CASE REPORT
Diagnosing ADHD using QEEG and planning EEG-biofeedback (Neurofeedback) therapy – pilot studies
1
Uniwersytet Rzeszowski, Polska
2
ADEA LTD, Bulgaria
Corresponding author
Med Og Nauk Zdr. 2021;27(2):205-212
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Among the causes of attention deficit hyperactivity disorder (ADHD) are mentioned mainly biological conditions (genetic, biochemical and anatomical). Environmental factors also significantly affect the functioning of the individual, but are largely a consequence of the determined biologically specific reactions of a child or an adult with ADHD. Thus, early diagnosis of dysfunctions is an important precondition for undertaking appropriate actions to mitigate specific symptoms and avoid various consequences related to attention deficit and hyperactivity. In diagnosing, it is necessary to take into account the objective and subjective symptoms of disorders. Here, an interview, observation, and psychological tests are also useful. Due to the difficulties in differential diagnosis related to various types of diseases, biological research is also important. Quantitative EEG (QEEG) is particularly helpful in making a diagnosis.
Objective:
The aim of the study was analysis of the usefulness of the QEEG method in diagnosing persons with ADHD, which is also the basis for planning supportive EEG biofeedback therapy.
Material and Methods:
The research presents a case study, which includes an in-depth analysis of the QEEG results concerning five randomly selected children with ADHD.
Results:
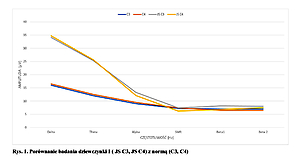
The QEEG assessment of children with ADHD shows repeated dependencies, the presence of high amplitudes of low-frequency waves – Delta, Theta, Alpha, and low amplitudes of high-frequency waves, compared to low-frequency waves. However, similar amplitudes of high-frequency waves were found – SMR, Beta1 and Beta2, and lower amplitudes of Beta2 waves, compared to Alpha and Theta.
Conclusions:
The QEEG test is very helpful in diagnosing ADHD. This method provides important information while planning EEG biofeedback therapy and checking its effectiveness.
Among the causes of attention deficit hyperactivity disorder (ADHD) are mentioned mainly biological conditions (genetic, biochemical and anatomical). Environmental factors also significantly affect the functioning of the individual, but are largely a consequence of the determined biologically specific reactions of a child or an adult with ADHD. Thus, early diagnosis of dysfunctions is an important precondition for undertaking appropriate actions to mitigate specific symptoms and avoid various consequences related to attention deficit and hyperactivity. In diagnosing, it is necessary to take into account the objective and subjective symptoms of disorders. Here, an interview, observation, and psychological tests are also useful. Due to the difficulties in differential diagnosis related to various types of diseases, biological research is also important. Quantitative EEG (QEEG) is particularly helpful in making a diagnosis.
Objective:
The aim of the study was analysis of the usefulness of the QEEG method in diagnosing persons with ADHD, which is also the basis for planning supportive EEG biofeedback therapy.
Material and Methods:
The research presents a case study, which includes an in-depth analysis of the QEEG results concerning five randomly selected children with ADHD.
Results:
The QEEG assessment of children with ADHD shows repeated dependencies, the presence of high amplitudes of low-frequency waves – Delta, Theta, Alpha, and low amplitudes of high-frequency waves, compared to low-frequency waves. However, similar amplitudes of high-frequency waves were found – SMR, Beta1 and Beta2, and lower amplitudes of Beta2 waves, compared to Alpha and Theta.
Conclusions:
The QEEG test is very helpful in diagnosing ADHD. This method provides important information while planning EEG biofeedback therapy and checking its effectiveness.
REFERENCES (39)
1.
Thapar A, Cooper M, Eyre O, et al. Practitioner review: What have we learnt about the causes of ADHD. J Child Psychol. Psychiatry. 2013; 5 4 (1): 3 –13.
2.
Gaidanowicz R, Deksnyte A, Palinauskaite K, et al. ADHD – plaga XXI wieku? Psychiatr Pol. 2018; 52(2): 287–387.
3.
De La Fuente A, Xia S, Branch C, Li X. A review of attention-deficit/hyperactivity disorder from the perspective of brain networks. Front Hum Neurosci. 2013; 7: 192.
4.
Rhodes SS. Parenting dependent young adults with ADHD. Pediatr Nurs. 2017; 43(5): 243.
5.
Philipp-Wiegman F, Retz-Junginger P, Retz W, Rosler M. The intrain-dividual impact of ADHD on the transition of adulthood to old age. Eur Arch Psychiatry Clin Neurosci. 2016; 266: 367–369.
6.
Wasserstein J. Diagnostic issues for adolescent and adults with ADHD. J Clin Psychol. 2005; 61: 535–547.
7.
Ochojska D, Pasternak J. Postawy rodzicielskie w percepcji studentów z ADHD. Wychowanie w Rodzinie. 2019: 20(1): 180–194.
8.
Munden A, Arcelus J. ADHD. Nadpobudliwość ruchowa. Kraków: Bellona; 2006: 130–133.
9.
Hetmańczyk H, Kawiak E. Diagnozowanie zespołu nadpobudliwości psychoruchowej z wykorzystaniem testu MOXO. Edukacja – Technika – Informatyka. 2018; 23(1): 237–241.
10.
Pisula A, Bryńska A, Kołakowski A, et al. ADHD – zespół nadpobud-liwości psychoruchowej. Przewodnik dla rodziców i wychowawców. Gdańsk: GWP; 2018.
11.
Orylska A, Jagielska G. Diagnoza zespołu nadpobudliwości psychoru-chowej z deficytem uwagi u dzieci w wieku przedszkolnym. Psychiatr Psychol K lin. 2011; 11(2): 115 –119.
12.
Conners CK, Sitarenios G, Parker JD, et al. The Revised Conners’ Pa-rent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abn Child Psychol. 1998; 26: 257–268.
13.
Conners CK. Conners Early Childhood Manual. Multi-Health Systems: New York; 2009.
14.
Bober-Płonka B, Kuleta-Krzyszkowiak M, Wasilewska M. Funkcjono-wanie studentów z ADHD – różnice między mężczyznami i kobietami. Edukacja – Technika – Informatyka. 2019; 1: 11–20.
15.
Kooij JJS, Francken MH. Diagnostic Interview for ADHD adults (Diva 2.0). In: Kooij JJS. Adult ADHD. Diagnostic Assessment and treatment. New York: Springer; 2013. p. 97–99.
16.
Levy E, Traicu A, Iyer S, et al. Psychotic disorders comorbid with attention-deficit hyperactivity disorder. An important knowledge gap. Can J Psychiatry. 2015; 60 (3 suppl. 2): 48–52.
17.
Blom JD, Niemantsverdriet M, Spuijbroek A, et al. Attention Deficit Disorder Psychosis. In: Sharpless BA, editor. Unusual and rare psy-chological disorders. A Handbook for clinical practice and research. Oxford: Oxford University Press; 2017: 78–81.
18.
Faraone CV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnosis valid? Am J Psychiatry. 2006; 163(10): 1720–1729.
19.
Lipowska M, Dykalska-Bieck D. Czy impulsywność w ADHD ma kom-ponenty temperamentalne? Psychiatr Psychol Klin. 2010; 10(3): 16–181.
20.
Fetz EE. Volitional control of neural activity: Implications for brain--computer interfaces. J Physiol. 2007; 15: 571–579.
21.
Walkowiak H. EEG biofeedback: charakterystyka, zastosowanie, opinie specjalistów. Studia Edukacyjne. 2015; 36: 307–325.
22.
Barry RJ, Clarke AR, Johnstone SJ, et al. EEG differences between eyes--closed and eyes-open resting conditions. Clin Neurophysiol. 2007; 118: 2765–73.
23.
Billeci L, Sicca F, Maharatna K, et al. On the application of quantitative EEG for characterizing autistic brain: a systematic review. Front Hum Neurosci. 2013; 7: 442.
24.
Chen C, Zhou C, Cavanaugh JM, et al. Quantitative electroencepha-lography in a swine model of blast-induced brain injury. Brain Inj. 2017; 31: 120–126.
25.
Wiśniewska M, Gmitrowicz A, Pawełczyk N. Zastosowanie QEEG w psychiatrii z uwzględnieniem populacji rozwojowej. Psychiatr Psychol Klin. 2016; 16: 188–193.
26.
Caviness JN, Hentz JG, Belden CM, et al. Longitudinal EEG changes correlate with cognitive measure deterioration in Parkinson’s disease. J Parkinsons Dis. 2015; 5: 117–24.
27.
Caviness JN, Utianski RL, Hentz JG. Differential spectral quantitative electroencephalography patterns between control and Parkinson’s disease cohorts. Eur J Neurol. 2016; 23: 387–92.
28.
Cozac VV, Chaturvedi M, Hatz F, et al. Increase of EEG Spectral Theta Power Indicates Higher Risk of the Development of Severe Cognitive Decline in Parkinson’s Disease after 3 Years. Front Aging Neurosci. 2016; 8: 284.
29.
Cozac VV, Gschwandtner U, Hatz F, et al. Quantitative EEG and Cog-nitive Decline in Parkinson’s Disease. Parkinsons Dis. 2016; 2016: 9060649.
30.
Ferreira D, Jelic V, Cavallin L, et al. Electroencephalography Is a Good Complement to Currently Established Dementia Biomarkers. Dement Geriatr Cogn Disord. 2016; 42: 80–92.
31.
Verrusio W, Ettorre E, Vicenzini E, et al. The Mozart Effect: A quanti-tative EEG study. Conscious Cogn. 2015; 35: 150–5.
32.
McVoy M, Lytle S, Fulchiero E, et al. A systematic review of quantitative EEG as a possible biomarker in child psychiatric disorders. Psychiatry Res. 2019; 279: 331–344.
33.
Hatz F, Meyer A, Zimmermann R, et al. Apathy in Patients with Parkinson’s Disease Correlates with Alteration of Left Fronto-Polar Electroencephalographic Connectivity. Front Aging Neurosci. 2017; 9: 262.
34.
Rommel AS, Kitsune GL, Michelini G, et al. Commonalities in EEG Spectral Power Abnormalities Between Women With ADHD and Wo-men With Bipolar Disorder During Rest and Cognitive Performance. Brain Topogr. 2016; 29: 856–866.
35.
M. Pinkowicka. Wpływ treningu EEG-Biofeedback na wybrane funkcje poznawcze u dzieci. Psychiatria. 2015; 12(4): 255–264.
36.
Pasternak J, Perenc L, Radochoński M. Podstawy psychopatologii dla pedagogów. Rzeszów: Wydawnictwo UR; 2017. p. 256–258.
37.
van Dongen-Boomsma M, Lansbergen M M, Bekker E M, Sandra Kooij, et al. Relation between resting EEG to cognitive performance and clinical symptoms in adults with attentiondeficit/hyperactivity disorder. Neurosci. Lett. 2010; 469: 102–106.
38.
Tye C, Rijsdijk F, McLoughlin G. Genetic overlap between ADHD symptoms and EEG theta power. Brain Cogn. 2014; 87: 168–172.
39.
Thomas BL, Viljoen M. EEG brain wave activity at rest and during evo-ked attention in children with attention-deficit/hyperactivity disorder and effects of methylphenidate. Neuropsychobiology. 2016; 73: 16–22.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.