RESEARCH PAPER
Improvement in patient and medical staff safety by using telemedicine capabilities in cardiology
1
Faculty of Medicine, Lazarski University, Warsaw, Poland
2
Central Clinical Hospital of the Ministry of Interior and Administration, Warsaw, Poland
Med Og Nauk Zdr. 2022;28(4):322-325
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Cardiovascular diseases are the leading cause of death in Poland and worldwide. Medical services together with telemedicine provide complex health care for patients with cardiovascular diseases. The aim of this study is to analyze the use of telemedicine options for reimbursed cardiac services between 2018–2021.
Material and methods:
From the database of the National Health Fund (the sole public payer of health services), teleconsultations between primary care physicians (PCPs, specialists, stationary consultations of primary care physicians with a cardiologist, and hybrid cardiac telerehabilitation were identified. Analysis was based on the number, age and gender of patients, as well as p;rovincial health centres.
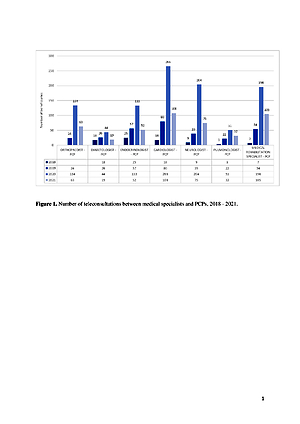
Results:
The largest number of teleconsultations of primary care physicians were with acardiologists, accounting for 25% of telemedicine consultations, 96% of which involved patients living in an area with 5–10 000 healthcare beneficiaries. Only 21% of all consultations between the primary care physicians and the cardiologists were stationary consultations. Hybrid cardiac telerehabilitation involved patients from 13 provincial centres (VCs), with the highest number of services recorded in the 60–64 age group.
Conclusions:
Telemedicine services are the main means of consultation between specialists and primary care. physicians. An increasing trend in the use of hybrid cardiac telerehabilitation was found.
Cardiovascular diseases are the leading cause of death in Poland and worldwide. Medical services together with telemedicine provide complex health care for patients with cardiovascular diseases. The aim of this study is to analyze the use of telemedicine options for reimbursed cardiac services between 2018–2021.
Material and methods:
From the database of the National Health Fund (the sole public payer of health services), teleconsultations between primary care physicians (PCPs, specialists, stationary consultations of primary care physicians with a cardiologist, and hybrid cardiac telerehabilitation were identified. Analysis was based on the number, age and gender of patients, as well as p;rovincial health centres.
Results:
The largest number of teleconsultations of primary care physicians were with acardiologists, accounting for 25% of telemedicine consultations, 96% of which involved patients living in an area with 5–10 000 healthcare beneficiaries. Only 21% of all consultations between the primary care physicians and the cardiologists were stationary consultations. Hybrid cardiac telerehabilitation involved patients from 13 provincial centres (VCs), with the highest number of services recorded in the 60–64 age group.
Conclusions:
Telemedicine services are the main means of consultation between specialists and primary care. physicians. An increasing trend in the use of hybrid cardiac telerehabilitation was found.
REFERENCES (26)
1.
Lustig TA and Institute of Medicine (U.S.). The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary. NCBI https://www.ncbi.nlm.nih.gov/b... (access: 2022.08.05).
2.
Wolfe A. Institute of Medicine report: crossing the quality chasm: a new health care system for the 21st century.Policy, Politics, & Nursing Practice. 2001; 2(3): 233–235. https://doi.org/10.1177/152715.... [Google Scholar].
3.
World Health Organization. Cardiovascular diseases. https://www-whoint. translate.goog/en/news-room/fact-sheets/detail/cardiovasculardiseases-(cvds)?_x_tr_sl=auto&_x_tr_tl=pl&_x_tr_hl=pl (access 2022.08.05).
4.
Lopez AD, et al., editors. Global Burden of Disease and Risk Factors. Open Knowledge Repository https://openknowledge.worldban... (access: 2022.08.07).
5.
Gaziano TA. Reducing the growing burden of cardiovascular disease in the developing world. Health Aff (Millwood). 2007;26(1):13–24. https://doi.org/10.1377/hlthaf... [Google Scholar].
6.
Główny Urząd Statystyczny. Umieralność w 2021 roku. Zgodny według przyczyn. https://stat.gov.pl/obszary-te...- wstepne,10,3.html (access: 2022.08.08).
7.
Narodowy Fundusz Zdrowia. Telekonsultacja kardiologiczna i geriatryczna finansowana przez NFZ. https://www.nfz.gov.pl/ aktualnosci/aktualnosci-centrali/telekonsultacja-kardiologiczna-igeriatryczna- finansowana-przez-nfz,6758.html (access: 2022.08.08).
8.
Rozporządzenie Ministra Zdrowia z dnia 16 grudnia 2016 r. zmieniające rozporządzenie w sprawie świadczeń gwarantowanych z zakresu rehabilitacji leczniczej. ISAP https://isap.sejm.gov.pl/isap.... DocDetails.xsp?id=WDU20160002162 (access: 2022.08.05).
9.
Ganapathy K, Das S, Reddy S, et al. Digital Health Care in Public Private Partnership Mode. Telemed J E Health. 2021. 27(12):1363–1371. https://doi.org/10.1089/tmj.20... [Google Scholar].
10.
Sood SP, Negash S, Mbarika VW, et al. Differences in public and private sector adoption of telemedicine: Indian case study for sectoral adoption.In: Westbrook JI, Coiera EW, editors. Information Technologyin Health Care 2007. Stud Health Technol Inform. 2007. p. 257–268. [Google Scholar].
11.
Jegier A, Szalewska D, Mawlichanów A, et al. Comprehensive cardiac rehabilitation as the keystone in the secondary prevention of cardiovascular disease. Kardiol Pol. 2021; 79(7–8): 901–916. https://doi. org/10.33963/KP.a2021.0066 [Google Scholar].
12.
Piotrowicz E. How to do: telerehabilitation in heart failure patients. Cardiol J. 2012. 19(3): 243–248, https://doi.org/10.5603/cj.201... [Google Scholar].
13.
Piotrowicz E, Piepoli MF, Jaarsma T, et al. Telerehabilitation in heart failure patients: the evidence and the pitfalls. Int J Cardiol. 2016. 220: 408–413, https://doi.org/10.1016/j.ijca... [Google Scholar].
14.
Raport „Top Disruptors in Healthcare 2022”. GOV https://www.gov.pl/ web/rpp/raport-top-disruptors-in-healthcare-2022 (access: 2022.08.10).
15.
Gajarawala SN, Pelkowski JN. Telehealth Benefits and Barriers. J Nurse Pract. 2021. 17(2):218–221. https://doi.org/10.1016/j.nurp... [Google Scholar].
16.
Daragó L, Jung Z, Ispán F, et al. A telemedicina előnyei és hátrányai [Benefits and disadvantages of telemedicine]. Orv Hetil. 2013.154(30):1167–71. https://doi.org/10.1556/OH.201... [Google Scholar]
17.
Mubaraki AA, Alrabie AD, Sibyani AK, et al. Advantages and disadvantages of telemedicine during the COVID-19 pandemic era among physicians in Taif, Saudi Arabia. Saudi Med J. 2021. 42(1):110– 115. https://doi.org/10.15537/smj.2....
18.
Furlepa K, Śliwczyński A, Kamecka K, et al. The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. Journal of Personalized Medicine. 2022; 12(7):1165. https:// doi.org/10.3390/jpm12071165 [Google Scholar].
19.
Furlepa, K, Tenderenda, A, Kozłowski, R, et al. Recommendations for the Development of Telemedicine in Poland Based on the Analysis of Barriers and Selected Telemedicine Solutions. Int J Environ Res Public Health. 2022; 19(3): 1221. https://doi.org/10.3390/ijerph... [Google Scholar].
20.
Barrios V, Cosin-Sales J, Bravo M, et al. Telemedicine consultation for the clinical cardiologists in the era of COVID-19: present and future. Consensus document of the Spanish Society of Cardiology. Rev Esp Cardiol (Engl Ed). 2020; 73(11): 910–918. https://doi.org/10.1016/j. rec.2020.06.032 [Google Scholar].
21.
Sytuacja zdrowotna ludności Polski i jej uwarunkowania – raport za 2020 rok. Narodowy Instytut Zdrowia Publicznego. https://www. pzh.gov.pl/sytuacja-zdrowotna-ludnosci-polski-i-jej-uwarunkowaniaraport- za-2020-rok/ (access: 2022.08.15).
22.
Zarządzenie nr 63/2015/DSOZ prezesa narodowego funduszu zdrowia z dnia 30 września 2015 r. Zmieniające zarządzenie w sprawie określenia warunków zawierania i realizacji umów w rodzaju świadczenia zdrowotne kontraktowane odrębnie. NFZ https://www.nfz.gov. pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-632015dsoz,6410.html (access:2022.08.15).
23.
Korzeniowska-Kubacka I, Dobraszkiewicz-Wasilewska B, Bilińska M, et al. Two models of early cardiac rehabilitation in male patients after myocardial infarction with preserved left ventricular function: comparison of standard out-patient versus hybrid training programmes. Kardiol Pol. 2011. 69(3): 220–226. [Google Scholar].
24.
Piotrowicz E, Pencina MJ, Opolski G, et al. Effects of a 9-week hybrid comprehensive telerehabilitation program on long-term outcomes in patients with heart failure: the telerehabilitation in heart failure patients (TELEREH-HF) randomized clinical trial. JAMA Cardiol. 2020; 5(3): 300–308. https://doi.org/10.1001/jamaca... [Google Scholar].
25.
Piotrowicz R, Krzesiński P, Balsam P, et al. Cardiology telemedicine solutions opinion of the experts of the Committee of Informatics and Telemedicine of Polish Society of Cardiology, Section of Non-invasive Electrocardiology and Telemedicine of Polish Society of Cardiology and Clinical Sciences C [article in Polish]. Kardiol Pol. 2018. 76(3): 698–707, https://doi.org/10.5603/KP.a20... [Google Scholar].
26.
Hybrydowa telerehabilitacja kardiologiczna bliżej pacjentów. Puls Medycyny. https://pulsmedycyny.pl/hybryd...- blizej-pacjentow-1121670 (access: 2022.08.15).
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.