RESEARCH PAPER
Humanization of medicine from the perspective of physicians in Poland
1
Katedra Biomedycznych Podstaw Rozwoju i Seksuologii, Wydział Pedagogiczny, Uniwersytet Warszawski, Polska
2
Katedra Humanizacji Medycyny i Seksuologii, Collegium Medicum, Uniwersytet Zielonogórski, Polska
Corresponding author
Alicja Kozakiewicz
Katedra Humanizacji Medycyny i Seksuologii, Collegium Medicum, Uniwersytet Zielonogórski, 65-046, Zielona Góra, Polska
Katedra Humanizacji Medycyny i Seksuologii, Collegium Medicum, Uniwersytet Zielonogórski, 65-046, Zielona Góra, Polska
Med Og Nauk Zdr. 2023;29(1):29-35
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Humanism in care is of fundamental importance in improving the level of medical services and maintaining a proper relationship between medical staff and patients, while appropriate communication is one of the determinants of increased patient satisfaction. The aim of the study is identification of key indicators of the concept of humanization of medicine from the perspective of male and female physicians, and determination of their communication skills resources by gender.
Material and methods:
A survey conducted during February – April 2022 included 498 physicians – 48.6% (N=242) of males and 52.4% (N=256) of females who declared that they work with patients on a daily basis. The respondents’ mean age was 48.3 (SD = 12.5). The survey used a question relating to the most important aspects in everyday work with patients designed by the research team, and the Health Professionals Communication Skills Scale (HP-CSS).
Results:
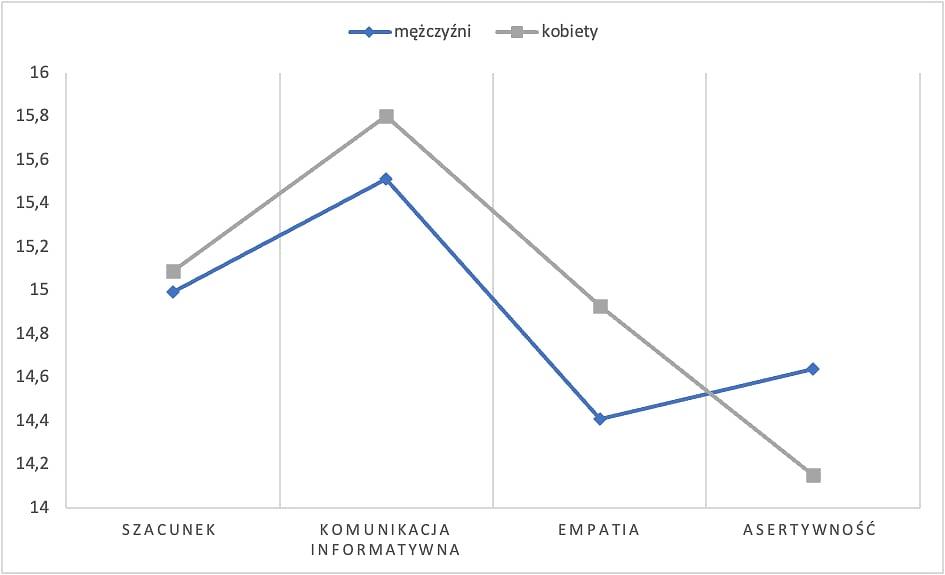
Among the most important components in working with patients were carefulness and precision of the actions performed (47.6%), clear and understandable communication (44.2%) and an individual approach to the patient (40.4%). Differences in the area of the dimensions of communication skills indicate that male and female physicians do not differ in terms of respect expressed to patients (p = 0.512). Significantly higher scores were obtained by female physicians in the area of empathy (p = 0.004), while males achieved higher scoresin the area of assertiveness (p = 0.029).
Conclusions:
The results of the study carry implications for both the teaching staff and those working in the health care sector emphasizing the importance of developing communication competencies, while planning activities taking into consideration gender differences remains important.
Humanism in care is of fundamental importance in improving the level of medical services and maintaining a proper relationship between medical staff and patients, while appropriate communication is one of the determinants of increased patient satisfaction. The aim of the study is identification of key indicators of the concept of humanization of medicine from the perspective of male and female physicians, and determination of their communication skills resources by gender.
Material and methods:
A survey conducted during February – April 2022 included 498 physicians – 48.6% (N=242) of males and 52.4% (N=256) of females who declared that they work with patients on a daily basis. The respondents’ mean age was 48.3 (SD = 12.5). The survey used a question relating to the most important aspects in everyday work with patients designed by the research team, and the Health Professionals Communication Skills Scale (HP-CSS).
Results:
Among the most important components in working with patients were carefulness and precision of the actions performed (47.6%), clear and understandable communication (44.2%) and an individual approach to the patient (40.4%). Differences in the area of the dimensions of communication skills indicate that male and female physicians do not differ in terms of respect expressed to patients (p = 0.512). Significantly higher scores were obtained by female physicians in the area of empathy (p = 0.004), while males achieved higher scoresin the area of assertiveness (p = 0.029).
Conclusions:
The results of the study carry implications for both the teaching staff and those working in the health care sector emphasizing the importance of developing communication competencies, while planning activities taking into consideration gender differences remains important.
REFERENCES (43)
1.
Håkansson Eklund J, Holmström IK, Kumlin T, et al. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ Couns. 2019;102(1):3–11. doi:10.1016/j.pec.2018.08.029.
2.
Shapiro J, Coulehan J, Wear D, et al. Medical humanities and their discontents: definitions, critiques, and implications. Acad Med. 2009;84(2):192–198. doi:10.1097/ACM.0b013e3181938bca.
3.
Arnott R, Bolton G, Evans M, et al. Proposal for an academic Association for Medical Humanities. Med Humanit. 2001;27(2):104–105. doi:10.1136/mh.27.2.104.
4.
Izdebski Z (red.) Debata Humanizacja Medycyny 2015, 2022, Warszawa: Wydawnictwa Uniwersytetu Warszawskiego, 2022, s. 99.- ISBN: 9788323557289.
5.
Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303(6814):1385–1387. doi:10.1136/bmj.303.6814.1385.
6.
Izdebski Z, Mazur J, Furman-Kwiatkowska K, i wsp. Humanizacja procesu leczenia i komunikacji klinicznej pomiędzy pacjentem a personelem medycznym przed i w czasie pandemii COVID-19. Wydawnictwa Uniwersytetu Warszawskiego, Warszawa 2023 (w druku).
7.
Keeney T, Kumar A, Erler KS, et al. Making the Case for Patient-Reported Outcome Measures in Big-Data Rehabilitation Research: Implications for Optimizing Patient-Centered Care. Arch Phys Med Rehabil. 2022;103(5):S140-S145. doi:10.1016/j.apmr.2020.12.028.
8.
González-Bueno J, Sevilla-Sánchez D, Puigoriol-Juvanteny E, et al. Improving medication adherence and effective prescribing through a patient-centered prescription model in patients with multimorbidity. Eur J Clin Pharmacol. 2022;78(1):127–137. doi:10.1007/s00228–021–03207–9.
9.
Tebeje TH, Klein J. Applications of e-Health to Support Person-Centered Health Care at the Time of COVID-19 Pandemic. Telemed J E Health. 2021;27(2):150–158. doi:10.1089/tmj.2020.0201.
10.
Nagamatsu Y, Natori Y, Yanai H, et al. Impact of a nursing education program about caring for patients in Japan with malignant pleural mesothelioma on nurses’ knowledge, difficulties and attitude: A randomized control trial. Nurse Educ Today. 2014;34(7):1087–1093. doi:10.1016/j.nedt.2014.02.007.
11.
Brédart A, Kop JL, Fiszer C, et al. Breast cancer survivors’ perceived medical communication competence and satisfaction with care at the end of treatment. Psycho-oncology. 2015;24:1670–1678. doi: 10.1002/pon.3836.
12.
van Osch M, van Dulmen S, van Vliet L, et al. Specifying the effects of physician’s communication on patients’ outcomes: A randomised controlled trial. Patient Educ Couns. 2017;100:1482–1489. doi: 10.1016/j.pec.2017.03.009.
13.
Rosenstein AH, O’Daniel M. A survey of the impact of disruptive behaviors and communication defects on patient safety. J Comm J Qual Saf. 2008;34:464–471. doi: 10.1016/S1553–7250(08)34058–6.
14.
Stewart M. Towards a global definition of patient centred care. BMJ. 2001;322(7284):444–445. doi:10.1136/bmj.322.7284.444.
15.
Arnold P. Gold foundation. What is humanism in healthcare? http://www.gold-foundation.org... (dostęp: 2023.01.08).
16.
Calle GHL, Martin MC, Nin N. Seeking to humanize intensive care. RBTI. 2017;29(1). doi:10.5935/0103–507X.20170003.
17.
Cohen JJ. Viewpoint: Linking Professionalism to Humanism: What It Means, Why It Matters: Acad Med. 2007;82(11):1029–1032. doi:10.1097/01.ACM.0000285307.17430.74.
18.
Halpern N, Bentov-Gofrit D, Matot I, et al. The effect of integration of non-cognitive parameters on medical students’ characteristics and their intended career choices. Isr Med Assoc J. 2011;13(8):488–493.
19.
Montemayor C, Halpern J, Fairweather A. In principle obstacles for empathic AI: why we can’t replace human empathy in healthcare. AI Soc. 2022;37(4):1353–1359. doi:10.1007/s00146–021–01230-z.
20.
Steinhausen S, Ommen O, Thüm S, et al. Physician empathy and subjective evaluation of medical treatment outcome in trauma surgery patients. Patient Educ Couns. 2014;95(1):53–60. doi:10.1016/j.pec.2013.12.007.
21.
Kerasidou A, Bærøe K, Berger Z, et al. The need for empathetic healthcare systems. J Med Ethics. 2021;47(12):e27-e27. doi:10.1136/medethics-2019–105921.
22.
Moudatsou M, Stavropoulou A, Philalithis A, et al. The Role of Empathy in Health and Social Care Professionals. Healthcare. 2020;8(1):26. doi:10.3390/healthcare8010026.
23.
Leal C, Tirado S, Rodríguez-Marín J, et al. Creation of the communication skills scale in health professionals, CSS-HP. An Psicol. 2015;32(49).
24.
Leal-Costa C, Tirado-González S, Rodríguez-Marín J, et al. Psychometric properties of the Health Professionals Communication Skills Scale (HP-CSS). Int J Clin Health Psychol. 2016;16(1):76–86. doi:10.1016/j.ijchp.2015.04.001.
25.
Cain MK, Zhang Z, Yuan KH. Univariate and multivariate skewness and kurtosis for measuring nonnormality: Prevalence, influence and estimation. Behav Res Methods. 2017;49(5):1716–1735. doi:10.3758/s13428–016–0814–1.
26.
Deng J, Lei L, Zhang HL, et al. The current status and the influencing factors of humanistic care ability among a group of medical professionals in Western China. THC. 2019;27(2):195–208. doi:10.3233/THC-181389.
27.
OECD; European Observatory on Health Systems and Policies. Poland: Country Health Profile 2019; OECD: Brussels, Belgium, 2019.
28.
Beaudoin PL, Labbé M, Fanous A, et al. Teaching communication skills to OTL-HNS residents: multisource feedback and simulated scenarios. Am J Otolaryngol Head Neck Surg. 2019;48(1):8. doi:10.1186/s40463–019–0329–8.
29.
Itri JN, Yacob S, Mithqal A. Teaching Communication Skills to Radiology Residents Curr Probl Diagn Radiol. 2017;46(5):377–381. doi:10.1067/j.cpradiol.2017.01.005.
30.
Ramaswamy R, Williams A, Clark EM, et al. Communication Skills Curriculum for Foreign Medical Graduates in an Internal Medicine Residency Program. J Am Geriatr Soc. 2014;62(11):2153–2158. doi:10.1111/jgs.13094.
31.
Roter DL, Hall JA. Physician Gender and Patient-Centered Communication: A Critical Review of Empirical Research. Ann Rev Public Health. 2004;25(1):497–519. doi:10.1146/annurev.publhealth.25.101802.123134.
32.
Jeffrey D. Clarifying empathy: the first step to more humane clinical care. Br J Gen Pract. 2016;66(643):e143-e145. doi:10.3399/bjgp16X683761.
33.
Butt NS, Rai SI, Liaqat N. et al. Communication Skills of Postgraduate Residents Using Health Professionals Communication Skills Scale. RJRMC. 2022; 2.
34.
Sánchez Expósito J, Leal Costa C, Díaz Agea JL, et al. Socio-emotional competencies as predictors of performance of nursing students in simulated clinical practice. Nurse Educ Pract. 2018;32:122–128. doi:10.1016/j.nepr.2018.07.009.
35.
Llor Lozano J, Seva Llor AM, Díaz Agea JL, et al. Burnout, habilidades de comunicación y autoeficacia en los profesionales de urgencias y cuidados críticos. Enf Global. 2020;19(3):68–92. doi:10.6018/eglobal.381641.
36.
Hossny E, Gabra S, Hussien R. Assessment of Professional Communication Skills of Healthcare Professionals toward the Patients. ASNJ. 2022;10(30):242–253. doi:10.21608/asnj.2022.132940.1359.
37.
Flin R, Winter J, Sarac, C, et al. Human factors in patient safety: Review of topics and tools. Geneva, Switzerland, 2019: World Health Organisation, http://www.who.int/patientsafe... (dostęp: 2023.01.08).
38.
World Health Organization. WHO Patient safety curric‐ ulum guide: Multi‐professional edition. Geneva, Switzerland: 2011, WHO Press. http://apps.who.int/iris/bitst... eam/10665/44641/1/9789241501958_eng.pdf. (dostęp: 2023.01.08).
39.
Patel R, Bachu R, Adikey A, et al. Factors Related to Physician Burnout and Its Consequences: A Review Behav Sci. 2018;8(11):98. doi:10.3390/bs8110098.
40.
Lee SM, Ryu YH, Kim JH. The Impacts of Assertiveness on Attitudes toward Nurse-Physician Collaboration in Nursing Students. J Korean Acad Soc Nurs Educ. 2018;24(4):326–336. doi:10.5977/jkasne.2018.24.4.326.
41.
Dec-Pietrowska J, Szczepek AJ. A Study of Differences in Compulsory Courses Offering Medicine Humanization and Medical Communication in Polish Medical Schools: Content Analysis of Secondary Data. Int J Environ Res Public Health. 2021;18(24):13326. 2021. doi:10.3390/ijerph182413326.
42.
Kiedik D, Grzebieluch J, Chomątowska B, et al. Representatives of generation ‘Z’ as future doctors – results of research among final year students at medical universities in Poland. Ann Agric Environ Med. Published online January 3, 2023. doi:10.26444/aaem/156575.
43.
Epstein RM. Defining and Assessing Professional Competence. JAMA. 2002;287(2):226. doi:10.1001/jama.287.2.226.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.