RESEARCH PAPER
Frequency of sharp injuries among nurses, underreporting and availability of safety devices – importance of training
1
Department of Nutrition and Epidemiology, Medical University, Łódż, Poland
2
Department of Conservative Nursing, Medical University, Łódż, Poland
Corresponding author
Anna Garus-Pakowska
Department of Nutrition and Epidemiology, Medical University of Łódź, Żeligowskiego 7/9, Łódź, Poland
Department of Nutrition and Epidemiology, Medical University of Łódź, Żeligowskiego 7/9, Łódź, Poland
Med Og Nauk Zdr. 2024;30(4):316-322
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Needlesticks and injuries caused by sharp instruments constitute a significant occupational risk problem in the work of nurses; their number, however, is underestimated worldwide. The aim of the study is to assess the frequency and structure of needlestick and sharps injuries (NSIs) analyse their reporting, assess availability of safety devices, and check whetherf training affects NSIs reporting and use of safety devices.
Material and methods:
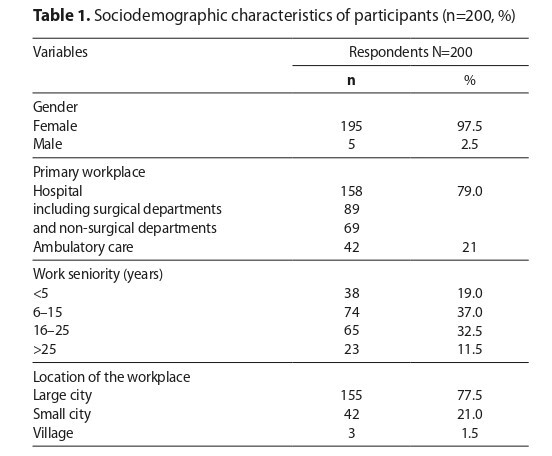
In 2021, a cross-sectional study was conducted with an online questionnaire among 200 nurses from the Łódź Province in Poland. The data were statistically analysed using descriptive methods. Pearson’s chi-squared test and Fisher›s exact probability test to compare the distribution of qualitative variables. The workplace, type of department, seniority and workplace location were related to the frequency of contact with potentially infectious material (PIM).
Results:
The study shows that unpredictable behaviour of a patient was the most common cause of injury, about 40% of nurses did not report NSIs, and 20.5% of nurses had never experienced NSIs. Nurses who had received infection prevention training and those who had undergone postexposure training in the past year were more likely to report NSIs. Most of the participants confirmed availability of safety devices, but the problem was that one in four nurses stated that they did not willingly use safety devices. The nurses who confirmed that training in the use of safety devices took place at work were more likely to use them. Most of the nurses had no influence on the type and quality of purchased safety devices.
Conclusions:
Emphasis should be placed on increasing NSIs reporting and the hospital management taking into account nurses' views of safety devices, which can be assisted by systematic training.
Needlesticks and injuries caused by sharp instruments constitute a significant occupational risk problem in the work of nurses; their number, however, is underestimated worldwide. The aim of the study is to assess the frequency and structure of needlestick and sharps injuries (NSIs) analyse their reporting, assess availability of safety devices, and check whetherf training affects NSIs reporting and use of safety devices.
Material and methods:
In 2021, a cross-sectional study was conducted with an online questionnaire among 200 nurses from the Łódź Province in Poland. The data were statistically analysed using descriptive methods. Pearson’s chi-squared test and Fisher›s exact probability test to compare the distribution of qualitative variables. The workplace, type of department, seniority and workplace location were related to the frequency of contact with potentially infectious material (PIM).
Results:
The study shows that unpredictable behaviour of a patient was the most common cause of injury, about 40% of nurses did not report NSIs, and 20.5% of nurses had never experienced NSIs. Nurses who had received infection prevention training and those who had undergone postexposure training in the past year were more likely to report NSIs. Most of the participants confirmed availability of safety devices, but the problem was that one in four nurses stated that they did not willingly use safety devices. The nurses who confirmed that training in the use of safety devices took place at work were more likely to use them. Most of the nurses had no influence on the type and quality of purchased safety devices.
Conclusions:
Emphasis should be placed on increasing NSIs reporting and the hospital management taking into account nurses' views of safety devices, which can be assisted by systematic training.
REFERENCES (25)
1.
Trzcińska A. Occupational exposure – the problem still valid. Forum Nefrologiczne. 2016;9(1):66–71.
2.
World Health Organization. Reducing Risks, Promoting Healthy Life. World Health Report; 2002.
3.
World Health Organization. WHO guideline on the use of safety-engineered syringes for intramuscular, intradermal and subcutaneous injections in health-care settings. 2015.
4.
Ji Y, Huang J, Jiang G, et al. Investigation of the occupational exposure to blood-borne pathogens of staff at a third-class specialist hospital in 2015–2018: a retrospective study. Sci Rep. 2022;12(1):1498. https://doi.org/10.1038/s41598....
5.
Matsubara C, Sakisaka K, Sychareun V, et al. Prevalence and risk factors of needle stick and sharps injury among tertiary hospital workers, Vientiane, Lao PDR. J Occup Health. 2017;59(6):581–585. https://doi.org/10.1539/joh.17....
6.
Świątkowska B, Hanke W. Occupational diseases in Poland in 2021. Institute of Occupational Medicine. Central Register of Occupational Diseases: Lodz; 2022. https://www.imp.lodz.pl/pliki/....
7.
Rubbi I, Cremonini V, Butuc A, et al. Incidence and type of health care associated injuries among nursing students: an experience in northern Italy. Acta Biomed. 2018;89(7–S):41–49. doi:10.23750/abm.v89i7-S.7812.
8.
Aziz S, Akhter A, Akhter K, et al. Prevalence of needle stick injury and its associated factors among nursing staff working at a tertiary care hospital of North India. Int J Res Med Sci. 2023;11:3755–62. https://dx.doi.org/10.18203/23....
9.
Ngatu NR, Phillips EK, Wembonyama OS, et al. Practice of universal precautions and risk of occupational blood-borne viral infection among Congolese health care workers. Am J Infect Control. 2012;40(1):68–70. https://doi.org/10.1016/j.ajic....
10.
Himmelreich H, Rabenau HF, Rindermann M, et al. The Management of Needlestick Injuries. Deutsches Arzteblatt. 2013;110(5):61–67. https://doi.org/10.3238/arzteb....
11.
Schuurmans J, Lutgens SP, Groen L, et al. Do safety engineered devices reduce needlestick injuries. J Hosp Infect. 2018;100:99–104. https://doi.org/10.23937/2474-....
12.
Marjadi B, Nguyen JD, Hoppett McLaws ML. Needlestick Injury among Medical Students in an Australian University. J Infect Dis and Epidemiol. 2017;3(034):1–4. https://doi.org/10.23937/2474-....
13.
Council Directive 2010/32/EU of 10 May 2010 implementing the Framework Agreement on prevention from sharp injuries in the hospital and healthcare sector concluded by HOSPEEM and EPSU. https://eur-lex.europa.eu/eli/... (access: 2023.11.10).
14.
Garus-Pakowska A, Górajski M. Epidemiology of needlestick and sharp injuries among health care workers based on records from 252 hospitals for the period 2010–2014, Poland. BMC Public Health. 2019;19(1):634. https://doi.org/10.1186/s12889....
15.
Jahic R, Piljic D, Porobic-Jahic H, et al. Epidemiological characteristics of the accidental exposures to blood-borne pathogens among workers in the hospital. Med Arch. 2018;72(3):187–191. https://doi.org/10.5455/medarh....
16.
Garus-Pakowska A, Górajski M, Szatko F. Did legal regulations change the reporting frequency of sharp injuries of medical personnel? Study from 36 hospitals in Łódź province, Poland. Int J Occup Med Environ Health. 2018;31(1):37–46. https://doi.org/10.13075/ijome....
17.
Aydin NN, Aksoy F, Yilmaz G, et al. An Assessment of Sharps Injuries in Healthcare Workers. Viral Hepatitis Journal. 2018;24(3):75–78. https://doi.org/10.4274/vhd.20....
18.
Cooke CE, Stephens M. Clinical, economic, and humanistic burden of needlestick injuries in healthcare workers. Med Devices: Evidence and Research. 2017;10:225–235. https://doi.org/10.2147/MDER.S....
19.
Wada K, Yoshikawa T, Lee JJ, et al. Sharp injuries in Japanese operating theaters of HIV/AIDS referral hospitals 2009–2011. Ind Health. 2016;54(4):224–229. https://doi.org/10.2486/indhea....
20.
Yifang Y, Yuan S, Li Y, et al. Assessment of adherence behaviors for the self-reporting of occupational exposure to blood and body fluids among registered nurses A cross-sectional study. PLoS ONE 2018;13(9):1–13. https://doi.org/10.1371/journa....
21.
Jończyk A, Szczypta A, Talaga-Ćwiertnia K. Injures as exposure events in providing medical services by nursing Staff. Przegl epidemiol. 2018;72(3):371–381. https://doi.org/10.32394/pe.72....
22.
Cheetham S, Ngo HTT, Liira J, et al. Education and training for preventing sharps injuries and splash exposures in healthcare workers. Cochrane Database of Systematic Reviews. 2021;4:CD012060. https://doi.org/10.1002/146518....
23.
Ding E, Tian S, Cheng M, et al. Investigation and analysis of the status of blood-borne occupational exposure of medical staff in a top three hospital and intervention measures. Chinese Journal of Industrial Hygiene and Occupational Diseases. 2019;37(8):593–596. https://doi.org/10.3760/cma.j.....
24.
Ballout R, Diab B, Harb A, et al. Use of safety-engineered devices by healthcare setting: a systematic reviev and meta-analisis. BMC Health Serv Res. 2016;16:458. https://doi.org/10.1186/s12913....
25.
Mannocci A, De Carli G, Di Bari V, et al. How Much do Needlestick Injuries Cost? A Systematic Reviev of the Economic Evaluations of Needlestick and Sharps Injuries Among Healtcare Personnel. Infect. Control Hosp. Epidemiol. 2016;37(6):635–646. https://doi.org/10.1017/ice.20....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.