Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Najczęstsza etiologia zapaleń płuc wśród dzieci hospitalizowanych w Uniwersyteckim Szpitalu Dziecięcym w Lublinie w latach 2010–2020
1
Department of Paediatric Pulmonology and Rheumatology, Medical University, Lublin, Poland
2
I Chair and Department of Cardiology, Medical University, Warsaw, Poland
Autor do korespondencji
Małgorzata Wieteska
Lung Disease and Child Rheumatology Clinic, Medical University of Lublin, University Children’s Hospital, 20-093 Lublin, Poland
Lung Disease and Child Rheumatology Clinic, Medical University of Lublin, University Children’s Hospital, 20-093 Lublin, Poland
Med Og Nauk Zdr. 2022;28(2):157-164
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Zapalenie płuc, definiowane jako ostra infekcja miąższu płuc o zróżnicowanej etiologii, pozostaje wiodącą przyczyną zachorowalności i śmiertelności wśród pacjentów pediatrycznych na całym świecie. Celem pracy jest przybliżenie najczęstszej etiologii zapaleń płuc wśród dzieci hospitalizowanych w Uniwersyteckim Szpitalu Dziecięcym w Lublinie w latach 2010–2020.
Materiał i metody:
Badaniem retrospektywnym objęto 2250 pacjentów w wieku od 2 do 227 miesięcy, hospitalizowanych z powodu zapaleń płuc w latach 2010–2020 w Klinice Chorób Płuc i Reumatologii Dziecięcej Uniwersyteckiego Szpitalu Dziecięcego w Lublinie. Elektroniczna dokumentacja medyczna stanowiła źródło wszystkich danych dotyczących pacjentów. Zgodnie z Międzynarodową Klasyfikacją Chorób ICD-10, ze względu na etiologię zapaleń płuc, pacjenci zostali podzieleni na 20 grup. Zebrane dane posłużyły następnie do obliczeń statystycznych.
Wyniki:
Zaobserwowano sezonowość zachorowalności na zapalenia płuc ze zwiększoną liczbą zakażeń w zimie. Bazując na Klasyfikacji Chorób ICD-10, stwierdzono, że najczęstszą etiologią zapaleń płuc była etiologia bakteryjna nieokreślona (rozpoznanie J15.9), leżąca u podstaw 30,2% wszystkich przypadków. Ponadto na podstawie diagnostyki serologicznej stwierdzono, że najczęściej wykrywanym patogenem związanym z rozwojem zapaleń płuc u dzieci była bakteria Mycoplasma pneumoniae (18,8% wszystkich przypadków). Średni czas hospitalizacji pacjentów wynosił 7,4 dnia, podczas gdy najczęściej stosowanym antybiotykiem była amoksycylina + kwas klawulanowy. Badania obrazowe klatki piersiowej wykonano u 88,8% pacjentów.
Zapalenie płuc, definiowane jako ostra infekcja miąższu płuc o zróżnicowanej etiologii, pozostaje wiodącą przyczyną zachorowalności i śmiertelności wśród pacjentów pediatrycznych na całym świecie. Celem pracy jest przybliżenie najczęstszej etiologii zapaleń płuc wśród dzieci hospitalizowanych w Uniwersyteckim Szpitalu Dziecięcym w Lublinie w latach 2010–2020.
Materiał i metody:
Badaniem retrospektywnym objęto 2250 pacjentów w wieku od 2 do 227 miesięcy, hospitalizowanych z powodu zapaleń płuc w latach 2010–2020 w Klinice Chorób Płuc i Reumatologii Dziecięcej Uniwersyteckiego Szpitalu Dziecięcego w Lublinie. Elektroniczna dokumentacja medyczna stanowiła źródło wszystkich danych dotyczących pacjentów. Zgodnie z Międzynarodową Klasyfikacją Chorób ICD-10, ze względu na etiologię zapaleń płuc, pacjenci zostali podzieleni na 20 grup. Zebrane dane posłużyły następnie do obliczeń statystycznych.
Wyniki:
Zaobserwowano sezonowość zachorowalności na zapalenia płuc ze zwiększoną liczbą zakażeń w zimie. Bazując na Klasyfikacji Chorób ICD-10, stwierdzono, że najczęstszą etiologią zapaleń płuc była etiologia bakteryjna nieokreślona (rozpoznanie J15.9), leżąca u podstaw 30,2% wszystkich przypadków. Ponadto na podstawie diagnostyki serologicznej stwierdzono, że najczęściej wykrywanym patogenem związanym z rozwojem zapaleń płuc u dzieci była bakteria Mycoplasma pneumoniae (18,8% wszystkich przypadków). Średni czas hospitalizacji pacjentów wynosił 7,4 dnia, podczas gdy najczęściej stosowanym antybiotykiem była amoksycylina + kwas klawulanowy. Badania obrazowe klatki piersiowej wykonano u 88,8% pacjentów.
Introduction and objective:
Pneumonia is defined as an acute infection of the lung parenchyma caused by various pathogens. It remains a leading cause of morbidity and mortality in the paediatric population globally. The aim of this study was to disclose most common aetiology of pneumonia among children hospitalized in the University Children’s Hospital in Lublin, Poland, from 2010–2020.
Material and methods:
This retrospective study included 2,250 patients in the age rage from 2–227 months, hospitalized in the Department of Paediatric Pulmonology and Rheumatology of University Children’s Hospital in Lublin from 2010–2020 due to pneumonia. All necessary information were obtained from electronic medical records. According to the International Classification of Diseases Version 10 (ICD-10), patients were divided into 20 groups in terms of aetiology of pneumonia. Subsequently collected data were submitted to statistical calculations.
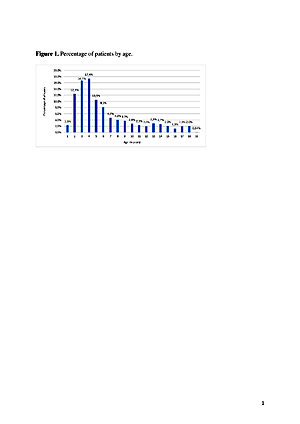
Results:
A seasonality of pneumonia admissions was observed with predominance in the winter. Based on ICD-10 codes, the most common aetiology of pneumonia was unspecified bacterial pneumonia (J15.9) related with 30.2% of all cases. Moreover, based on IgM serology tests, Mycoplasma pneumoniae was the main identified pathogen (18.8% of all cases). Average duration of hospitalization oscillated around 7.4 days; the most common administered antibiotic was amoxicillin + clavulanic acid. Chest imaging was performed in 88.8% of patients.
Conclusions:
Pneumonia dominated in the bacterial aetiology of children. Younger groups of children were more prone to the development of pneumonia. In many casus, there were observed difficulties with the identification of an exact pathogen.
Pneumonia is defined as an acute infection of the lung parenchyma caused by various pathogens. It remains a leading cause of morbidity and mortality in the paediatric population globally. The aim of this study was to disclose most common aetiology of pneumonia among children hospitalized in the University Children’s Hospital in Lublin, Poland, from 2010–2020.
Material and methods:
This retrospective study included 2,250 patients in the age rage from 2–227 months, hospitalized in the Department of Paediatric Pulmonology and Rheumatology of University Children’s Hospital in Lublin from 2010–2020 due to pneumonia. All necessary information were obtained from electronic medical records. According to the International Classification of Diseases Version 10 (ICD-10), patients were divided into 20 groups in terms of aetiology of pneumonia. Subsequently collected data were submitted to statistical calculations.
Results:
A seasonality of pneumonia admissions was observed with predominance in the winter. Based on ICD-10 codes, the most common aetiology of pneumonia was unspecified bacterial pneumonia (J15.9) related with 30.2% of all cases. Moreover, based on IgM serology tests, Mycoplasma pneumoniae was the main identified pathogen (18.8% of all cases). Average duration of hospitalization oscillated around 7.4 days; the most common administered antibiotic was amoxicillin + clavulanic acid. Chest imaging was performed in 88.8% of patients.
Conclusions:
Pneumonia dominated in the bacterial aetiology of children. Younger groups of children were more prone to the development of pneumonia. In many casus, there were observed difficulties with the identification of an exact pathogen.
Wieteska M, Maj D, Wacławska M, Wawryk-Gawda E. Most common aetiology of pneumonia among children hospitalized in the University
Children’ s Hospital in Lublin, Poland, 2010–2020. Med Og Nauk Zdr. 2022; 28(2): 157–164. doi: 10.26444/monz/150668
REFERENCJE (33)
1.
Mackenzie G. The definition and classification of pneumonia. Pneumonia (Nathan). 2016; 8: 14. https://doi.org/10.1186/s41479....
2.
Mathew JL. Etiology of Childhood Pneumonia: What We Know, and What We Need to Know. Indian J Pediatr. 2018; 85(1): 25–34. https://doi.org/10.1007/s12098....
3.
Ramjith J, Roes KCB, Zar HJ, et al. Flexible modelling of risk factors on the incidence of pneumonia in young children in South Africa using piece-wise exponential additive mixed modelling. BMC Med Res Methodol. 2021; 21(1): 17. https://doi.org/10.1186/s12874...
4.
Fadl N, Ashour A, Yousry Muhammad Y. Pneumonia among underfive children in Alexandria, Egypt: a case-control study. J Egypt Public Health Assoc. 2020; 95(1): 14. https://doi.org/10.1186/s42506...- 00043-0.
5.
Hoang VT, Dao TL, Minodier P, et al. Risk Factors for Severe Pneumonia According to WHO 2005 Criteria Definition Among Children <5 Years of Age in Thai Binh, Vietnam: A Case-Control Study. J Epidemiol Glob Health. 2019; 9(4): 274–280. https://doi.org/10.2991/jegh.k....
6.
Rodrigues CMC, Groves H. Community-Acquired Pneumonia in Children: the Challenges of Microbiological Diagnosis. J Clin Microbiol. 2018; 56(3): e01318–17. https://doi.org/10.1128/JCM.01....
7.
Lange J, Kozielski, J, Bartolik, K, et al. The incidence of pneumonia in the paediatric population in Poland in light of the maps of health needs. J Public Health. 2021; 73: 1–9. https://doi.org/10.1007/s10389....
8.
Jain V, Vashisht R, Yilmaz G, et al. Pneumonia Pathology. StatPearls http://www.statpearls.com/Arti... (access: 2021.08.04).
9.
Horsky J, Drucker EA, Ramelson HZ. Accuracy and Completeness of Clinical Coding Using ICD-10 for Ambulatory Visits. AMIA Annu Symp Proc. 2018; 2017: 912–920.
10.
Kasundriya SK, Dhaneria M, Mathur A, et al. Incidence and Risk Factors for Severe Pneumonia in Children Hospitalized with Pneumonia in Ujjain, India. Int J Environ Res Public Health. 2020; 17(13): 4637. https:// doi.org/10.3390/ijerph17134637.
11.
Orimadegun AE, Adepoju AA, Myer L. A Systematic Review and Metaanalysis of Sex Differences in Morbidity and Mortality of Acute Lower Respiratory Tract Infections Among African Children. J Pediatr Rev. 2020; 8(2): 65–78. https://doi.org/10.32598/jpr.8....
12.
Lange J, Kozielski J, Bartolik K, et al. Analysis of the incidence of acute respiratory diseases in the paediatric population in Poland in the light of the „Health Needs Map”. Adv Respir Med. 2020; 88(3): 204–214. https://doi.org/10.5603/ARM.20....
13.
Lee CH, Won YK, Roh EJ, et al. A nationwide study of children and adolescents with pneumonia who visited Emergency Department in South Korea in 2012. Clin Exp Pediatr. 2016; 59(3): 132–138. https:// doi.org/10.3345/kjp.2016.59.3.132.
14.
Wen Z, Wei J, Xue H, et al. Epidemiology, microbiology, and treatment patterns of pediatric patients hospitalized with pneumonia at two hospitals in China: a patient chart review study. Ther Clin Risk Manag. 2018; 14: 501–510. https://doi.org/10.2147/TCRM.S....
15.
Tannous R, Haddad RN, Torbey PH. Management of Community- Acquired Pneumonia in Pediatrics: Adherence to Clinical Guidelines. Front Pediatr. 2020; 8: 302. https://doi.org/10.3389/fped.2....
16.
González-Coquel S, Escamilla-Arrieta J, Coronell-Rodriguez W, et al. Severity factors of Acquired Pneumonia Community in a children’s hospital in the Colombian Caribbean. Salud Uninorte. 2018; 34(2): 302–314. https://doi.org/10.14482/sun.3....
17.
Gajewska M, Lewtak K, Scheres J, et al. Trends in Hospitalization of Children with Bacterial Pneumonia in Poland. Cent Eur J Public Health. 2016; 24(3): 188–192. https://doi.org/10.21101/cejph....
18.
Mantero M, Tarsia P, Gramegna A, et al. Antibiotic therapy, supportive treatment and management of immunomodulation-inflammation response in community acquired pneumonia: review of recommendations. Multidiscip Respir Med. 2017; 12: 1–19. https://doi. org/10.1186/s40248-017-0106-3.
19.
Nguyen PT, Tran HT, Fitzgerald DA, et al. Antibiotic use in children hospitalised with pneumonia in Central Vietnam. Arch Dis Child. 2020; 105(8): 713–719. https://doi.org/10.1136/archdi....
20.
Mathur S, Fuchs A, Bielicki J, et al. Antibiotic use for communityacquired pneumonia in neonates and children: WHO evidence review. Paediatr Int Child Health. 2018; 38(1): 66–75. https://doi.org/10.1080/ 20469047.2017.1409455.
21.
Nguyen PTK, Tran HT, Fitzgerald DA, et al. Characterisation of children hospitalised with pneumonia in central Vietnam: a prospective study. Eur Respir J. 2019; 54(1): 1802256. https://doi.org/10.1183/139930...- 2018.
22.
Sulley S, Ndanga M. Pediatric pneumonia: An analysis of cost & outcome influencers in the United States. Int J Pediatr Adolesc Med. 2019; 6(3): 79–86. https://doi.org/10.1016/j.ijpa....
23.
Hammitt LL, Murdoch DR, Scott JA, et al. Specimen collection for the diagnosis of pediatric pneumonia. Clin Infect Dis. 2012; 54(2): 132–139. https://doi.org/10.1093/cid/ci....
24.
Shim JY. Current perspectives on atypical pneumonia in children. Clin Exp Pediatr. 2020; 63(12): 469–476. https://doi.org/10.3345/ cep.2019.00360.
25.
Meyer Sauteur PM, Unger WW, Nadal D, et al. Infection with and Carriage of Mycoplasma pneumoniae in Children. Front Microbiol. 2016; 7: 329. https://doi.org/10.3389/fmicb.....
26.
Chen JR, Zhou XF. A retrospective survey of Chlamydia pneumoniae infection rates in paediatric patients from a single centre in Wuxi, China. J Int Med Res. 2020; 48(10): 1–5. https://doi.org/10.1177/030006....
27.
Fulová M, Kotrbancová M, Bražinová A, et al. Legionnaires› Disease in Pediatric Patients, Control Measures and 5-Year Follow-up. Pediatr Infect Dis J. 2020; 39(11): 990–994. https://doi.org/10.1097/ INF.0000000000002781.
28.
O’Grady KAF, Torzillo, PJ, Frawley K, et al. The radiological diagnosis of pneumonia in children. Pneumonia (Nathan). 2014; 5(1): 38–51. https://doi.org/10.15172/pneu.....
29.
Liszewski MC, Görkem S, Sodhi KS, et al. Lung magnetic resonance imaging for pneumonia in children. Pediatr Radiol. 2017; 47(11): 1420– 1430. https://doi.org/10.1007/s00247....
30.
Andronikou S, Lambert E, Halton J, et al. Guidelines for the use of chest radiographs in community-acquired pneumonia in children and adolescents. Pediatr Radiol. 2017; 47(11): 1405–1411. https://doi. org/10.1007/s00247-017-3944-4.
31.
Andronikou S, Goussard P, Sorantin E. Computed tomography in children with community-acquired pneumonia. Pediatr Radiol. 2017; 47(11): 1431–1440. https://doi.org/10.1007/s00247....
32.
Stadler JAM, Andronikou S, Zar HJ. Lung ultrasound for the diagnosis of community-acquired pneumonia in children. Pediatr Radiol. 2017; 47(11): 1412–1419. https://doi.org/10.1007/s00247...
33.
Franquet T. Imaging of Community-acquired Pneumonia. J Thorac Imaging. 2018; 33(5): 282–294. https://doi.org/10.1097/ RTI.0000000000000347.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.