim of this study is to review the objective diagnostic methods essential for the correct diagnosis of myofascial pain syndrome.
Brief description of the state of knowledge:
The progress of clinical medicine depends on the ability to accurately diagnose the disease and objectively assess the effects of the treatment. Therefore, it seems crucial to develop effective, objective methods for diagnosing myofascial pain syndrome. Currently, there is no consensus among clinicians regarding the myofascial pain syndrome diagnostic procedure.
Conclusion:
Manual palpation performed by an experienced physiotherapist seems to be the most reliable examination, followed by establishing the Simons’ diagnostic criteria on its basis, together with supporting the diagnosis using one of the objective tools assessing changes in muscle tissue suggesting the presence of trigger points.
Piętka T, Onik G, Knapik K, Sieroń K. Obiektywne metody diagnostyki zespołu bólu mięśniowo-powięziowego. Med Og Nauk Zdr. 2021; 27(4):
387–394. doi: 10.26444/monz/136573
REFERENCJE (85)
1.
Fleckenstein J, Zaps D, Rüger L, et al. Discrepancy between preva-lence and perceived effectiveness of treatment methods in myofascial pain syndrome: Results of a cross-sectional, nationwide survey. BMC Musculoskel Disord. 2010; 11: 32. https://doi:10.1186/1471-2474-....
2.
Weller JL, Comeau D, Otis JAD. Myofascial Pain. Semin Neurol. 2018; 38(6): 640–643. https://doi:10.1055/s-0038-167....
3.
Skootsky SA, Jaeger B, Oye RK. Prevalence of myofascial pain in general internal medicine practice. West J Med. 1989; 151(2): 157–60.
4.
Simons DG. Clinical and etiological update of myofascial pain from trigger points. J Musc Pain. 1996; 4: 93–122.
5.
Lucas N, Macaskill P, Les I, et al. Reliability of Physical Examination for Diagnosis of Myofascial Trigger Points. Clin J Pain. 2009; 25(1): 80–89. https://doi:10.1097/AJP.0b013e....
6.
Fricton JR. Myofascial pain of the head and neck: diagnosis and mana-gement. J Back Musculoskeletal Rehabil. 1996; 6: 177–194.
7.
Simons DG. Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J Electromyogr Kinesiol. 2004; 14(1): 95–107. https://doi:10.1016/j.jelek in.2003.09.018.
8.
Gerwin RD. Myofascial Trigger Point Pain Syndromes. Semin Neurol. 2016; 36(5): 469–473. https://doi:10.1055/s-0036-158....
9.
Cummings M, Baldry P. Regional myofascial pain: diagnosis and ma-nagement. Best Pract Res Clin Rheumatol. 2007; 21: 367–387. https://doi:10.1016/j.berh.200....
10.
Gerwin RD, Dommerholt J, Shah JP. An Expansion of Simons’ Integra-ted Hypothesis of Trigger Point Formation. Curr Pain Headache Rep. 2004; 8: 468–475. https://doi:10.1007/s11916-004....
11.
Hocking MJL. Exploring the Central Modulation Hypothesis: Do Ancient Memory Mechanisms Underlie the Pathophysiology of Trigger Points? Curr Pain Headache Rep. 2013; 17(7): 347. https://doi:10.1007/s11916-013....
12.
Shah JP, Thaker N, Heimur J, et al. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PMR. 2015; 7: 746–761. https://doi:10.1016/j.pmrj.201....
13.
Buchmann J, Neustadt B, Buchmann-Barthel K. Objective measurement of tissue tension in myofascial trigger point areas before and during the administration of anesthesia with complete blocking of neuromuscular transmission. Clin J Pain. 2014; 30(3): 191–198. https://doi:10.1097/AJP.0b013e....
14.
Gerwin RD. Diagnosing fibromyalgia and myofascial pain syndrome. J Fam Pract. 2013; 62(12): 19–25.
15.
Borg-Stein J, Iaccarino MA. Myofascial pain syndrome treatments. Phys Med Rehabil Clin N Am. 2014; 25(2): 357–74. https://doi:10.1016/j.pmr.2014....
16.
Srbely JZ, Kumbhare D, Grosman-Rimon LA. Narrative review of new trends in the diagnosis of myofascial trigger points: diagnostic ultraso-und imaging and biomarkers. J Can Chiropr Assoc. 2016; 60(3): 220–225.
17.
Tough EA, White AR, Richards S. Variability of criteria used to diag-nose myofascial trigger point pain syndrome – evidence from a review of the literature. Clin J Pain. 2007; 23(3): 278–86. https://doi:10.1097/AJ P. 0 b 013 e 318 0 2 f d a 7c.
18.
Chiarotto A, Clijsen R, Fernandez-de-las-Penas C, et al. Prevalence of myofascial trigger points in spinal disorders: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2016; 97(3): 16–37. https://doi:10.1016/j.apmr.201....
19.
Grosman-Rimon L, Clarkec H, Chan AK, et al. Clinicians’ perspective of the current diagnostic criteria for myofascial pain syndrome. J Back Musculoskelet Rehabil. 2017; 30: 509–514.
20.
Fernández-de-las-Peñas C, Dommerholt J. International consensus on diagnostic criteria and clinical considerations of myofascial trig-ger points: A delphi study. Pain Medicine. 2018; 19: 142–150. https://doi:10.1093/pm/pnx 207.
21.
Giamberardino MA, Affaitati G, Fabrizio A. Myofascial pain syndro-mes and their evaluation. Best Pract Res Clin Rheumatol. 2011; 25(2): 185–198. https://doi:10.1016/j.berh.201....
22.
Quintner JL, Bove GM, Cohen ML. A critical evaluation of the trig-ger point phenomenon. Rheumatology. 2015; 54: 392–399. https://doi:10.1093/rheumatolo....
23.
Rozenfeld E, Finestone AS, Moran U, et al. Test-retest reliability of myofascial trigger point detection in hip and thigh areas. J Bodyw Mov Ther. 2017; 21(4): 914–919. https://doi:10.1016/j.jbmt.201....
24.
Mayoral del Moral O, Torres Lacomba M, Russell I J, et al. Validity and Reliability of Clinical Examination in the Diagnosis of Myofascial Pain Syndrome and Myofascial Trigger Points in Upper Quarter Muscles. Pain Med. 2018; 19(10): 2039–2050. https://doi:10.1093/pm/pnx315.
25.
Watt-Watson J, Peter E, Clark AJ, et al. The ethics of Canadian entry--to-practice pain competencies: how are we doing? Pain Res Manag. 2013; 18: 25–32.
26.
Mora-Relucio R, Núñez-Nagy S, Gallego-Izquierdo T, et al. Expe-rienced versus Inexperienced Interexaminer Reliability on Location and Classification of Myofascial Trigger Point Palpation to Diagnose Lateral Epicondylalgia: An Observational Cross-Sectional Study. J Evid Based Complementary Altern Med. 2016; 2016: 6059719. https://doi.org/10.1155/2016/6....
27.
Myburgh C, Lauridsen HH, Larsen AH. Standardized manual palpa-tion of myofascial trigger points in relation to neck/shoulder pain; the influence of clinical experience on inter-examiner reproducibility. Man Ther. 2011; 16(2): 136–140.
28.
Barbero M, Bertoli P, Cescon C, et al. Intra-rater reliability of an expe-rienced physiotherapist in locating myofascial trigger points in upper trapezius muscle. J Man Manip Ther. 2012; 20(4): 171–177.
29.
Dong Wook R, Ji Cheol S, Yong Kyun K. Detecting Local Twitch Re-sponses of Myofascial Trigger Points in the Lower-Back Muscles Using Ultrasonography. Arch Phys Med Rehabil. 2011; 92(10): 1576–1580.
30.
Myburgh C, Holsgaard LA, Hartvigsen J. A Systematic, Critical Re-view of Manual Palpation for Identifying Myofascial Trigger Points: Evidence and Clinical Significance. Arch Phys Med Rehabil. 2008; 89(6): 1169–1176.
31.
Zale KE, Klatt M, Volz KR, et al. A mixed-method approach to evalu-ating the association between myofascial trigger points and ankle/foot pain using handheld sonography equipment: a pilot study. J Diagn Med Sonogr. 2015; 31: 210–220.
32.
Sikdar S, Shah JP, Gebreab T, et al. Novel applications of ultrasound technology to visualize and characterize myofascial trigger points and surrounding soft tissue. Arch Phys Med Rehabil. 2009; 90: 1829–1838.
33.
Cheatham SW, Kolber MJ, Mokha GM, et al. Concurrent validation of a pressure pain threshold scale for individuals with myofascial pain syndrome and fibromyalgia. J Man Manip Ther. 2018; 26(1): 25–35. https://doi:10.1080/10669817.2....
34.
Giburm P, Chan Woo K, Si Bog P. Reliability and Usefulness of the Pressure Pain Threshold Measurement in Patients with Myofascial Pain. Ann Rehabil Med. 2011; 35(3): 412–417.
35.
Liew B, Lee HY, Rügamer D, et al. A novel metric of reliability in pres-sure pain threshold measurement. Sci Rep. 2021; 11: 6944. https://doi.org/10.1038/s41598....
36.
Mense S. Muscle Pain: Mechanisms and Clinical Significance. Dtsch Arztebl Int. 2008; 105(12): 214–219. doi:10.3238/artzebl.2008.0214.
37.
Hong CZ, Chen YN, Twehous DA, et al. Pressure threshold for referred pain by compression on the trigger point and adjacent areas. J Muscu-loskelet Pain. 1996; 4: 61–79.
38.
Ziaeifar M, Massoud Arab A, Karimi N, et al. The effect of dry need-ling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J Bodyw Mov Ther. 2014; 18(2): 298–305.
39.
Jerez-Mayorga D, Dos Anjos CF, Macedo MC, et al. Instrumental va-lidity and intra/inter-rater reliability of a novel low-cost digital pressure algometer. Peer J. 2020; 12(8): e10162. https://doi:10.7717/peerj.
40.
Linde Lukas D, Kumbhare D, Joshi Maneil DA, et al. The relationship between rate of algometer application and pain pressure threshold in the assessment of myofascial trigger point sensitivity. Pain Pract. 2018; 18(2): 224–229.
41.
Park G, Kim C, Park S, et al. Reliability and usefulness of the pressure pain threshold measurement in patients with myofascial pain. Ann Rehabil Med. 2011; 35(3): 412–7. https://doi:10.5535/arm.2011.3....
42.
Bernhardt O, Schiffman E, Look J. Reliability and validity of a new fin-gertip-shaped pressure algometer for assessing pressure pain thresholds in the temporomandibular joint and masticatory muscles. J Orofac Pain. 2007; 21(1): 29–38.
43.
Jafari M, Bahrpeyma F, Mokhtari-Dizaji M, et al. Novel method to measure active myofascial trigger point stiffness using ultrasound imaging. J Bodyw Mov Ther. 2018; 22(2): 374–378. https://doi:10.1016/j.jbmt.201....
44.
Kumbhare D, Singh D, Rathbone A, et al. Ultrasound-guided interven-tional procedures: myofascial trigger points with structured literature review. Reg Anesth Pain Med. 2017; 42(3): 407–412. https://doi:10.1097/AAP.000000....
45.
Da Silva AC, Aily JB, Oliveira AB. Interrater and intrarater reliability and minimum detectable change of ultrasound for active myofascial trigger points in upper trapezius muscle in individuals with shoulder pain. J Manipulative Physiol Ther. 2020; 43(9): 855–863.
46.
Kisha T, Shankar H. Targeting myofascial taut bands by ultrasound topical collection on myofascial pain. Curr Pain Headache Rep. 2013; 17(7): 1–4. https://doi:10.1007/s11916-013....
47.
Parthasarathy S, Charles S. Analgesic Efficacy of Ultrasound Iden-tified Trigger Point Injection in Myofascial Pain Syndrome: A Pilot Study in Indian Patients. Indian J Pain 2016; 30(3): 162–165. https://doi:10.4103/0970-5333.....
48.
Jasti N, Bista S, Bhargav H, et al. Medical Applications of Infrared Thermography: A Narrative Review. Infrared Phys Technol. 2019; 14(1): 35–53.
49.
Dibai-Filho A, Guirro E, Ferreira V, et al. Reliability of different me-thodologies of infrared image analysis of myofascial trigger points in the upper trapezius muscle. Braz J Phys Ther. 2015; 19(2):122–128.
50.
Shah JP, Gilliams EA. Uncovering the biochemical milieu of myofascial trigger points using in vivo microdialysis: An application of muscle pain concepts to myofascial pain syndrome. J Bodyw Mov Ther. 2008; 12(4): 371–384. https://doi:10.1016/j.jbmt.200....
51.
Costa A, Dibai Filho A, Packer AC, et al. Intra and inter-rater reliability of infrared image analysis of masticatory and upper trapezius muscles in women with and without temporomandibular disorder. Braz J Phys Ther. 2013; 17(1): 24–31. https://doi:10.1590/s1413-3555....
52.
Cojocaru MC, Cojocaru IM, Voiculescu VM, et al. Trigger points--ultrasound and thermal findings. J Med Life. 2015; 8(3): 315–318.
53.
Magalhães MF, Dibai-Filho A, de Oliveira Guirro EC. Evolution of Skin Temperature after the Application of Compressive Forces on Tendon, Muscle and Myofascial Trigger Point. PLOS ONE 2015; 10(6): e0129034. https://doi.org/10.1371/journa....
54.
Girasol CE, Dibai-Filho A, de Oliveira AK, de Jesus Guirro RR. Cor-relation Between Skin Temperature Over Myofascial Trigger Points in the Upper Trapezius Muscle and Range of Motion, Electromyographic Activity, and Pain in Chronic Neck Pain Patients. J Manipulative Physiol Ther. 2018; 41(4): 350–357. https://doi:10.1016/j.jmpt.201....
55.
Dibai-Filho A, Roberto de Jesus Guirro R. Evaluation of myofascial trigger points using infrared thermography: a critical review of the literature. J Manipulative Physiol Ther. 2015; 38(1): 86–92. https://doi:10.1016/j.jmpt.201....
56.
Altindiş T, Güngörmüş M. Thermographic evaluation of occlusal splint and low level laser therapy in myofascial pain syndrome. Complement Ther Med. 2019; 44: 277–281. https://doi:10.1016/j.ctim.201....
57.
Onik G, Kasprzyk T, Knapik K, et al. Myofascial Trigger Points Therapy Modifies Thermal Map of Gluteal Region. Biomed Res Int. 2020; Article ID 4328253, 7 pages. https://doi:10.1155/2020/43282....
58.
Andonian BJ, Masi AT, Aldag JC, et al. Greater Resting Lumbar Extensor Myofascial Stiffness in Younger Ankylosing Spondylitis Patients Than Age-Comparable Healthy Volunteers Quantified by Myotonometry. Arch Phys Med Rehabil. 2015; 96(11): 2041–2047. https://doi:10.1016/j.apmr.201....
59.
Bizzini M, Mannion AF. Reliability of a new, hand-held device for assessing skeletal muscle stiffness. Clin Biomech. 2003; 18(5): 459–461. https://doi:10.1016/s0268-0033....
60.
Jiménez-Sánchez C, Ortiz-Lucas M, Bravo-Esteban E, et al. Myoto-nometry as a Measure to Detect Myofascial Trigger Points: An Inter--Rater Reliability Study. Physiol Meas. 2018; 26; 39(11): 115004. https://doi:10.1088/1361-6579/....
61.
Liu CL, Feng N, Zhang HQ, et al. Assessing the viscoelastic properties of upper trapezius muscle: Intra-and inter-tester reliability and the effect of shoulder elevation. J Electromyogr Kinesiol. 2018; 43: 226–229. https://doi:10.1016/j.jelek in.2017.09.007.
62.
Marusiak J, Jaskólska A, Koszewicz M, et al. Myometry revealed medication-induced decrease in resting skeletal muscle stiffness in Parkinson's disease patients. Clin Biomech. 2012; 27(6): 632–635. https://doi:10.1016/j.clinbiom....
63.
Chuang L, Wu C, Lin K, et al. Quantitative mechanical properties of the relaxed biceps and triceps brachii muscles in patients with subacute stroke: a reliability study of the Myoton-3 myometer. Stroke Res Treat. 2012; 2012: 617694. https://doi:10.1155/2012/61769....
64.
Ge JS, Chang TT, Zhang ZJ. Reliability of Myotonometric Measurement of Stiffness in Patients with Spinal Cord Injury. Med Sci Monit. 2020; 28(26): e924811. https:// doi: 10.12659/MSM.924811.
65.
Nair K, Masi AT, Andonian BJ, et al. Stiffness of resting lumbar myofascia inhealthy young subjects quantified using a handheld myotonometer and concurrently with surface electromyography monitoring. J Bodyw Mov Ther. 2016; 20(2): 388–396. https://doi: 10.1016/j.jbmt.2015.12.005.
66.
Wytrążek M, Huber J, Lipiec J, et al. Evaluation of palpation, pressure algometry, and electromyography for monitoring trigger points in young participants. J Manipulative Physiol Ther. 2015; 38(3): 232–243. https://doi:10.1016/j.jmpt.201....
67.
Hun Yu S, Jin Kim H. Electrophysiological characteristics according to activity level of myofascial trigger points. J Phys Ther Sci. 2015; 27(9): 2841–2843. https://doi:10.1589/jpts.27.28....
68.
Ge HY, Monterde S, Graven-Nielsen T, et al. Latent myofascial trigger points are associated with an increased intramuscular electromyograp-hic activity during synergistic muscle activation. J Pain. 2014; 15(2): 181–187. https://doi:10.1016/j.jpain.20....
69.
Couppe CH, Midttun A, Hilden J, et al. Spontaneous Needle Electro-myographic Activity in Myofascial Trigger Points in the Infraspinatus Muscle: A Blinded Assessment. J Musculoskelet Pain. 2001; 9(3): 7–16. https://doi:10.1300/J094v09n03....
70.
Meekin GD, So Y, Quan D. American Association of Neuromuscular & Electrodiagnostic Medicine evidence-based review: use of surface elec-tromyography in the diagnosis and study of neuromuscular disorders. Muscle Nerve. 2008; 38(4): 1219–1224. https://doi:10.1002/mus.21055.
71.
Rubin DI. Needle electromyography: Basic concepts. Handb Clin Neurol. 2019; 160: 243–256. https://doi: 10.1016/B978-0-444-64032-1.00016-3.
72.
Hong CZ, Simons DG. Pathophysiologic and electrophysiologic me-chanisms of myofascial trigger points. Arch Phys Med Rehabil. 1998; 79: 863–872. https://doi:10.1016/s0003-9993....
73.
Feng LP, Schmidt JE, De Leeuw R. Inability of surface electromyography to register the local twitch response elicited by trigger point injection and snapping palpation in myofascial pain patients. J Muscoskelet Pain. 20 08; 16(3):165 –173. https://doi:10.1080/1058245080....
74.
Chen Q, Bensamoun S, Basford J, et al. Identification and Quantifica-tion of Myofascial Taut Bands with Magnetic Resonance Elastography. Arch Phys Med Rehabil. 2007; 88(12): 1658–1661. https://doi:10.1016/j.apmr.200....
75.
Chen Q, Basford J, An KN. Ability of magnetic resonance elastograp-hy to assess taut bands. Clin Biomech. 2008; 23(5): 623–629. https://doi:10.1016/j.clinbiom....
76.
Chen Q, Wang HJ, Gay RE, et al. Quantification of Myofascial Taut Bands. Arch Phys Med Rehabil. 2016; 97(1): 67–73. https://doi:10.1016/j.apmr.201....
77.
Shah JP, Phillips TM, Danoff JV, et al. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J Appl Physiol. 2005; 99(5): 1977–84. https://doi:10.1152/japplphysi....
78.
Simons DG. Review of Microanalytical in vivo study of biochemical milieu of myofascial trigger points. J Bodyw Mov Ther. 2006; 10(1): 10–11. https://doi:10.1016/j.jbmt.200....
79.
Moraska AF, Hickner RC, Kohrt WM, et al. Changes in Blood Flow and Cellular Metabolism at a Myofascial Trigger Point with Trigger Point Release (Ischemic Compression): A Proof-of-Principle Pilot Study. Arch Phys Med Rehabil. 2013; 94(1): 196–200. https://doi:10.1016/j.apmr.201....
80.
Garra BS. Elastography: current status, future prospects, and making it work for you. Ultrasound Q. 2011; 27(3): 177–86. https://doi:10.1097/RUQ.0b013e....
81.
Brandenburg JE, Eby SF, Song P, et al. Ultrasound Elastography: The New Frontier in Direct Measurement of Muscle Stiffness. Arch Phys Med Rehabil. 2014; 95(11): 2207–19. https://doi:10.1016/j.apmr.201....
82.
Sikdar S, Turo D, Otto P, et al. Ultrasound Imaging and Elastography for Characterizing Muscle Tissue in Myofascial Pain Syndrome. PM&R. 2013; 5(9): 133-S133. https://doi:10.1016/j.pmrj.201....
83.
Ling G, Chen Z, Ding-Ding Z, et al. Application of shear wave elasto-graphy in the evaluation of neck-shoulder myofascial pain syndrome. Zhongguo Gu Shang. 2016; 29(2): 142–145.
84.
Calvo-Lobo C, Diez-Vega I, Martínez-Pascual B, et al. Tensiomyography, sonoelastography, and mechanosensitivity differences between active, latent, and control low back myofascial trigger points. Medicine. 2017; 96(10): e6287.https://doi:10.1097/MD.0000000...
85.
Bird M, Shah J, Gerber L, et al. Characterization of local muscle fiber anisotropy using shear wave elastography in patients with chronic myofascial pain. Ann Rehabil Med. 2018; 61: 13-e13.
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.