RESEARCH PAPER
Does bariatric surgery improve patients’ quality of life?
1
Wydział Medyczno-Społeczny, Wyższa Szkoła Planowania Strategicznego w Dąbrowie Górniczej, Polska
2
Szkoła Doktorska, Śląski Uniwersytet Medyczny w Katowicach, Polska
3
Katedra i Oddział Kliniczny Ginekologii i Położnictwa w Rudzie Śląskiej, Wydział Nauk o Zdrowiu w Katowicach, Śląski
Uniwersytet Medyczny w Katowicach, Polska
Corresponding author
Agata Grochal
Szkoła Doktorska, Śląski Uniwersytet Medyczny w Katowicach, ul. Poniatowskiego 15, 40-055 Katowice, Polska
Szkoła Doktorska, Śląski Uniwersytet Medyczny w Katowicach, ul. Poniatowskiego 15, 40-055 Katowice, Polska
Med Og Nauk Zdr. 2023;29(4):316-321
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The study of the quality of life is based on the impact of obesity-related illness on various spheres of life of an individual. Obesity is a state of an excessive accumulation of body fat which leads to the deterioration of health. The aim of the study was to subjectively assess the impact of bariatric surgery on patients’ quality of life.
Material and methods:
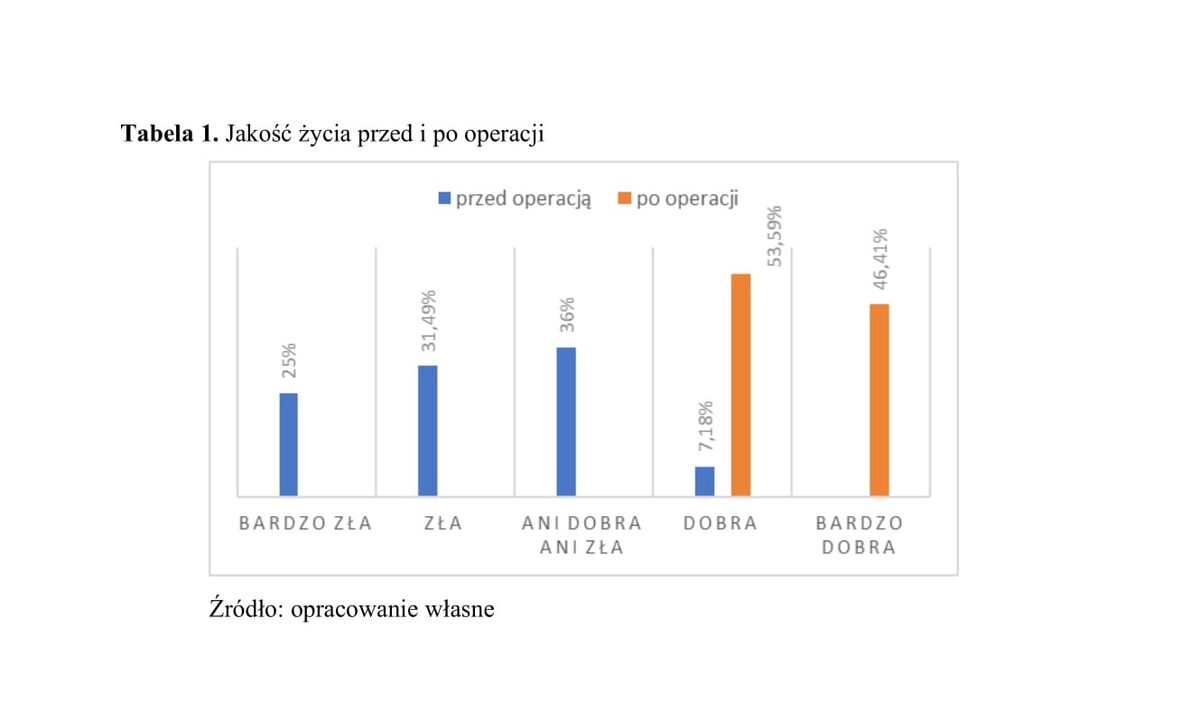
The survey was administered to 181 people who were struggling with obesity and had undergone bariatric surgery. The survey was conducted with reference to two time intervals: before surgery and during the last four weeks. An author-constructed questionnaire was used, which included sociodemographic characteristics of the group, along with questions about obesity, comorbidities, time before and after bariatric surgery, augmented by the standardised WHOQOL – BREF quality of life questionnaire. Results Among the respondents, women were the most numerous group, accounting for as much as 77.3%. The largest group was aged between 36–45 years; mean age 39.9. While determining the quality of life before the surgery, only 13 respondents described their quality of life as good. The others described their quality of life neutrally, or as poor and very poor. Within the last 4 weeks, the respondents’ quality of life was higher in the somatic and psychological spheres, compared to the environmental and social spheres.
Results:
The quality of life of obese people is at a low level, while in patients after bariatric surgery it improved to an average level mainly in the somatic and psychological domains. On the other hand, quality of life in the environmental and social domains increased with time at least 6 months after bariatric surgery.
The study of the quality of life is based on the impact of obesity-related illness on various spheres of life of an individual. Obesity is a state of an excessive accumulation of body fat which leads to the deterioration of health. The aim of the study was to subjectively assess the impact of bariatric surgery on patients’ quality of life.
Material and methods:
The survey was administered to 181 people who were struggling with obesity and had undergone bariatric surgery. The survey was conducted with reference to two time intervals: before surgery and during the last four weeks. An author-constructed questionnaire was used, which included sociodemographic characteristics of the group, along with questions about obesity, comorbidities, time before and after bariatric surgery, augmented by the standardised WHOQOL – BREF quality of life questionnaire. Results Among the respondents, women were the most numerous group, accounting for as much as 77.3%. The largest group was aged between 36–45 years; mean age 39.9. While determining the quality of life before the surgery, only 13 respondents described their quality of life as good. The others described their quality of life neutrally, or as poor and very poor. Within the last 4 weeks, the respondents’ quality of life was higher in the somatic and psychological spheres, compared to the environmental and social spheres.
Results:
The quality of life of obese people is at a low level, while in patients after bariatric surgery it improved to an average level mainly in the somatic and psychological domains. On the other hand, quality of life in the environmental and social domains increased with time at least 6 months after bariatric surgery.
REFERENCES (25)
1.
Ostrowska L, Zyśk B. Definicja, epidemiologia i diagnostyka choroby otyłościowej. In: Ostrowska L, Bogdański P, Mamcarz A, editor. Otyłość i jej powikłania. Praktyczne zalecenia diagnostyczne i terapeutyczne. Warszawa: PZWL Wydawnictwo Lekarskie; 2021. p. 3–51.
2.
Muchacka R, Cebula N. Nadwaga i otyłość – ogólnoświatowa epidemia. Prace Naukowe WSZiP. 2017;42:75–85.
3.
Courcoulas AP, Schauer PR. The Surgical Management of Obesity. In: Brunicardi F, Andersen DK, Billiar TR, Dunn DL, Kao LS, Hunter JG, Matthews JB, Pollock RE. Schwartz's Principles of Surgery. 11th ed. McGraw Hill; 2019. Web sites: https://accesssurgery.mhmedica... (data wejścia: 20/09/2022).
4.
Shawe J, Ceulemans D, Akhter Z, et al. Pregnancy after bariatric surgery: Consensus recommendations for periconception, antenatal and postnatal care. Obes Rev. 2019 Nov;20(11):1507–1522. doi: 10.1111/obr.12927.
5.
Stanowski E, Wyleżoł M. Rozwój chirurgicznego leczenia otyłości na świecie i w Polsce. Postępy Nauk Medycznych. 2009;7:498–501.
6.
WHOQOL Group. The World Health Organisation quality of life assessment (WHOQOL): Position paper from the world health organisation. Soc Sci Med. 1995;41:1403–1409.
7.
Rolka H, Kowalewska B, Jankowiak B. Jakość a jakość życia w ujęciu historycznym. In: Kowalewska B, Jankowiak B, Rolka H, Krajewska-Kułak E, editor. Jakość życia w naukach medycznych i społecznych. T1. Białystok: Uniwersytet Medyczny w Białymstoku; 2017. p. 31–42.
8.
Wiśniewska E, Zagroba M, Ostrowska B, et al. Jakość życia w zdrowiu i w chorobie – charakterystyka pojęcia. In: Kowalewska B, Jankowiak B, Rolka H, Krajewska-Kułak E. editor. Jakość życia w naukach medycznych i społecznych. T1. Białystok: Uniwersytet Medyczny w Białymstoku; 2017. p. 43–52.
9.
Majkowicz M. Metodologiczne podstawy oceny jakości życia. Medycyna Paliatywna w Praktyce. 2017;11(2):78–83.
10.
Versteegden DPA, Van Himbeeck MJJ, Nienhuijs SW. Improvement in quality of life after bariatric surgery: sleeve versus bypass. Surg Obes Relat Dis. 2018 Feb;14(2):170–174.
11.
Castanha CR, Tcbc-Pe ÁABF, Castanha AR, et al. Evaluation of quality of life, weight loss and comorbidities of patients undergoing bariatric surgery. Rev Col Bras Cir. 2018 Jul 16;45(3):e1864. Portuguese, English. doi: 10.1590/0100-6991e-20181864.
13.
Homer CV, Tod AM, Thompson AR, et al. Expectations and patients’ experiences of obesity prior to bariatric surgery: a qualitative study BMJ Open 2016; 6.
14.
Wolfe BM, Kvach E, Eckel RH. Treatment of Obesity: Weight Loss and Bariatric Surgery. Circ Res. 2016 May 27;118(11):1844–55. doi: 10.1161/CIRCRESAHA.116.307591.
15.
Kolotkin RL, Andersen JR. A systematic review of reviews: Exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7:273–289.
16.
Halina Zielińska-Więczkowska, Milena Budnik, Analiza jakości życia pacjentów z nadwagą i otyłością w zależności od wskaźnika masy ciała i czynników socjo-demograficznych, Farmacja Współczesna. 2016;9:110–116.
17.
Sierżantowicz R, Ładny JR, Lewko J. Quality of Life after Bariatric Surgery-A Systematic Review. Int J Environ Res Public Health. 2022 Jul 26;19(15):9078. doi:10.3390/ijerph19159078.
18.
Martinelli V, Chiappedi M. Bariatric Surgery: Psychosocial Aspects and Quality of Life. Int J Environ Res Public Health. 2022 Dec 8;19(24):16516. doi:10.3390/ijerph192416516.
19.
Coulman KD, Blazeby JM. Health-Related Quality of Life in Bariatric and Metabolic Surgery. Curr Obes Rep. 2020 Sep;9(3):307–314. doi:10.1007/s13679-020-00392-z.
20.
Gilmartin J, Bath-Hextall F, Maclean J, et al. Quality of life among adults following bariatric and body contouring surgery: a systematic review. JBI Database System Rev Implement Rep. 2016 Nov;14(11):240–270. doi:10.11124/JBISRIR-2016-003182.
21.
Grönroos S, Helmiö M, Juuti A, et al. Effect of Laparoscopic Sleeve Gastrectomy vs Roux-en-Y Gastric Bypass on Weight Loss and Quality of Life at 7 Years in Patients With Morbid Obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA Surg. 2021 Feb 1;156(2):137–146. doi:10.1001/jamasurg.2020.5666.
22.
Pinheiro JA, Castro IRD, Ribeiro IB, et al. Repercussions of Bariatric Surgery on metabolic parameters: experience of 15-year follow-up in a hospital in Maceio, Brazil. Arq Bras Cir Dig. 2022 Jan 31;34(4).
23.
Małczaka P, Mizera M, Lee Y, et al. Quality of Life After Bariatric Surgery-a Systematic Review with Bayesian Network Meta-analysis. Obes Surg. 2021 Dec;31(12):5213–5223. doi:10.1007/s11695-021-05687-1.
24.
Driscoll S, Gregory DM, Fardy JM, et al. Long-term health-related quality of life in bariatric surgery patients: A systematic review and meta-analysis. Obesity (Silver Spring). 2016 Jan;24(1):60–70. doi:10.1002/oby.21322.
25.
Alotaibi AA, Almutairy AN, Alsaab AS. Post-Bariatric Surgery Patients: A Quality of Life Assessment in Saudi Arabia. Cureus. 2022 Apr 19;14(4):e24273. doi:10.7759/cureus.24273.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.