RESEARCH PAPER
Factors influencing the perception of pain after surgery
1
Faculty of Health Sciences, Vincent Pol University, Lublin, Poland
These authors had equal contribution to this work
Corresponding author
Med Og Nauk Zdr. 2024;30(3):218-222
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Pain is the natural response of the body to surgical intervention. However, its intensity and duration can depend on the type of surgery, location of the procedure, and the individual characteristics of the patient. shortening the recovery period and improving the overall well-being of the patient. The aim of this study was to identify factors that exacerbate pain in adult patients following surgical treatment
Material and methods:
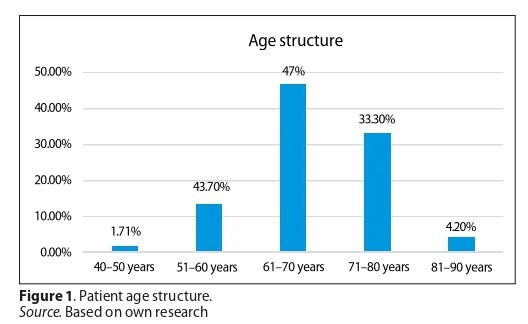
A retrospective analysis of medical records was conducted for patients who underwent surgery for colorectal cancer over a period of 6 months. The study included 117 patients. Statistical analysis of the study results was performed using IBM SPSS Statistics
Results:
Nearly 95% of patients experienced pain after surgery. It was identified that the following factors contributed to increased pain perception: pre-operative systemic treatment (p = 0.017), high risk of post-operative wound infection (p = 0.022), surgical method – laparotomy (p = 0.018), and body mass index (BMI) value (p = 0.012).
Conclusions:
Post-operative pain is one of the most significant problems after surgery. Factors influencing increased pain sensations have been identified, such as: BMI value, surgical method, risk assessment of infection, and systemic treatment used before surgery. The primary aim of post-operative management is to eliminate unnecessary suffering, provide comfort, and facilitate recovery
Pain is the natural response of the body to surgical intervention. However, its intensity and duration can depend on the type of surgery, location of the procedure, and the individual characteristics of the patient. shortening the recovery period and improving the overall well-being of the patient. The aim of this study was to identify factors that exacerbate pain in adult patients following surgical treatment
Material and methods:
A retrospective analysis of medical records was conducted for patients who underwent surgery for colorectal cancer over a period of 6 months. The study included 117 patients. Statistical analysis of the study results was performed using IBM SPSS Statistics
Results:
Nearly 95% of patients experienced pain after surgery. It was identified that the following factors contributed to increased pain perception: pre-operative systemic treatment (p = 0.017), high risk of post-operative wound infection (p = 0.022), surgical method – laparotomy (p = 0.018), and body mass index (BMI) value (p = 0.012).
Conclusions:
Post-operative pain is one of the most significant problems after surgery. Factors influencing increased pain sensations have been identified, such as: BMI value, surgical method, risk assessment of infection, and systemic treatment used before surgery. The primary aim of post-operative management is to eliminate unnecessary suffering, provide comfort, and facilitate recovery
REFERENCES (25)
1.
Chojnacka-Kowalewska G, Sopolińska M, Chojnacka B. Ocena skuteczności leczenia dolegliwości bólowych u pacjentów w pierwszej dobie po przednich resekcjach odbytnicy z powodu nowotworu złośliwego. Innowacje w Pielęgniarstwie i Naukach o Zdrowiu. 2022;7(3):7–28. https://doi.org/10.21784/IwP.2....
2.
Pysz-Waberski D, Bulska-Będkowska W, Wachuła E. Leczenie bólu przewlekłego w onkologii – współpraca onkologa z psychoonkologiem. Onkologia w Praktyce Klinicznej – Edukacja. 2019;5(4):257–265.
3.
Cata JP, Corrales G, Speer B, Owusu-Agyemang P. Postoperative acute pain challenges in patients with cancer. Best Pract Res Clin Anaesthesiol. 2019;33(3):361–371. https://doi.org/10.1016/j.bpa.....
4.
Amaechi O, McCann Huffman M, Featherstone K, et al. Pharmacologic therapy for acute pain. Am Fam Physician. 2021:104(1):63–72.
5.
Krawczyk M, Wrdliczek J, Czupryna A, et al. Rekomendacje w uśmierzaniu bólu okołooperacyjnego w chirurgii ogólnej. Chirurgia po Dyplomie. 2013;8(1):47–56.
6.
Mears L, Mears J. The pathophysiology, assessment, and management of acute pain. Br J Nurs. 2023;32(2):58–65. https://doi.org/10.12968/bjon.....
7.
Lopes A, Seligman Menezes M, Antonio Moreira de Barros G. Chronic postoperative pain: ubiquitous and scarcely appraised: narrative review. Braz J Anesthesiol. 2021;71(6):649–655. https://doi.org/10.1016/j.bjan....
8.
Gawęda A, Kamińska J, Wawoczna G, et al. Ból pooperacyjny w opinii pacjenta. Pielęgniarstwo Pol. 2020;4(78):209–216. https://doi.org/10.20883/pielp....
9.
Small C, Laycock H. Acute postoperative pain management. Br J Surg. 2020;107(2):e70-e80. https://doi.org/10.1002/bjs.11....
10.
Budzyńska K. Ból jako jeden z głównych problemów osób leczonych operacyjnie. Innowacje w Pielęgniarstwie i Naukach o Zdrowiu. 2021;6(2):33–45. https://doi.org/10.21784/IwP.2....
11.
Wojciechowska U, Barańska K, Michałek I, et al. Nowotwory złośliwe w Polsce w 2020 roku. Zwrotnik raka. https://www.zwrotnikraka.pl/no... (access: 2024.06.13).
12.
Grochans E, Hyrcza V, Kuczyńska M, et al. Subjctive, postoperative judgment of patients pain after certain surgery. Surg Vascular Nurs. 2011;5(2):82–87.
13.
Golden A. Obesity›s Impact. Nurs Clin North Am. 2021;56(4):xiii-xiv. https://doi.org/10.1016/j.cnur....
14.
Sun X, Yan AF, Shi Z, et al. Health consequences of obesity and projected future obesity health burden in China. Obesity (Silver Spring). 2022;30(9):1724–1751. https://doi.org/10.1002/oby.23....
15.
González-Callejas C, Aparicio VA, De Teresa C, Nestares T. Association of Body Mass Index and Serum Markers of Tissue Damage with Postoperative Pain. The Role of Lactate Dehydrogenase for Postoperative Pain Prediction. Pain Med. 2020;21(8):1636–1643. https://doi.org/10.1093/pm/pnz....
16.
Giesinger K, Giesinger JM, Hamilton DF, Rechsteiner J, Ladurner A. Higher body mass index is associated with larger postoperative improvement in patient-reported outcomes following total knee arthroplasty. BMC Musculoskelet Disord. 2021;22(1):635.
17.
Safaei M, Sundararajan EA, Driss M, Boulila W, Shapi›i A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput Biol Med. 2021;136:104754.
18.
Iqbal U, Green JB, Patel S, et al. Preoperative patient preparation in enhanced recovery pathways. J Anaesthesiol Clin Pharmacol. 2019;35(Suppl1):S14-S23. https://doi.org/10.4103/joacp.....
19.
Naranjo C, Ortega-Jiménez P, Del Reguero L, et al. Relationship between diabetic neuropathic pain and comorbidity. Their impact on pain intensity, diabetes complications and quality of life in patients with type-2 diabetes mellitus. Diabetes Res Clin Pract. 2020;165:108236. https://doi.org/10.1016/j.diab....
20.
Chiang HL, Huang YC, Lin HS, et al. Hypertension and Postoperative Pain: A Prospective Observational Study. Pain Res Manag. 2019; 2019:8946195. https://doi.org/10.1155/2019/8....
21.
Sevick MA, Trauth JM, Ling BS, et al. Patients with Complex Chronic Diseases: perspectives on supporting self-management. J Gen Intern Med. 2007;22 Suppl 3(Suppl 3):438–444. https://doi.org/10.1007/s11606....
22.
Marmiroli P, Scuteri A, Cornblath DR,et al.Pain in chemotherapy-induced peripheral neurotoxicity. J Peripher Nerv Syst. 2017;22(3):156–161. https://doi.org/10.1111/jns.12....
23.
Wang J, Cheng L, Liu J, et al. Laparoscopy vs. Laparotomy for the Management of Abdominal Trauma: A Systematic Review and Meta-Analysis. Front Surg. 2022;9:817134. https://doi.org/10.3389/fsurg.....
24.
Gao Y, Li S, Xi H, et al. Laparoscopy versus conventional laparotomy in the management of abdominal trauma: a multi-institutional matched-pair study. Surg Endosc. 2020;34(5):2237–2242. https://doi.org/10.1007/s00464....
25.
Buia A, Stockhausen F, Hanisch E. Laparoscopic surgery: A qualified systematic review. World J Methodol. 2015;5(4):238–254. https://doi.org 10.5662/wjm.v5.i4.238.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.