REVIEW PAPER
Diet therapy and pharmacotherapy in the prevention and prophylaxis of food allergies and intolerance
1
Department of Environmental Biology, Jan Kochanowski University, Kielce, Poland
2
Department of Medical Biology, Jan Kochanowski University, Kielce, Poland
3
No. 5 Educatory Facilities, Education and Upbringing Facilities, Skarżysko-Kamienna, Poland
These authors had equal contribution to this work
Corresponding author
Joanna Ślusarczyk
Zakład Biologii Środowiska, Uniwersytet Jana Kochanowskiego, Uniwersytecka 7, 25-406, Kielce, Polska
Zakład Biologii Środowiska, Uniwersytet Jana Kochanowskiego, Uniwersytecka 7, 25-406, Kielce, Polska
Med Og Nauk Zdr. 2025;31(1):13-19
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The global problem of allergies, including food allergies, affects every age group. For many years, the treatment of allergies has been limited to therapy consisting in administration of drugs suppressing the activity of the immune system. The aim of this review is to compile information about food allergies and food intolerance, assess the importance of diet therapy and pharmacotherapy in the treatment of these conditions, and discuss the role of the intestinal microbiome in the prevention of food allergies.
Review methods:
A review of available literature was conducted using electronic databases (PubMed and Google Scholar) and appropriate key words. Publications from the last eight years constituted 80%
Brief description of the state of knowledge:
Observations carried out in recent years indicate a constantly increasing problem of food allergy in both children and adults. Some of the most common food disorders are gluten, lactose, and histamine intolerance. The development of food allergies is complex and multifaceted. A key role in their development is played by genetic and environmental factors. Allergens of plant and animal origin can trigger food allergies. The role of the bacterial intestinal microbiome and proper nutrition in organism response to contact with a potential allergen is increasingly being highlighted.
Summary:
The current medical knowledge does not provide quick therapies for food allergies. Improvement of the quality of life of patients with food allergy or intolerance is primarily achieved by introduction of an elimination diet,and pharmacological treatment aimed at enhancement of the efficacy of therapies.
The global problem of allergies, including food allergies, affects every age group. For many years, the treatment of allergies has been limited to therapy consisting in administration of drugs suppressing the activity of the immune system. The aim of this review is to compile information about food allergies and food intolerance, assess the importance of diet therapy and pharmacotherapy in the treatment of these conditions, and discuss the role of the intestinal microbiome in the prevention of food allergies.
Review methods:
A review of available literature was conducted using electronic databases (PubMed and Google Scholar) and appropriate key words. Publications from the last eight years constituted 80%
Brief description of the state of knowledge:
Observations carried out in recent years indicate a constantly increasing problem of food allergy in both children and adults. Some of the most common food disorders are gluten, lactose, and histamine intolerance. The development of food allergies is complex and multifaceted. A key role in their development is played by genetic and environmental factors. Allergens of plant and animal origin can trigger food allergies. The role of the bacterial intestinal microbiome and proper nutrition in organism response to contact with a potential allergen is increasingly being highlighted.
Summary:
The current medical knowledge does not provide quick therapies for food allergies. Improvement of the quality of life of patients with food allergy or intolerance is primarily achieved by introduction of an elimination diet,and pharmacological treatment aimed at enhancement of the efficacy of therapies.
REFERENCES (50)
2.
Rey A, Chełmińska M. Ogólne zasady postępowania w chorobach alergicznych w praktyce lekarza rodzinnego. Forum Med Rodz. 2019;13(4):170–175.
3.
Cukrowska B. Probiotyki w profilaktyce i leczeniu chorób alergicznych – przegląd piśmiennictwa. Standardy medyczne/Pediatria. 2013;11:191–201.
4.
Gregorczyk-Maślanka K, Kurzawa R. Mikrobiota organizmu ludzkiego i jej wpływ na homeostazę immunologiczną – część I. Alerg Astma Immun. 2016;21(3):146–150.
5.
Libório SdO, Freire Alberca GG, Sato MN, et al. Allergy: Concepts and Treatments. Front. Young Minds. 2020;8:43. https://doi.org/10.3389/frym.2....
6.
Wasilewska E, Ziętarska M, Małgorzewicz S. Immunologiczna nadwrażliwość na pokarm. Forum Zab Metabol. 2016;7(4):152–161.
7.
Wierzchanowska WM, Iwanicki T. Rola mikrobiomu jelitowego w funkcjonowaniu układu nerwowego. Kosmos. 2020;69(2):301–311. https://doi.org/10.36921/kos.2....
8.
Chinthrajah RS, Hernandez JD, Boyd SD, et al. Molecular and cellular mechanisms of food allergy and food tolerance. J Allergy Clin Immunol. 2016;137(4):984–997. https://doi.org/10.1016/j.jaci....
9.
Foong RX, Santos AF. Biomarkers of diagnosis and resolution of food allergy. Pediatr Allergy Immunol. 2021;32(2):223–233. https://doi.org/10.1111/pai.13....
10.
Kalinowska A, Marciniak M, Grzymisławski M. Żywienie osób z nadwrażliwością pokarmową. In: Grzymisławski M, editors. Dietetyka kliniczna. Warszawa: PZWL; 2020. p. 509–543.
11.
Bos A, van Egmond M, Mebius R. The role of retinoic acid in the production of immunoglobulin A. Mucosal Immunol. 2022;15(4):562–572. https://doi.org/10.1038/s41385....
12.
Zhang P, Xu Q, Zhu R. Vitamin D and allergic diseases. Front. Immunol. 2024;15:1420883. https://doi.org/10.3389/fimmu.....
13.
Moro K, Yamada T, Tanabe M, et al. Innate production of T(H)2 cytokines by adipose tissue-associated c-Kit(+)Sca-1(+) lymphoid cells. Nature. 2010;463(7280):540–4. https://doi.org/10.1038/nature....
14.
Januszkiewicz E, Mierzejewski M, Biniszewska O, et al. The importance of the gut microbiome in the development of allergic diseases. Alergol Pol – Polish J Allergol. 2023;10(3):202–209. https://doi.org/10.5114/pja.20....
15.
Brończyk-Puzoń A, Bieniek J, Koszowska A, et al. Jakość życia osób z celiakią, alergią i nadwrażliwością na gluten stosujących dietę bezglutenową – ocena za pomocą kwestionariusza WHOQOL-BREF. Med Og Nauk Zdr. 2014;20(3):241–244. https://doi.org/10.5604/208345....
16.
Bartuzi Z, Ukleja-Sokołowska N. Alergia pokarmowa na mąkę i celiakia. Alergia. 2014;2:4–10.
17.
Dardzińska J, Banach D, Małgorzewicz S. Diety roślinne a ryzyko osteoporozy. Forum Zab Metabol. 2016;7(3):99–105.
18.
Gajewska D, Kibil I. Wege Dieta roślinna w praktyce. Warszawa: PZWL; 2019. p. 128–132.
19.
Fassio F, Facioni MS, Guagnini F. Lactose Maldigestion, Malabsorption, and Intolerance: A Comprehensive Review with a Focus on Current Management and Future Perspectives. Nutrients. 2018;10(11):1599. https://doi.org/10.3390/nu1011....
20.
Suchy FJ, Brannon PM, Carpenter TO, et al. National Institutes of Health Consensus Development Conference: Lactose Intolerance and Health. Ann Intern Med. 2010;152(12):792–796. https://doi.org/10.7326/0003-4....
21.
Nigra AD, Teodoro AJ, Gil GA. A Decade of Research on Coffee as an Anticarcinogenic Beverage. Oxid Med Cell Longev. 2021;2021:4420479. https://doi.org/10.1155/2021/4....
22.
Chieng D, Kistler PM. Coffee and tea on cardiovascular disease (CVD) prevention. Trends Cardiovasc Med. 2022;32(7):399–405. https://doi.org/10.1016/j.tcm.....
23.
Suphioglu C. Coffee Anyone? Are You at Risk of Allergy? Int Arch Allergy Immunol. 2012;159(3):213–215. https://doi.org/10.1159/000339....
24.
Tuck CJ, Biesiekierski JR, Schmid-Grendelmeier P, et al. Food Intolerances. Nutrients. 2019;11(7):1684. http://doi.org/10.3390/nu11071....
25.
Martin ISM, Brachero S, Vilar EG. Histamine intolerance and dietary management: A complete review. Allergol Immunopathol (Madr). 2016;44(5):475–483. https://doi.org/10.1016/j.alle....
27.
Bartuzi M, Ukleja-Sokołowska N. Nietolerancja histaminy a dieta współczesnego człowieka. Alergia Astma Immunol. 2021;26(4):82–88.
28.
Cudowska B, Kaczmarski M, Sawicka-Żukowska M. Objawy ze strony przewodu pokarmowego u dzieci z alergią wieloważną. Przegl Pediatryczny. 2010;40(1):16–20.
30.
Panaszek B, Szmagierewski W. Źródła alergenów reagujących krzyżowo i ich znaczenie kliniczne. Alergia. 2010;4:32–38.
31.
Pomés A, Davies JM, Gadermaier G. WHO/IUIS Allergen Nomenclature: Providing a common language. Mol Immunol. 2018;100:3–13. https://doi.org/10.1016/j.moli....
32.
Wawrzeńczyk A, Bartuzi Z. Zespoły kliniczne alergii krzyżowej. Alergia Astma Immunol. 2018;23(2):64–66.
33.
Błażowski Ł, Gregorczyk-Maślanka K, Kurzawa R. Zespół alergii jamy ustnej (zespół pyłkowo-pokarmowy), anafilaksja i alergologia molekularna. Nowe endotypy, nowe horyzonty. Pol J Allergol. 2016;3(4):137–143. https://doi.org/10.1016/j.aler....
34.
Kiguchi T, Yamamoto-Hanada K, Saito-Abe M, et al. Pollen-food allergy syndrome and component sensitization in adolescents: A Japanese population-based study. PLoS One. 2021;16(4):e0249649. https://doi.org/10.1371/journa....
35.
Kargano D, Appanna R, Santonicola A, et al. Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns. Nutrients. 2021;13(5):1638. https://doi.org/10.3390/nu1305....
36.
Krogulska A. Diagnostyka alergii pokarmowej w 2023 roku. Standardy Medyczne/Pediatria. 2023;20:302–311.
37.
Małgorzewicz S, Wasilewska E. Diagnostyka niepożądanych reakcji na pokarm. Forum Zab Metabol. 2016;7(2):62–68.
38.
Butrym I, Płaczkowska S, Pawlik-Sobecka L, et al. Podstawowe testy wykorzystywane w diagnostyce alergii IgE-zależnej i alergii kontaktowej. Diagn Lab. 2017;53(3):169–174. https://doi.org/10.5604/01.300....
39.
Krakowiak W, Lisowska H, Kaca W. Pathogenic Features of Porphyromonas Gingivalis Influence Progression of Rheumatoid Arthritis. Adv Microbiol. 2024;63(1):15–22. https://doi.org/10.2478/am-202....
40.
Ding RX, Goh WR, Wu RN, et al. Revisit gut microbiota and its impact on human health and disease. J Food Drug Anal. 2019;27(3):623–631. https://doi.org/10.1016/j.jfda....
41.
Milani C, Duranti S, Bottacini F, et al. The First Microbial Colonizers of the Human Gut: Composition, Activities, and Health Implications of the Infant Gut Microbiota. Microbiol Mol Biol Rev. 2017;81(4):e00036–17. https://doi.org/10.1128/MMBR.0....
42.
Wastyk HC, Fragiadakis GK, Perelman D, et al. Gut-microbiota-targeted diets modulate human immune status. Cell. 2021;184(16):4137–4153.e14. https://doi.org/10.1016/j.cell....
43.
Makki K, Deehan EC, Walter J, et al. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host Microbe. 2018;23(6):705–715. https://doi.org/10.1016/j.chom....
44.
Huang YJ, Marsland BJ, Bunyavanich S, et al. The microbiome in allergic disease: Current understanding and future opportunities-2017 PRACTALL document of the American Academy of Allergy, Asthma & Immunology and the European Academy of Allergy and Clinical Immunology. J Allergy Clin Immunol. 2017;139(4):1099–1110. https://doi.org/10.1016/j.jaci....
45.
Tang MLK, Ponsonby AL, Orsini F, et al. Administration of a probiotic with peanut oral immunotherapy: A randomized trial. J Allergy Clin Immunol. 2015;135(3):737–44.e8. https://doi.org/10.1016/j.jaci....
46.
Kalinowski P, Mirosław K. Wiedza rodziców na temat alergii pokarmowej występującej u ich dzieci. Med Og Nauk Zdr. 2014;20(1):88–91.
47.
Muraro A, Tropeano A, Giovannini M. Allergen immunotherapy for food allergy: Evidence and outlook. Allergol Select. 2022;6:285–292. https://doi.org/10.5414/ALX023....
48.
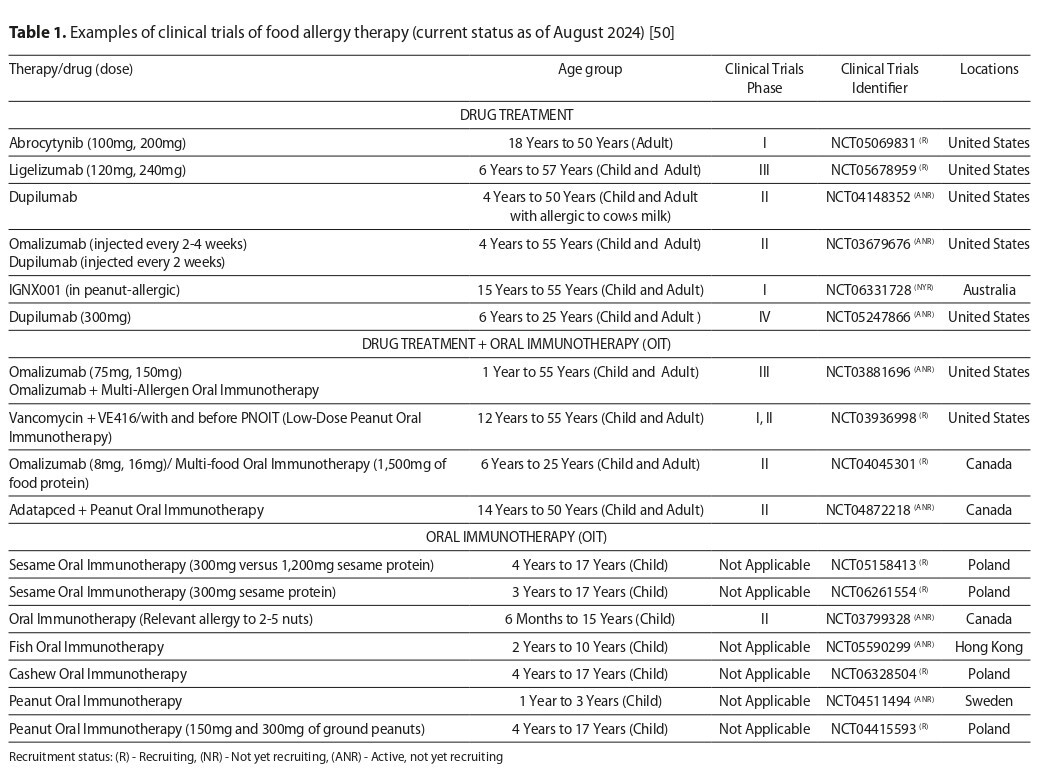
Stefanowicz A, Podsiedlik A, Poloczek A, et al. Food allergies, searching for rescue therapy: a literaturę review. Pol J Allergol. 2023;10(4):265–270. https://doi.org/10.5114/pja.20....
49.
Fowler J, Lieberman J. Update on clinical research for food allergy treatment. Front Allergy. 2023;4:1154541. https://doi.org/10.3389/falgy.....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.