Online first
Bieżący numer
Archiwum
O czasopiśmie
Polityka etyki publikacyjnej
System antyplagiatowy
Instrukcje dla Autorów
Instrukcje dla Recenzentów
Rada Redakcyjna
Komitet Redakcyjny
Recenzenci
Wszyscy recenzenci
2024
2023
2022
2021
2020
2019
2018
2017
2016
Kontakt
Bazy indeksacyjne
Klauzula przetwarzania danych osobowych (RODO)
PRACA PRZEGLĄDOWA
Leki przeciwdrgawkowe stosowane w zaburzeniach związanych z nadużywaniem alkoholu
1
5th year student, Faculty of Medicine, Medical University, Lublin, Poland
2
6th year student, Faculty of Medicine, Medical University, Lublin, Poland
3
Department of Histology, Embryology and Cytophysiology, Medical University, Lublin, Poland
Med Og Nauk Zdr. 2024;30(3):186-191
SŁOWA KLUCZOWE
DZIEDZINY
STRESZCZENIE
Wprowadzenie i cel:
Niniejszy artykuł miał na celu przegląd piśmiennictwa w poszukiwaniu leków przeciwdrgawkowych stosowanych w leczeniu zaburzeń związanych z nadużywaniem alkoholu. Stały się one przedmiotem badań jako alternatywa dla obecnej terapii, której celem jest uzyskanie trwałej abstynencji lub wywołanych alkoholem.
Metody przeglądu:
Przeglądu literatury dokonano przy użyciu bazy danych PubMed i Google Scholar. Przeanalizowano publikacje z lat 2015–2024, a jako kryteria wyszukiwania zastosowano następujące słowa kluczowe: „zaburzenia związane z używaniem alkoholu”, „zespół abstynencyjny”, „leki przeciwdrgawkowe”.
Opis stanu wiedzy:
Zaburzenia związane z używaniem alkoholu mogą objawiać się jako nawracające i gwałtowne pragnienie jego spożywania, a także jako przewlekłe intensywne picie, a wszelkie jego ograniczenia prowadzą do zespołu abstynencyjnego. Nadużywanie alkoholu można zdiagnozować na podstawie kryteriów DSM-5 lub ICD-11. Patogeneza AUD jest związana ze zwiększoną ilością spożywanego etanolu, co prowadzi do nadmiernej aktywności receptorów GABAergicznych i zmniejszonej aktywności receptorów glutaminergicznych. Narzędziem przesiewowym stosowanym w celu wykrywania problemów związanych z nadużywaniem alkoholu jest test AUDIT, podczas gdy negatywne skutki jego odstawienia oceniane są za pomocą protokołu CIWA-AR. Leki przeciwdrgawkowe są aktualnie lekami drugiego rzutu w leczeniu, a najbardziej obiecujące wyniki badań zaobserwowano w przypadku gabapentyny i topiramatu.
Podsumowanie:
Obecnie odnotowuje się pewne korzyści z podawania leków przeciwpadaczkowych w chorobach związanych z nadużywaniem alkoholu, ale ze względu na brak wystarczających badań w tym zakresie nie zaleca się ich rutynowego stosowania. Mogą one być brane pod uwagę, gdy u pacjenta występują choroby współistniejące i nie ma przeciwwskazań do ich przyjmowania.
Niniejszy artykuł miał na celu przegląd piśmiennictwa w poszukiwaniu leków przeciwdrgawkowych stosowanych w leczeniu zaburzeń związanych z nadużywaniem alkoholu. Stały się one przedmiotem badań jako alternatywa dla obecnej terapii, której celem jest uzyskanie trwałej abstynencji lub wywołanych alkoholem.
Metody przeglądu:
Przeglądu literatury dokonano przy użyciu bazy danych PubMed i Google Scholar. Przeanalizowano publikacje z lat 2015–2024, a jako kryteria wyszukiwania zastosowano następujące słowa kluczowe: „zaburzenia związane z używaniem alkoholu”, „zespół abstynencyjny”, „leki przeciwdrgawkowe”.
Opis stanu wiedzy:
Zaburzenia związane z używaniem alkoholu mogą objawiać się jako nawracające i gwałtowne pragnienie jego spożywania, a także jako przewlekłe intensywne picie, a wszelkie jego ograniczenia prowadzą do zespołu abstynencyjnego. Nadużywanie alkoholu można zdiagnozować na podstawie kryteriów DSM-5 lub ICD-11. Patogeneza AUD jest związana ze zwiększoną ilością spożywanego etanolu, co prowadzi do nadmiernej aktywności receptorów GABAergicznych i zmniejszonej aktywności receptorów glutaminergicznych. Narzędziem przesiewowym stosowanym w celu wykrywania problemów związanych z nadużywaniem alkoholu jest test AUDIT, podczas gdy negatywne skutki jego odstawienia oceniane są za pomocą protokołu CIWA-AR. Leki przeciwdrgawkowe są aktualnie lekami drugiego rzutu w leczeniu, a najbardziej obiecujące wyniki badań zaobserwowano w przypadku gabapentyny i topiramatu.
Podsumowanie:
Obecnie odnotowuje się pewne korzyści z podawania leków przeciwpadaczkowych w chorobach związanych z nadużywaniem alkoholu, ale ze względu na brak wystarczających badań w tym zakresie nie zaleca się ich rutynowego stosowania. Mogą one być brane pod uwagę, gdy u pacjenta występują choroby współistniejące i nie ma przeciwwskazań do ich przyjmowania.
Introduction and objective:
This study was designed to review the literature in search of current anticonvulsants for the treatment of alcohol-related diseases. As an alternative to the currently applied medicaments, antiepileptic drugs have become the focus of research so that patients can achieve permanent abstinence or reduce the bothersome alcoholinduced symptoms.
Review methods:
The literature review was conducted using the PubMed and Google Scholar database. Publications from 2015–2024 were analyzed and the following keywords were used as search criteria: „alcohol use disorder,” „alcohol withdrawal syndrome,” „anticonvulsant drugs.”
Brief description of the state of knowledge:
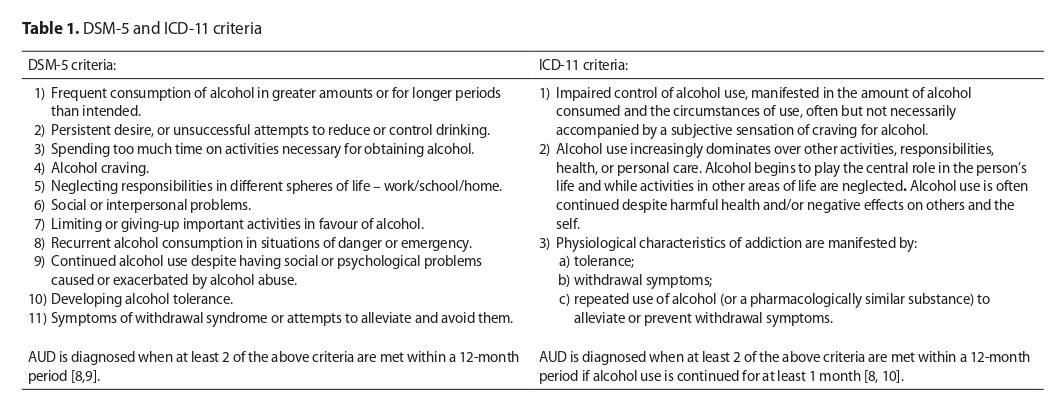
Alcohol use disorder (AUD) can manifest itself as either a recurrent and violent desire to consume alcohol or chronic heavy drinking. While attempting to stop drinking, patients experience the symptoms of alcohol withdrawal syndrome (AWS). Alcohol abuse can be clinically diagnosed on the basis of DSM-5 or ICD-11 criteria. The pathogenesis of AUD is connected with the increased amount of ethanol consumed, the excess of which leads to increased activity of GABAergic receptors and decreased activity of glutamatergic receptors. The AUDIT test was created to screen for problems with significant alcohol abuse, while the negative effects of alcohol withdrawal are assessed by the CIWA-AR protocol. Anticonvulsants are currently second-line drugs for the treatment of alcoholrelated disorders. The most promising study results have been observed with gabapentin and topiramate
Summary:
Currently, some benefits of administering antiepileptic drugs in alcohol-related diseases have been noted, but due to lack of sufficient research their routine use is not recommended. Anticonvulsants can be considered an option when the patient has comorbidities and when there are no contraindications to the drugs applied.
This study was designed to review the literature in search of current anticonvulsants for the treatment of alcohol-related diseases. As an alternative to the currently applied medicaments, antiepileptic drugs have become the focus of research so that patients can achieve permanent abstinence or reduce the bothersome alcoholinduced symptoms.
Review methods:
The literature review was conducted using the PubMed and Google Scholar database. Publications from 2015–2024 were analyzed and the following keywords were used as search criteria: „alcohol use disorder,” „alcohol withdrawal syndrome,” „anticonvulsant drugs.”
Brief description of the state of knowledge:
Alcohol use disorder (AUD) can manifest itself as either a recurrent and violent desire to consume alcohol or chronic heavy drinking. While attempting to stop drinking, patients experience the symptoms of alcohol withdrawal syndrome (AWS). Alcohol abuse can be clinically diagnosed on the basis of DSM-5 or ICD-11 criteria. The pathogenesis of AUD is connected with the increased amount of ethanol consumed, the excess of which leads to increased activity of GABAergic receptors and decreased activity of glutamatergic receptors. The AUDIT test was created to screen for problems with significant alcohol abuse, while the negative effects of alcohol withdrawal are assessed by the CIWA-AR protocol. Anticonvulsants are currently second-line drugs for the treatment of alcoholrelated disorders. The most promising study results have been observed with gabapentin and topiramate
Summary:
Currently, some benefits of administering antiepileptic drugs in alcohol-related diseases have been noted, but due to lack of sufficient research their routine use is not recommended. Anticonvulsants can be considered an option when the patient has comorbidities and when there are no contraindications to the drugs applied.
Góral A, Czachajda M, Żuk K, Duszyńska K, Dolepski K, Lis-Sochocka M. Anticonvulsant drugs for alcohol-related disorders. Med Og Nauk Zdr. 2024; 30(3): 186–191. doi: 10.26444/monz/189992
REFERENCJE (50)
1.
Bahji A, Bach P, Danilewitz M, et al. Pharmacotherapies for Adults With Alcohol Use Disorders: A Systematic Review and Network Meta-analysis. J Addict Med. 2022;16(6):630–638. doi:10.1097/ADM.0000000000000992.
2.
Koob GF. Alcohol Use Disorder Treatment: Problems and Solutions. Annu Rev Pharmacol Toxicol. 2024;64:255–275. doi:10.1146/ANNUREV-PHARMTOX-031323-115847.
3.
Bahji A, Bach P, Danilewitz M, et al. Comparative efficacy and safety of pharmacotherapies for alcohol withdrawal: a systematic review and network meta-analysis. Addiction. 2022;117(10):2591–2601. doi:10.1111/ADD.15853.
4.
Miranda R, O’Malley SS, Treloar Padovano H, et al. Effects of Alcohol Cue Reactivity on Subsequent Treatment Outcomes Among Treatment-Seeking Individuals with Alcohol Use Disorder: A Multisite Randomized, Double-Blind, Placebo-Controlled Clinical Trial of Varenicline. Alcohol Clin Exp Res. 2020;44(7):1431–1443. doi:10.1111/ACER.14352.
5.
Hammond CJ, Niciu MJ, Drew S, et al. Anticonvulsants for the treatment of alcohol withdrawal syndrome and alcohol use disorders. CNS Drugs. 2015;29(4):293–311. doi:10.1007/S40263-015-0240-4.
6.
Choi HY, Seo JS, Lee SK. [Assessment and Treatment of Alcohol Withdrawal Syndrome]. Korean J Gastroenterol. 2020;76(2):71–77. doi:10.4166/KJG.2020.76.2.71.
7.
Attilia F, Perciballi R, Rotondo C, et al. Alcohol withdrawal syndrome: diagnostic and therapeutic methods. Riv Psichiatr. 2018;53(3):118–122. doi:10.1708/2925.29413.
8.
Saunders JB, Degenhardt L, Reed GM, et al. Alcohol Use Disorders in ICD-11: Past, Present, and Future. Alcohol Clin Exp Res. 2019;43(8):1617–1631. doi:10.1111/ACER.14128.
9.
Saha TD, Chou SP, Grant BF. The performance of DSM-5 alcohol use disorder and quantity-frequency of alcohol consumption criteria: An item response theory analysis. Drug Alcohol Depend. 2020;216. doi:10.1016/J.DRUGALCDEP.2020.108299.
10.
Degenhardt L, Bharat C, Bruno R, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: Analysis of data from the WHO’s World Mental Health Surveys. Addiction. 2019;114(3):534. doi:10.1111/ADD.14482.
12.
Liu J, Wang LN. Baclofen for alcohol withdrawal. Cochrane database Syst Rev. 2019;2019(11). doi:10.1002/14651858.CD008502.PUB6.
13.
Morisot N, Ron D. Alcohol-dependent molecular adaptations of the NMDA receptor system. Genes Brain Behav. 2017;16(1):139–148. doi:10.1111/GBB.12363.
14.
Tiglao SM, Meisenheimer ES, Oh RC. Alcohol Withdrawal Syndrome: Outpatient Management. Am Fam Physician. 2021;104(3):253–262.
15.
Muddapah CP, Weich L. Assessing the revised Clinical Institute Withdrawal for Alcohol Scale use at Stikland Hospital. S Afr J Psychiatr. 2023;29. doi:10.4102/SAJPSYCHIATRY.V29I0.1915.
16.
Sanchez-Roige S, Palmer AA, Fontanillas P, et al. Genome-Wide Association Study Meta-Analysis of the Alcohol Use Disorders Identification Test (AUDIT) in Two Population-Based Cohorts. Am J Psychiatry. 2019;176(2):107–118. doi:10.1176/APPI.AJP.2018.18040369.
17.
Grover S, Ghosh A. Delirium Tremens: Assessment and Management. J Clin Exp Hepatol. 2018;8(4):460–470. doi:10.1016/j.jceh.2018.04.012.
18.
Pribék IK, Kovács I, Kádár BK, et al. Evaluation of the course and treatment of Alcohol Withdrawal Syndrome with the Clinical Institute Withdrawal Assessment for Alcohol – Revised: A systematic review-based meta-analysis. Drug Alcohol Depend. 2021;220. doi:10.1016/J.DRUGALCDEP.2021.108536.
19.
Teixeira J. Tratamento Farmacológico da Síndrome de Abstinência Alcoólica [Pharmacological Treatment of Alcohol Withdrawal]. Acta Med Port. 2022;35(4):286–293. doi:10.20344/amp.15799.
20.
Holleck JL, Merchant N, Gunderson CG. Symptom-Triggered Therapy for Alcohol Withdrawal Syndrome: a Systematic Review and Meta-analysis of Randomized Controlled Trials. J Gen Intern Med. 2019;34(6):1018–1024. doi:10.1007/S11606-019-04899-7.
21.
Campbell EJ, Lawrence AJ, Perry CJ. New steps for treating alcohol use disorder. Psychopharmacology (Berl). 2018;235(6):1759–1773. doi:10.1007/S00213-018-4887-7.
22.
Grunze H, Schaefer M, Scherk H, et al. Preuss UW. Comorbid Bipolar and Alcohol Use Disorder—A Therapeutic Challenge. Front Psychiatry. 2021;12:660432. doi:10.3389/FPSYT.2021.660432/BIBTEX.
23.
Depounti A, Goff T. ADDERRAL (AMPHETAMINE/DEXROAMPHETAMINE SALT MIXTURE 1:1) VERSUS TEGRETOL (CARBAMAZEPINE) IN THE TREATMENT AND ALLEVIATION OF SYMPTOMS OF TRIGEMINAL NEURALGIA IN PATIENTS WITH A NOTED HISTORY OF ALCOHOL USE DISORDER. Int J Oral Maxillofac Surg. 2024;52:13. doi:10.1016/j.ijom.2023.10.045.
24.
Kim Y, Hack LM, Ahn ES, et al. Practical outpatient pharmacotherapy for alcohol use disorder. Drugs Context. 2018;7:212308. doi:10.7573/DIC.212308.
25.
Rojo-Mira J, Pineda-Álvarez M, Zapata-Ospina JP. Efficacy and Safety of Anticonvulsants for the Inpatient Treatment of Alcohol Withdrawal Syndrome: A Systematic Review and Meta-analysis. Alcohol Alcohol. 2022;57(2):155–164. doi:10.1093/ALCALC/AGAB057.
26.
De Iuliis V, Gelormini R, Flacco M, et al. Comparison of Serum Total Valproic Acid Levels and %CDT Values in Chronic Alcohol Addictive Patients in an Italian Clinic: A Retrospective Study. Drugs – Real World Outcomes. 2016;3(1):7–12. doi:10.1007/S40801-015-0053-2/TABLES/3.
27.
Latifi S, Messer T. The Efficacy of Tiapride and Carbamazepine Combination Therapy in Reducing Alcohol Withdrawal Symptoms: A Systematic Review and Meta-Analysis. Pharmacopsychiatry. 2019;52(5):209–216. doi:10.1055/A-0795-3689.
28.
Archibald L, Brunette MF, Wallin DJ, et al. Alcohol Use Disorder and Schizophrenia or Schizoaffective Disorder. Alcohol Res. 2019;40(1):e1-e9. doi:10.35946/ARCR.V40.1.06.
29.
Celik M, Gold MS, Fuehrlein B. A Narrative Review of Current and Emerging Trends in the Treatment of Alcohol Use Disorder. Brain Sci. 2024;14(3):294. Published 2024 Mar 20. doi:10.3390/brainsci14030294.
30.
T. Neuropharmacology of Antiseizure Drugs. Neuropsychopharmacol reports. 2021;41(3):336–351. doi:10.1002/NPR2.12196.
31.
Wise J. Valproate: Men planning a family should seek advice in light of neurodevelopmental disorders risk in children, says regulator. BMJ. 2024;384:q122. Published 2024 Jan 16. doi:10.1136/bmj.q122.
32.
Abou-Khalil BW. Update on Antiepileptic Drugs 2019. Continuum (Minneap Minn). 2019;25(2):508–536. doi:10.1212/CON.0000000000000715.
33.
Mariani JJ, Pavlicova M, Basaraba C, et al. Pilot randomized placebo-controlled clinical trial of high-dose gabapentin for alcohol use disorder. Alcohol Clin Exp Res. 2021;45(8). doi:10.1111/ACER.14648.
35.
Anton RF, Latham P, Voronin K, et al. Efficacy of Gabapentin for the Treatment of Alcohol Use Disorder in Patients With Alcohol Withdrawal Symptoms: A Randomized Clinical Trial. JAMA Intern Med. 2020;180(5):728–736. doi:10.1001/JAMAINTERNMED.2020.0249.
36.
Saeed M, Saleem U, Anwar F, et al. Inhibition of Valproic Acid-Induced Prenatal Developmental Abnormalities with Antioxidants in Rats. ACS Omega. 2020;5(10):4953–4961. Published 2020 Mar 2. doi:10.1021/acsomega.9b03792.
37.
Falk DE, Ryan ML, Fertig JB, et al. Gabapentin Enacarbil Extended-Release for Alcohol Use Disorder: A Randomized, Double-Blind, Placebo-Controlled, Multisite Trial Assessing Efficacy and Safety. Alcohol Clin Exp Res. 2019;43(1):158–169. doi:10.1111/ACER.13917.
38.
Mattle AG, McGrath P, Sanu A, et al. Gabapentin to treat acute alcohol withdrawal in hospitalized patients: A systematic review and meta-analysis. Drug Alcohol Depend. 2022;241. doi:10.1016/J.DRUGALCDEP.2022.109671.
39.
Kranzler HR, Feinn R, Morris P, et al. A Meta-analysis of the Efficacy of Gabapentin for Treating Alcohol Use Disorder. doi:10.1111/add.14655.
40.
Ornoy A, Echefu B, Becker M. Valproic Acid in Pregnancy Revisited: Neurobehavioral, Biochemical and Molecular Changes Affecting the Embryo and Fetus in Humans and in Animals: A Narrative Review. Int J Mol Sci. 2023;25(1):390. Published 2023 Dec 27. doi:10.3390/ijms25010390.
41.
Ahmed S, Stanciu CN, Kotapati PV, et al. Effectiveness of Gabapentin in Reducing Cravings and Withdrawal in Alcohol Use Disorder: A Meta-Analytic Review. Prim care companion CNS Disord. 2019;21(4). doi:10.4088/PCC.19R02465.
42.
Wetherill RR, Spilka N, Jagannathan K, et al. Effects of topiramate on neural responses to alcohol cues in treatment-seeking individuals with alcohol use disorder: preliminary findings from a randomized, placebo-controlled trial. Neuropsychopharmacology. 2021;46(8):1414–1420. doi:10.1038/S41386-021-00968-W.
43.
Freynhagen R, Backonja M, Schug S, et al. Pregabalin for the Treatment of Drug and Alcohol Withdrawal Symptoms: A Comprehensive Review. CNS Drugs. 2016;30(12):1191–1200. doi:10.1007/s40263-016-0390-z.
44.
Palpacuer C, Duprez R, Huneau A, et al. Pharmacologically controlled drinking in the treatment of alcohol dependence or alcohol use disorders: a systematic review with direct and network meta-analyses on nalmefene, naltrexone, acamprosate, baclofen and topiramate. Addiction. 2018;113(2):220–237. doi:10.1111/ADD.13974.
45.
Manhapra A, Chakraborty A, Arias AJ. Topiramate Pharmacotherapy for Alcohol Use Disorder and Other Addictions: A Narrative Review. J Addict Med. 2019;13(1):7–22. doi:10.1097/ADM.0000000000000443.
46.
Petrakis I, Ralevski E, Arias AJ, et al. Zonisamide as an Adjunctive Treatment to Cognitive Processing Therapy for Veterans With Posttraumatic Stress Disorder and Comorbid Alcohol Use Disorder: A Pilot Study. Am J Addict. 2020;29(6):515–524. doi:10.1111/AJAD.13061.
47.
Gidal BE, Resnick T, Smith MC, et al. Zonisamide: A Comprehensive, Updated Review for the Clinician. Neurol Clin Pract. 2024;14(1):e200210. doi:10.1212/CPJ.0000000000200210.
48.
Mariani JJ, Pavlicova M, Choi CJ, et al. An open-label pilot study of pregabalin pharmacotherapy for alcohol use disorder. Am J Drug Alcohol Abuse. 2021;47(4):467–475. doi:10.1080/00952990.2021.1901105.
49.
Winslow BT, Onysko M, Hebert M. Medications for Alcohol Use Disorder. Am Fam Physician. 2016;93(6):457–465.
50.
Goodyear K, Miranda R Jr, MacKillop J. Behavioral economic analysis of topiramate pharmacotherapy for alcohol: a placebo-controlled investigation of effects on alcohol reinforcing value and delayed reward discounting. Psychopharmacology (Berl). 2022;239(1):153–161. doi:10.1007/s00213-021-06034-z.
Przetwarzamy dane osobowe zbierane podczas odwiedzania serwisu. Realizacja funkcji pozyskiwania informacji o użytkownikach i ich zachowaniu odbywa się poprzez dobrowolnie wprowadzone w formularzach informacje oraz zapisywanie w urządzeniach końcowych plików cookies (tzw. ciasteczka). Dane, w tym pliki cookies, wykorzystywane są w celu realizacji usług, zapewnienia wygodnego korzystania ze strony oraz w celu monitorowania ruchu zgodnie z Polityką prywatności. Dane są także zbierane i przetwarzane przez narzędzie Google Analytics (więcej).
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.
Możesz zmienić ustawienia cookies w swojej przeglądarce. Ograniczenie stosowania plików cookies w konfiguracji przeglądarki może wpłynąć na niektóre funkcjonalności dostępne na stronie.