Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Wpływ stomii jelitowej na obraz ciała i funkcje seksualne
1
Department of Reproductive Health and Sexology. Department of Women's Health, Medical University of Silesia, Katowice, Poland
Autor do korespondencji
Wiktoria Paszyńska
Zakład Zdrowia Reprodukcyjnego i Seksuologii. Katedra Zdrowia Kobiety, Śląski Uniwersytet Medyczny w Katowicach.
Zakład Zdrowia Reprodukcyjnego i Seksuologii. Katedra Zdrowia Kobiety, Śląski Uniwersytet Medyczny w Katowicach.
Med Og Nauk Zdr. 2025;31(1):33-39
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Pomimo że stomia umożliwia pacjentom dłuższe i bardziej produktywne życie, to stomicy mogą cierpieć z powodu dolegliwości fizjologicznych, psychoseksualnych oraz społecznych. Duża grupa osób z wyłonioną przetoką jelitową zmaga się z problemami typu: wzdęcia, nieprzyjemny zapach i wyciek treści kałowej, zmiana obrazu ciała. Zaburzenia te mogą prowadzić do izolacji, nasilonego lęku oraz obniżenia samooceny, co negatywnie wpływa na życie seksualne. Badania dotyczące wpływu stomii jelitowej na obraz ciała i funkcje seksualne pozostają ograniczone. Celem pracy była ocena wpływu stomii jelitowej na obraz ciała oraz jakość życia seksualnego stomików
Materiał i metody:
Dane zebrano od 89 pacjentów ze stomią. Do ich pozyskania i oceny wykorzystano Formularz Identyfikacji Pacjenta, Skalę Oceny Ciała (BES), Indeks Funkcji Seksualnych Kobiet (FSFI) i Międzynarodowy Indeks Funkcji Erekcji (IIEF).
Wyniki:
Analiza wykazała, że mężczyźni, którzy nie zostali poddani chemioterapii lub radioterapii po operacji raka jelita grubego, mieli znacznie wyższe wyniki funkcji erekcji niż ci, którzy przeszli terapię uzupełniającą. Kobiety, które otrzymały leczenie uzupełniające, wykazały znacznie niższe poziomy pożądania seksualnego w porównaniu z kobietami, które nie otrzymały tego typu leczenia.
Wnioski:
Wyniki tego badania pokazują, że u pacjentów ze stomią występują zaburzenia funkcji seksualnych związane z leczeniem uzupełniającym oraz zaburzenia obrazu ciała, które wpływają na funkcje seksualne.
Pomimo że stomia umożliwia pacjentom dłuższe i bardziej produktywne życie, to stomicy mogą cierpieć z powodu dolegliwości fizjologicznych, psychoseksualnych oraz społecznych. Duża grupa osób z wyłonioną przetoką jelitową zmaga się z problemami typu: wzdęcia, nieprzyjemny zapach i wyciek treści kałowej, zmiana obrazu ciała. Zaburzenia te mogą prowadzić do izolacji, nasilonego lęku oraz obniżenia samooceny, co negatywnie wpływa na życie seksualne. Badania dotyczące wpływu stomii jelitowej na obraz ciała i funkcje seksualne pozostają ograniczone. Celem pracy była ocena wpływu stomii jelitowej na obraz ciała oraz jakość życia seksualnego stomików
Materiał i metody:
Dane zebrano od 89 pacjentów ze stomią. Do ich pozyskania i oceny wykorzystano Formularz Identyfikacji Pacjenta, Skalę Oceny Ciała (BES), Indeks Funkcji Seksualnych Kobiet (FSFI) i Międzynarodowy Indeks Funkcji Erekcji (IIEF).
Wyniki:
Analiza wykazała, że mężczyźni, którzy nie zostali poddani chemioterapii lub radioterapii po operacji raka jelita grubego, mieli znacznie wyższe wyniki funkcji erekcji niż ci, którzy przeszli terapię uzupełniającą. Kobiety, które otrzymały leczenie uzupełniające, wykazały znacznie niższe poziomy pożądania seksualnego w porównaniu z kobietami, które nie otrzymały tego typu leczenia.
Wnioski:
Wyniki tego badania pokazują, że u pacjentów ze stomią występują zaburzenia funkcji seksualnych związane z leczeniem uzupełniającym oraz zaburzenia obrazu ciała, które wpływają na funkcje seksualne.
Introduction and objective:
The aim of the study was to assess the body image and sexual functioning of patients with a stoma.
Material and methods:
Data were collected from 89 stoma patients. The Patient Identification Form, Body Esteem Scale (BES), Female Sexual Function Index (FSFI), and International Index of Erectile Function (IIEF) were used to compile and evaluate data
Results:
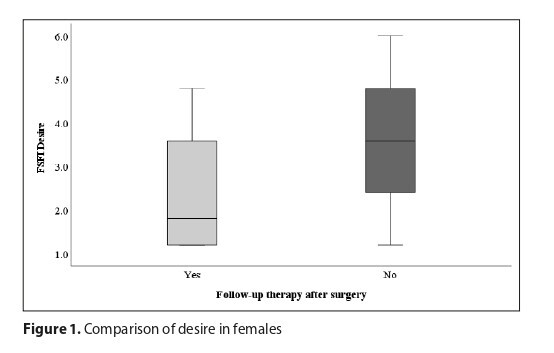
The analysis revealed that men who had not been subjected to chemotherapy or radiotherapy after colorectal cancer surgery had significantly higher erectile function scores than men who had undergone the follow-up therapy (p =.033, r = 0.37). Women who had received a follow-up treatment showed significantly lower levels of sexual desire in comparison with women who had not received this type of treatment (p =.006, r = 0.47).
Conclusions:
The results show that patients with a stoma experience sexual dysfunction related to adjuvant treatment and body image disorders that affect sexual functions.
The aim of the study was to assess the body image and sexual functioning of patients with a stoma.
Material and methods:
Data were collected from 89 stoma patients. The Patient Identification Form, Body Esteem Scale (BES), Female Sexual Function Index (FSFI), and International Index of Erectile Function (IIEF) were used to compile and evaluate data
Results:
The analysis revealed that men who had not been subjected to chemotherapy or radiotherapy after colorectal cancer surgery had significantly higher erectile function scores than men who had undergone the follow-up therapy (p =.033, r = 0.37). Women who had received a follow-up treatment showed significantly lower levels of sexual desire in comparison with women who had not received this type of treatment (p =.006, r = 0.47).
Conclusions:
The results show that patients with a stoma experience sexual dysfunction related to adjuvant treatment and body image disorders that affect sexual functions.
Paszyńska W, Zborowska K, Skrzypulec-Plinta V. Influence of intestinal stoma on body image and sexual functioning. Med Og Nauk Zdr.
2025; 31(1): 33–39. doi: 10.26444/monz/200813
REFERENCJE (32)
1.
García-Rodríguez T, Barreiro-Trillo A, Seijo-Bestilleiro R, González-Martin C. Sexual Dysfunction in Ostomized Patients: A Systematized Review. Healthcare. 2021;9(5):520.
2.
Jayarajah U, Samarasekera DN. Psychological Adaptation to Alteration of Body Image among Stoma Patients: A Descriptive Study. Indian J Psychol Med. 2017;39(1):63–68.
3.
Kiliç E, Taycan O, Belli AK, Ozmen M. The effect of permanent ostomy on body image, self-esteem, marital adjustment, and sexual functioning. Turk Psikiyatri Derg. 2007;18:302–10.
4.
Song L, Han X, Zhang J, Tang L. Body image mediates the effect of stoma status on psychological distress and quality of life in patients with colorectal cancer. Psychooncology. 2020;29(4):796–802.
5.
Aktas D, Gocman Baykara Z. Body Image Perceptions of Persons With a Stoma and Their Partners: A Descriptive, Cross-sectional Study. Ostomy Wound Manage. 2015;61(5):26–40.
6.
Petersén C, Carlsson E. Life with a stoma-coping with daily life: Experiences from focus group interviews. Journal of clinical nursing, 2021;30(15–16):2309–2319.
7.
MacDonald S, Wong LS, John-Charles R, McKee T, Quasim T, Moug S. The impact of intestinal stoma formation on patient quality of life after emergency surgery-A systematic review. Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland. 2023;25(7):1349–1360.
8.
Persson E, Hellström AL. Experiences of Swedish men and women 6 to 12 weeks after ostomy surgery. J Wound Ostomy Continence Nurs. 2002;29(2):103–8.
9.
Brown H, Randle J. Living with a stoma: a review of the literature. J Clin Nurs. 2005;14(1):74–81.
10.
Saracco C, Rastelli G, Roveron G, Ferrara F. Sexual Function in Patients with Stoma and its Consideration Among Their Caregivers: A Cross-Sectional Study. Sex Disabil. 2019;37:415–427.
11.
Ayaz-Alkaya S. Overview of psychosocial problems in individuals with stoma: A review of literature. Int Wound J. 2019;16(1):243–249.
12.
Sörensson M, Asplund D, Matthiessen P, et al. Self-reported sexual dysfunction in patients with rectal cancer. Colorectal Dis. 2020;22(5):500–512.
13.
Sutsunbuloglu E, Vural F. Evaluation of Sexual Satisfaction and Function in Patients Following Stoma Surgery: A Descriptive Study. Sex Disabil. 2018;36:349–361.
14.
Gozuyesil E, Taylan S, Manav AI. The Evaluation of Self-Esteem and Sexual Satisfaction of Patients with Bowel Stoma in Turkey. Sexuality and Disability. 2017;35(2):157.
15.
Ma S, Knapp P, Galdas P. ‘My sexual desires, everything, my normal life just stops’; a qualitative study of male sexual health in inflammatory bowel disease. J Clin Nurs. 2024;33(10):4034–4047.
16.
Yilmaz E, Çelebi D, Kaya Y, Baydur H. A Descriptive, Cross-sectional Study to Assess Quality of Life and Sexuality in Turkish Patients with a Colostomy. Ostomy Wound Manage. 2017;63(8):22–29.
17.
Altschuler A, Ramirez M, Grant M, Wendel C, Hornbrook MC, Herrinton L, Krouse RS. The influence of husbands’ or male partners’ support on women’s psychosocial adjustment to having an ostomy resulting from colorectal cancer. J Wound Ostomy Continence Nurs. 2009;36(3):299–305.
18.
Manderson L. Boundary breaches: the body, sex, and sexuality after stoma surgery. Soc Sci Med. 2005;61:405–415.
19.
Thyø A, Laurberg S, Emmertsen KJ. Impact of bowel and stoma dysfunction on female sexuality after treatment for rectal cancer. Colorectal Dis. 2020;22(8):894–905.
20.
Lin S, Yin G, Chen L. The sexuality experience of stoma patients: a meta-ethnography of qualitative research. BMC Health Serv Res. 2023;23(1):489.
21.
Reese JB, Porter LS, Somers TJ, Keefe FJ. Pilot feasibility study of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. J Sex Marital Ther. 2012;38:402–417.
22.
Marijnen CA, van de Velde CJ, Putter H, van den Brink M, Maas CP, Martijn H, Rutten HJ, Wiggers T, Kranenbarg EK, Leer JW. Stiggelbout AM. Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol. 2005;23(9):1847–58.
23.
Bruheim K, Tveit KM, Skovlund E, Balteskard L, Carlsen E, Fosså SD, Guren MG. Sexual function in females after radiotherapy for rectal cancer. Acta Oncol. 2010;49(6):826–32.
24.
Thyø A, Elfeki H, Laurberg S, Emmertsen KJ. Female sexual problems after treatment for colorectal cancer – a population-based study. Colorectal Dis. 2019;21(10):1130–1139.
25.
Albaugh JA, Tenfelde S, Hayden DM. Sexual Dysfunction and Intimacy for Ostomates. Clin. Colon Rectal Surg. 2017;30:201–216.
26.
DuHamel K, Schuler T, Nelson C, et al. The sexual health of female rectal and anal cancer survivors: results of a pilot randomized psycho-educational intervention trial. J Cancer Surviv. 2016;10(3):553–563.
27.
Fakhrian K, Sauer T, Dinkel A, Klemm S, Schuster T, Molls M, Geinitz H. Chronic adverse events and quality of life after radiochemotherapy in anal cancer patients. A single institution experience and review of the literature. Strahlenther Onkol. 2013;189(6):486–94.
28.
Knowles G, Haigh R, McLean C, Phillips H. Late effects and quality of life after chemo-radiation for the treatment of anal cancer. Eur J Oncol Nurs. 2015;19(5):479–85.
29.
Ball M, Nelson CJ, Shuk E, Starr TD, Temple L, Jandorf L, Schover L, Mulhall JP, Woo H, Jennings S, DuHamel K. Men’s experience with sexual dysfunction post-rectal cancer treatment: a qualitative study. J Cancer Educ. 2013;28(3):494–502.
30.
Sheng Z. Psychological consequences of erectile dysfunction. Trends in Urology & Men’s Health, 2021;12.
31.
Milbury K, Cohen L, Jenkins R, Skibber JM, Schover LR. The association between psychosocial and medical factors with long-term sexual dysfunction after treatment for colorectal cancer. Support Care Cancer. 2013;21(3):793–802.
32.
Benedict C, Philip EJ, Baser RE, Carter J, Schuler TA, Jandorf L, DuHamel K, Nelson C. Body image and sexual function in women after treatment for anal and rectal cancer. Psychooncology. 2016;25(3):316–23.
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.