Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA ORYGINALNA
Wyniki rewaskularyzacji za pomocą przezskórnej interwencji wieńcowej u pacjentów w wieku podeszłym oraz charakterystyka zwężeń w tętnicach wieńcowych w tej populacji – retrospektywne badanie kohortowe
1
1st Department and Clinic of Cardiology, Medical University, Warsaw, Poland
Autor do korespondencji
Mateusz Wawrzeńczyk
I Katedra i Klinika Kardiologii, Warszawski Uniwersytet Medyczny, Banacha 1a, 02-097, Warsaw, Polska
I Katedra i Klinika Kardiologii, Warszawski Uniwersytet Medyczny, Banacha 1a, 02-097, Warsaw, Polska
Med Og Nauk Zdr. 2023;29(3):187-195
SŁOWA KLUCZOWE
przeskórna interwencja wieńcowaosoby w wieku podeszłymśmiertelnośćchoroba wieńcowazespół kruchościwyniki leczenia
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Przezskórna interwencja wieńcowa (PCI) to metoda z wyboru w leczeniu ostrych zespołów wieńcowych i choroby wieńcowej. Tymczasem osoby w wieku podeszłym, ze zwiększonym ryzykiem zespołu kruchości, są często pomijane w kwalifikacji do tej inwazyjnej formy leczenia. Nasze badanie służy ocenie wyników zastosowania PCI w tej populacji oraz określeniu cech istotnych zwężeń obserwowanych u tych pacjentów.
Materiał i metody:
Przeprowadziliśmy retrospektywną analizę wyników leczenia za pomocą PCI populacji 150 pacjentów w wieku ≥ 70 lat hospitalizowanych w naszym ośrodku od listopada 2020 do grudnia 2021 roku. Zbadaliśmy również, jak wpływają na te wyniki czynniki takie jak płeć, BMI czy obciążenia określone przy przyjęciu do szpitala, takie jak zaburzenia lipidowe, nadciśnienie tętnicze lub cukrzyca.
Wyniki:
W badanej populacji średnia wieku wynosiła 77,5 ± 7,1 roku; 65,33% pacjentów stanowili mężczyźni. Średnie BMI miało wartość 27,5 ± 4,3; przy czym 92,00% pacjentów miało nadciśnienie. Większość pacjentów (n = 84) przeszła PCI z powodu ostrych zespołów wieńcowych, a średnia długość stentów wynosiła 31 mm. Skuteczność procedury oceniona jako 3 w skali TIMI została osiągnięta w 94,67% przypadków. Śmiertelność pacjentów łącznie w trakcie procedury oraz do wypisu ze szpitala wyniosła 2,67%.
Wnioski:
PCI jest inwazyjną metodą leczenia ostrych zespołów wieńcowych i przewlekłej choroby wieńcowej, która z powodzeniem może być stosowana u osób w wieku podeszłym, u których występuje zwiększone ryzyko zespołu kruchości. Sam wiek nie może powodować dyskwalifikacji pacjentów, a płeć i BMI są czynnikami mającymi wpływ na wyniki leczenia, dlatego je również należy wziąć pod uwagę, kierując osoby w wieku podeszłym na leczenie za pomocą PCI.
Przezskórna interwencja wieńcowa (PCI) to metoda z wyboru w leczeniu ostrych zespołów wieńcowych i choroby wieńcowej. Tymczasem osoby w wieku podeszłym, ze zwiększonym ryzykiem zespołu kruchości, są często pomijane w kwalifikacji do tej inwazyjnej formy leczenia. Nasze badanie służy ocenie wyników zastosowania PCI w tej populacji oraz określeniu cech istotnych zwężeń obserwowanych u tych pacjentów.
Materiał i metody:
Przeprowadziliśmy retrospektywną analizę wyników leczenia za pomocą PCI populacji 150 pacjentów w wieku ≥ 70 lat hospitalizowanych w naszym ośrodku od listopada 2020 do grudnia 2021 roku. Zbadaliśmy również, jak wpływają na te wyniki czynniki takie jak płeć, BMI czy obciążenia określone przy przyjęciu do szpitala, takie jak zaburzenia lipidowe, nadciśnienie tętnicze lub cukrzyca.
Wyniki:
W badanej populacji średnia wieku wynosiła 77,5 ± 7,1 roku; 65,33% pacjentów stanowili mężczyźni. Średnie BMI miało wartość 27,5 ± 4,3; przy czym 92,00% pacjentów miało nadciśnienie. Większość pacjentów (n = 84) przeszła PCI z powodu ostrych zespołów wieńcowych, a średnia długość stentów wynosiła 31 mm. Skuteczność procedury oceniona jako 3 w skali TIMI została osiągnięta w 94,67% przypadków. Śmiertelność pacjentów łącznie w trakcie procedury oraz do wypisu ze szpitala wyniosła 2,67%.
Wnioski:
PCI jest inwazyjną metodą leczenia ostrych zespołów wieńcowych i przewlekłej choroby wieńcowej, która z powodzeniem może być stosowana u osób w wieku podeszłym, u których występuje zwiększone ryzyko zespołu kruchości. Sam wiek nie może powodować dyskwalifikacji pacjentów, a płeć i BMI są czynnikami mającymi wpływ na wyniki leczenia, dlatego je również należy wziąć pod uwagę, kierując osoby w wieku podeszłym na leczenie za pomocą PCI.
Introduction and objective:
Percutaneous coronary intervention (PCI) is the method of choice for the treatment of coronary artery disease or acute coronary syndromes, but clinicians often refrain from performing it on elderly and/or frail patients. The aimed of the study was to determine the feasibility of PCI in the elderly, and define characteristics of significant stenoses and clinical outcomes of those procedures.
Material and methods:
A retrospective analysis was conducted on a total of 150 patients aged ≥70 years, who were admitted and underwent PCI between November 2020 – December.2021. Also investgated was the impact of patients’ baseline characteristics, such as: gender, body mass index (BMI) or comorbidities: hyperlipidaemia, hypertension, diabetes, etc. on clinical outcomes of PCI performed in the elderly.
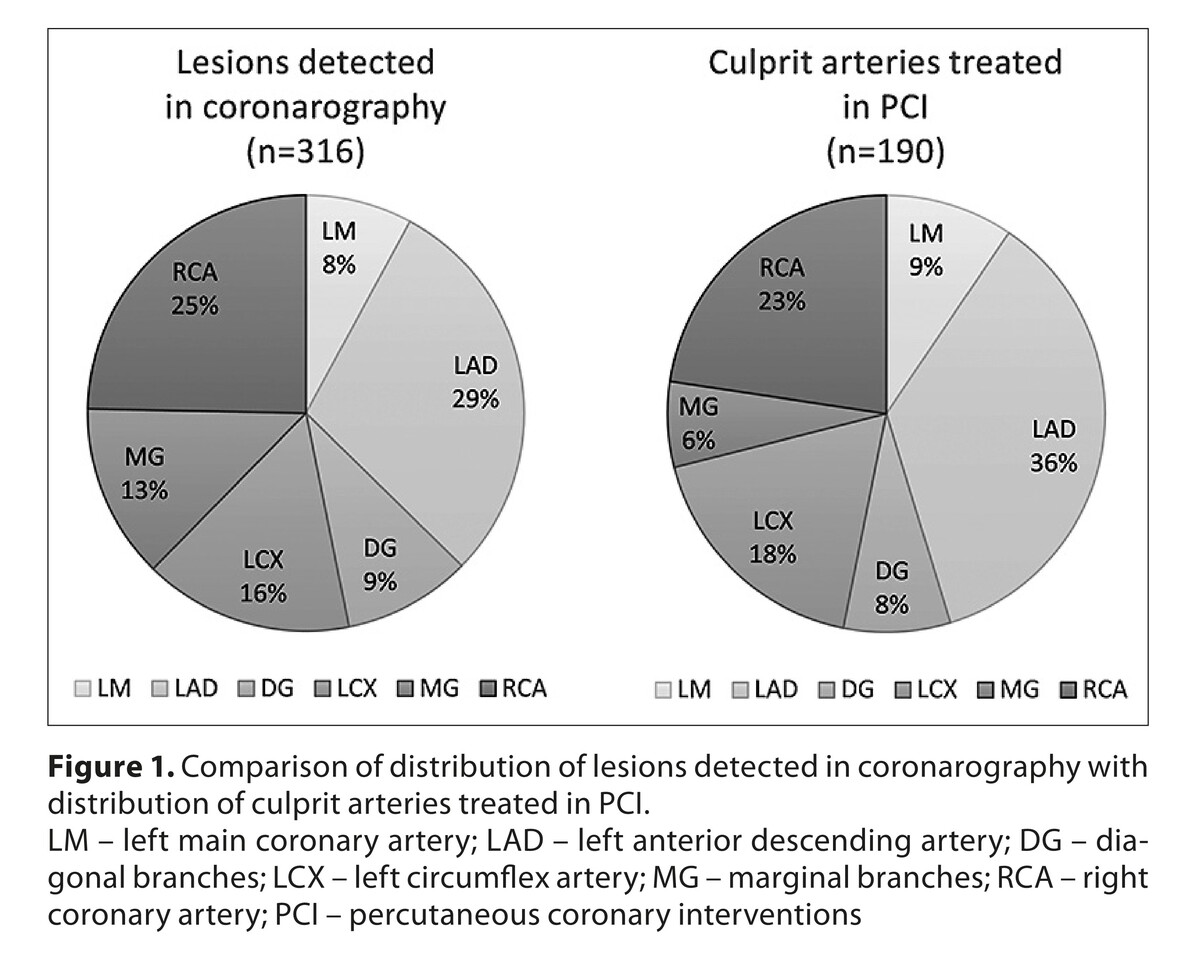
Results:
The mean age was 77.5 ± 7.1 years, 65.33% were male. The average BMI was 27.5 ± 4.3, 92.00% had a history of HT. The majority of patients (n=84) were treated for acute coronary syndromes (ACS). The mean length of stents implanted in one procedure was 31mm. The TIMI 3 flow was achieved in 94.67% of cases. Combined intra-procedural and in-hospital mortality was 2.67%.
Conclusions:
Complex PCI may be successfully and safely performed among elderly patients who frequently suffer from severe myocardial ischemia and carry a substantial comorbidity burden. Age itself cannot warrant disqualification from interventional management of coronary artery disease. Gender and BMI are potential factors that influence clinical outcomes.
Percutaneous coronary intervention (PCI) is the method of choice for the treatment of coronary artery disease or acute coronary syndromes, but clinicians often refrain from performing it on elderly and/or frail patients. The aimed of the study was to determine the feasibility of PCI in the elderly, and define characteristics of significant stenoses and clinical outcomes of those procedures.
Material and methods:
A retrospective analysis was conducted on a total of 150 patients aged ≥70 years, who were admitted and underwent PCI between November 2020 – December.2021. Also investgated was the impact of patients’ baseline characteristics, such as: gender, body mass index (BMI) or comorbidities: hyperlipidaemia, hypertension, diabetes, etc. on clinical outcomes of PCI performed in the elderly.
Results:
The mean age was 77.5 ± 7.1 years, 65.33% were male. The average BMI was 27.5 ± 4.3, 92.00% had a history of HT. The majority of patients (n=84) were treated for acute coronary syndromes (ACS). The mean length of stents implanted in one procedure was 31mm. The TIMI 3 flow was achieved in 94.67% of cases. Combined intra-procedural and in-hospital mortality was 2.67%.
Conclusions:
Complex PCI may be successfully and safely performed among elderly patients who frequently suffer from severe myocardial ischemia and carry a substantial comorbidity burden. Age itself cannot warrant disqualification from interventional management of coronary artery disease. Gender and BMI are potential factors that influence clinical outcomes.
Wawrzeńczyk M, Kuciński J, Kuleta K, Baruś P, Gumiężna K, Pietrasik A, Huczek Z, Grabowski M, Kochman J, Tomaniak M. Association between
baseline characteristics and clinical outcomes among the elderly undergoing PCI: retrospective cohort study. Med Og Nauk Zdr. 2023; 29(3):
187–195. doi: 10.26444/monz/169255
REFERENCJE (45)
1.
Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):e254-e743. https://dx.doi.org/10.1161/CIR....
2.
Gu D, Qu J, Zhang H, et al. Revascularization for Coronary Artery Disease: Principle and Challenges. Adv Exp Med Biol. 2020;1177:75–100. https://dx.doi.org/10.1007/978....
3.
Brenes-Salazar JA, Forman DE Advances in percutaneous coronary interventions for elderly patients. Prog Cardiovasc Dis. 2014;57(2):176–186. https://dx.doi.org/10.1016/j.p....
4.
Shanmugam VB, Harper R, Meredith I, et al. An overview of PCI in the very elderly. J Geriatr Cardiol. 2015;12(2):174–184. https://dx.doi.org/10.11909/j.....
5.
Guo L, Lv HC, Huang RC Percutaneous Coronary Intervention in Elderly Patients with Coronary Chronic Total Occlusions: Current Evidence and Future Perspectives. Clin Interv Aging. 2020;15:771–781. https://dx.doi.org/10.2147/CIA....
6.
Hannan EL, Racz M, Holmes DR, et al. Impact of completeness of percutaneous coronary intervention revascularization on long-term outcomes in the stent era. Circulation. 2006;113(20):2406–2412. https://dx.doi.org/10.1161/CIR....
7.
Uchmanowicz I, Mlynarska A, Lisiak M, et al. Heart Failure and Problems with Frailty Syndrome: Why it is Time to Care About Frailty Syndrome in Heart Failure. Card Fail Rev. 2019;5(1):37–43. https://dx.doi.org/10.15420/cf....
8.
Sanchez E, Vidan MT, Serra JA, et al. Prevalence of geriatric syndromes and impact on clinical and functional outcomes in older patients with acute cardiac diseases. Heart. 2011;97(19):1602–1606. https://dx.doi.org/10.1136/hrt....
9.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. [2018 ESC/EACTS Guidelines on myocardial revascularization. The Task Force on myocardial revascularization of the European Society of Cardiology (ESC) and European Association for Cardio-Thoracic Surgery (EACTS)]. G Ital Cardiol (Rome). 2019;20(7–8 Suppl 1):1S–61S. https://dx.doi.org/10.1714/320....
10.
Yuan L, Chang M, Wang J Abdominal obesity, body mass index and the risk of frailty in community-dwelling older adults: a systematic review and meta-analysis. Age Ageing. 2021;50(4):1118–1128. https://dx.doi.org/10.1093/age....
11.
Van de Werf F Reperfusion treatment in acute myocardial infarction in elderly patients. Kardiol Pol. 2018;76(5):830–837. https://dx.doi.org/10.5603/KP.....
12.
Wang JL, Guo CY, Chen H, et al. Improvement of long-term clinical outcomes by successful PCI in the very elderly women with ACS. BMC Cardiovasc Disord. 2021;21(1):122. https://dx.doi.org/10.1186/s12....
13.
Kim JH, Choi W, Kim KC, et al. The Current Status of Intervention for Intermediate Coronary Stenosis in the Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circ J. 2019;49(11):1022–1032. https://dx.doi.org/10.4070/kcj....
14.
Antoni ML, Yiu KH, Atary JZ, et al. Distribution of culprit lesions in patients with ST-segment elevation acute myocardial infarction treated with primary percutaneous coronary intervention. Coron Artery Dis. 2011;22(8):533–536. https://dx.doi.org/10.1097/MCA....
15.
Wasilewski J, Roleder M, Niedziela J, et al. The role of septal perforators and „myocardial bridging effect” in atherosclerotic plaque distribution in the coronary artery disease. Pol J Radiol. 2015;80:195–201. https://dx.doi.org/10.12659/PJ....
16.
Kim MC, Ahn Y, Sun Sim D, et al. Comparison of the planned one- and elective two-stent techniques in patients with coronary bifurcation lesions with or without acute coronary syndrome from the COBIS II Registry. Catheter Cardiovasc Interv. 2018;92(6):1050–1060. https://dx.doi.org/10.1002/ccd....
17.
Nasir M, Shafique HM, Hussain S, et al. Percutaneous Coronary Intervention for Left Main Coronary Artery Bifurcation Lesions: Two-stent versus one-stent Strategy for Comparison of 6-month MACE. J Coll Physicians Surg Pak. 2020;30(9):894–899. https://dx.doi.org/10.29271/jc....
18.
Arif S, Bartus S, Rakowski T, et al. Comparison of radiation dose exposure in patients undergoing percutaneous coronary intervention vs. peripheral intervention. Postepy Kardiol Interwencyjnej. 2014;10(4):308–313. https://dx.doi.org/10.5114/pwk....
19.
Ekenback C, Jokhaji F, Ostlund-Papadogeorgos N, et al. Changes in Index of Microcirculatory Resistance during PCI in the Left Anterior Descending Coronary Artery in Relation to Total Length of Implanted Stents. J Interv Cardiol. 2019;2019:1397895. https://dx.doi.org/10.1155/201....
20.
Januszek RA, Bryniarski L, Siudak Z, et al. Predictors and trends of contrast use and radiation exposure in a large cohort of patients treated with percutaneous coronary interventions: Chronic total occlusion analysis based on a national registry. Cardiol J. 2021. https://dx.doi.org/10.5603/CJ.....
21.
World Health O: WHO clinical consortium on healthy ageing: topic focus: frailty and intrinsic capacity: report of consortium meeting,1–2 December 2016 in Geneva, Switzerland. In. Geneva: World Health Organization; 2017.
22.
Salaffi F, Farah S, Di Carlo M. Frailty syndrome in rheumatoid arthritis and symptomatic osteoarthritis: an emerging concept in rheumatology. Acta Biomed. 2020;91(2):274–296. https://dx.doi.org/10.23750/ab....
23.
Kane AE, Howlett SE Sex differences in frailty: Comparisons between humans and preclinical models. Mech Ageing Dev. 2021;198:111546. https://dx.doi.org/10.1016/j.m....
24.
Kosmidou I, Leon MB, Zhang Y, et al. Long-Term Outcomes in Women and Men Following Percutaneous Coronary Intervention. J Am Coll Cardiol. 2020;75(14):1631–1640. https://dx.doi.org/10.1016/j.j....
25.
Lee CY, Liu KT, Lu HT, et al. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry. PLoS One. 2021;16(2):e0246474. https://dx.doi.org/10.1371/jou....
26.
Birkemeyer R, Schneider H, Rillig A, et al. Do gender differences in primary PCI mortality represent a different adherence to guideline recommended therapy? a multicenter observation. BMC Cardiovasc Disord. 2014;14:71. https://dx.doi.org/10.1186/147....
27.
Guelker JE, Bansemir L, Ott R, et al. Gender-based acute outcome in percutaneous coronary intervention of chronic total coronary occlusion. Neth Heart J. 2017;25(5):304–311. https://dx.doi.org/10.1007/s12....
28.
Tang L, Cui QW, Liu DP, et al. The number of stents was an independent risk of stent restenosis in patients undergoing percutaneous coronary intervention. Medicine (Baltimore). 2019;98(50):e18312. https://dx.doi.org/10.1097/md.....
29.
Li Q, Liu S, Myers KJ, et al. Impact of Reconstruction Algorithms and Gender-Associated Anatomy on Coronary Calcium Scoring with CT: An Anthropomorphic Phantom Study. Acad Radiol. 2016;23(12):1470–1479. https://dx.doi.org/10.1016/j.a....
30.
Siudak Z, Bryniarski L, Malinowski KP, et al. Procedural Outcomes in Patients Treated with Percutaneous Coronary Interventions within Chronic Total Occlusions Stratified by Gender. J Clin Med. 2022;11(5). https://dx.doi.org/10.3390/jcm....
31.
Watanabe D, Yoshida T, Watanabe Y, et al. A U-Shaped Relationship Between the Prevalence of Frailty and Body Mass Index in Community-Dwelling Japanese Older Adults: The Kyoto-Kameoka Study. J Clin Med. 2020;9(5). https://dx.doi.org/10.3390/jcm....
32.
Khan SS, Ning H, Wilkins JT, et al. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018;3(4):280–287. https://dx.doi.org/10.1001/jam....
33.
Crowhurst J, Savage M, Hay K, et al. Impact of Patient BMI on Patient and Operator Radiation Dose During Percutaneous Coronary Intervention. Heart Lung Circ. 2022;31(3):372–382. https://dx.doi.org/10.1016/j.h....
34.
Jankowska-Polańska B, Zamęta K, Uchmanowicz I, et al. Adherence to pharmacological and non-pharmacological treatment of frail hypertensive patients. J Geriatr Cardiol. 2018;15(2):153–161. https://dx.doi.org/10.11909/j.....
35.
Kala P, Kanovsky J, Rokyta R, et al. Age-related treatment strategy and long-term outcome in acute myocardial infarction patients in the PCI era. BMC Cardiovasc Disord. 2012;12:31. https://dx.doi.org/10.1186/147....
36.
Vetrano DL, Palmer KM, Galluzzo L, et al. Hypertension and frailty: a systematic review and meta-analysis. BMJ Open. 2018;8(12):e024406. https://dx.doi.org/10.1136/bmj....
37.
Mouton AJ, Li X, Hall ME, et al. Obesity, Hypertension, and Cardiac Dysfunction: Novel Roles of Immunometabolism in Macrophage Activation and Inflammation. Circ Res. 2020;126(6):789–806. https://dx.doi.org/10.1161/cir....
38.
Röhrig G, Anemia in the frail, elderly patient. Clin Interv Aging. 2016;11:319–326. https://dx.doi.org/10.2147/cia....
39.
Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–1516. https://dx.doi.org/10.1056/NEJ....
40.
Iannaccone M, D'Ascenzo F, Piazza F, et al. Optimal medical therapy vs. coronary revascularization for patients presenting with chronic total occlusion: A meta-analysis of randomized controlled trials and propensity score adjusted studies. Catheter Cardiovasc Interv. 2019;93(6):E320–E325. https://dx.doi.org/10.1002/ccd....
41.
Shaw LJ, Berman DS, Maron DJ, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117(10):1283–1291. https://dx.doi.org/10.1161/CIR....
42.
Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 2018;39(26):2484–2493. https://dx.doi.org/10.1093/eur....
43.
Eisenberg MJ, Afilalo J, Lawler PR, et al. Cancer risk related to low -dose ionizing radiation from cardiac imaging in patients after acute myocardial infarction. CMAJ. 2011;183(4):430–436. https://dx.doi.org/10.1503/cma....
44.
Kim DW, Her SH, Park MW, et al. Impact of Postprocedural TIMI Flow on Long-Term Clinical Outcomes in Patients with Acute Myocardial Infarction. Int Heart J. 2017;58(5):674–685. https://dx.doi.org/10.1536/ihj....
45.
Chiarito M, Cao D, Nicolas J, et al. Radial versus femoral access for coronary interventions: An updated systematic review and meta-analysis of randomized trials. Catheter Cardiovasc Interv. 2021;97(7):1387–1396. https://dx.doi.org/10.1002/ccd....
Udostępnij
ARTYKUŁ POWIĄZANY
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.