REVIEW PAPER
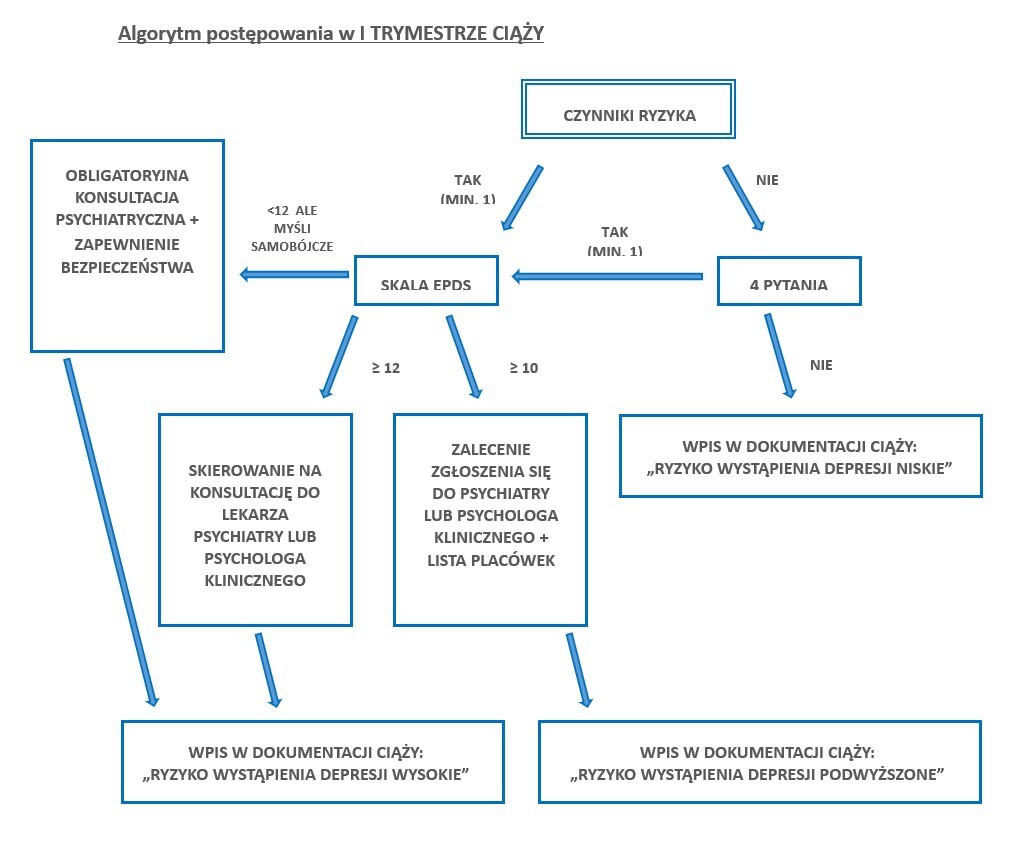
Why and how to monitor the risk of perinatal depression - management algorithms.
1
Uniwersytecki Szpital Kliniczny w Poznaniu, Polska
2
Katedra Zdrowia Matki i Dziecka, Uniwersytet Medyczny im. Karola Marcinkowskiego w Poznaniu, Polska
3
Zakład Zdrowia Kobiet, Instytut Medycyny Wsi w Lublinie, Polska
Med Og Nauk Zdr. 2024;30(3):208-212
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Postpartum depression is a medical condition which affects approximately 7–19% of pregnant women. The occurrence of postpartum depression has negative consequences for both the mother and the child, and negatively affects the functioning of the family. Each assessment of the patient’s condition should consist of an interview focused on psychological and social aspects and the use of appropriate screening tools. The article aims to spread general awareness about postpartum depression, its consequences, and ways to support women. The practical aspect of the publication provides precise guidance for healthcare professionals which allows early diagnosis and monitoring of depression risk factors
Review methods:
The article was prepared based on materials obtained from the PubMed electronic database, a review of recommendations and current standards of practice. The materials were selected using the key words: ‘postpartum’, ‘depression’, ‘mood’, ‘disorders’, ‘pregnancy’, ‘postnatal’, ‘algorithm’, and taking into account the assessment of the usefulness of research results/conclusions for practitioners. The article was based mainly on current literature.
Brief description of the state of knowledge:
Brief description of the state of knowledge. According to the current state of knowledge, postpartum depression is a common condition; however, it often remains underdiagnosed. The role of health care professionals, gynaecologists-obstetricians and midwives, is crucial in diagnosing and caring for patients, as well as the impact of social support on the course of depression and the process of recovery. Early intervention for the mother reduces the consequences for her child.
Summary:
Summing up, it is very important to monitor risk factors and act appropriately in the event of an increased risk of depression
Postpartum depression is a medical condition which affects approximately 7–19% of pregnant women. The occurrence of postpartum depression has negative consequences for both the mother and the child, and negatively affects the functioning of the family. Each assessment of the patient’s condition should consist of an interview focused on psychological and social aspects and the use of appropriate screening tools. The article aims to spread general awareness about postpartum depression, its consequences, and ways to support women. The practical aspect of the publication provides precise guidance for healthcare professionals which allows early diagnosis and monitoring of depression risk factors
Review methods:
The article was prepared based on materials obtained from the PubMed electronic database, a review of recommendations and current standards of practice. The materials were selected using the key words: ‘postpartum’, ‘depression’, ‘mood’, ‘disorders’, ‘pregnancy’, ‘postnatal’, ‘algorithm’, and taking into account the assessment of the usefulness of research results/conclusions for practitioners. The article was based mainly on current literature.
Brief description of the state of knowledge:
Brief description of the state of knowledge. According to the current state of knowledge, postpartum depression is a common condition; however, it often remains underdiagnosed. The role of health care professionals, gynaecologists-obstetricians and midwives, is crucial in diagnosing and caring for patients, as well as the impact of social support on the course of depression and the process of recovery. Early intervention for the mother reduces the consequences for her child.
Summary:
Summing up, it is very important to monitor risk factors and act appropriately in the event of an increased risk of depression
REFERENCES (16)
1.
Brudkiewicz P. Depresja i psychoza poporodowa. Medycyna Praktyczna. https://www.mp.pl/pacjent/psyc... (access: 24.06.2024).
2.
Maliszewska K, Preis K. Terapia depresji poporodowej – aktualny stan wiedzy. Ann Acad Med Gedan. 2014;44:105–111.
3.
Dominiak M, Antosik-Wojcinska AZ, Baron M, et al. Recommendations for the prevention and treatment of postpartum depression. Ginekol Pol. 2021;92(2):153–164. https://doi:10.5603/GP.a2020.0....
4.
Amani B, Krzeczkowski JE, Schmidt LA, et al. Public health nurse-delivered cognitive behavioral therapy for postpartum depression: Assessing the effects of maternal treatment on infant emotion regulation. Dev Psychopathol. 2024:1–9. https://doi.org/10.1017/S09545....
5.
Dagher RK, Bruckheim HE, Colpe LJ. Perinatal Depression: Challenges and Opportunities. J Womens Health (Larchmt). 2021;30(2):154–159. https://doi.org/10.1089/jwh.20....
6.
Jośko-Ochojska J. Traumatyczne przeżycia matki ciężężarnej a zdrowie jej dziecka. Dziecko Krzywdzone. Teoria, badania, praktyka. 2016;15(3).
7.
Van Niel MS, Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020;87(5):273–277. https://doi.org/10.3949/ccjm.8....
8.
Oliveira TA, Luzetti GGCM, Rosalém MMA, el al. Screening of Perinatal Depression Using the Edinburgh Postpartum Depression Scale. Rev Bras Ginecol Obstet. 2022;44(5):452–457. https://doi.org/10.1055/s-0042....
9.
Rekomendacje do standardów organizacyjnych opieki okołoporodowej. Polskie Towarzystwo Położnych. http://www.ptpol.pl/o-nas/reko... (access: 24.06.2024).
10.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–78.
11.
Rekomendacja nr 13/2020 z dnia 30 listopada 2020 r. Prezesa Agencji Oceny Technologii Medycznych i Taryfikacji w sprawie zalecanych technologii medycznych, działań przeprowadzanych w ramach programów polityki zdrowotnej oraz warunków realizacji tych programów, dotyczących problemu zdrowotnego depresji poporodowej. Agencja Oceny Technologii Medycznych i Taryfikacji. https://bipold.aotm.gov.pl/ass... (access: 24.06.2024).
12.
Rozporządzenie Ministra Zdrowia z dnia 16 sierpnia 2018 roku w sprawie standardu organizacyjnego opieki okołoporodowej. Dziennik Ustaw. 2018 poz. 1756. https://isap.sejm.gov.pl/isap.... (access: 24.06.2024).
13.
Kułak-Bejda A, Bejda G, Waszkiewicz N. Zasady komunikacji z pacjentem doświadczającym zaburzeń psychicznych i jego rodziną. In: Krajewska-Kułak E, Guzowski AN, Bejda G, Lankau A, editor. Kontekst „Inności” w komunikacji interpersonalnej: praca zbiorowa; 2019. p. 338–354.
14.
Goodman JH. Women’s attitudes, preferences, and perceived barriers to treatment for perinatal depression. Birth. 2009;36(1):60–69. https://doi.org/10.1111/j.1523....
15.
Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013(2):CD001134. https://doi.org/10.1002/146518....
16.
Mental Health During Childbirth And Across The Lifespan. Perinatal Mental Health Task Force, Clinical Standards, Documents Committee Approved by the Board of Directors. 2020. https://www.mid wife.org/acnm/files/acnmlibrarydata/uploadfilename/000000000324/PS- Mental%20Health%20During%20Childbirth%20and%20Across%20Lifespan.pdf.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.