RESEARCH PAPER
Analysis of cortisol levels in breast milk and blood serum in women with symptoms of postpartum depression
1
Department of Perinatology, Gynaecology and Gynaecologic Oncology, Faculty of Health Sciences, Ludwik Rydygier Collegium Medicum, Bydgoszcz, Nicolaus Copernicus University, Toruń, Poland
2
Department of Gynaecology and Obstetrics, Ludwik Błażek Multispecialist Hospital, Inowrocław, Poland
3
Department of Pathobiochemistry and Clinical Chemistry, Faculty of Pharmacy, Ludwik Rydygier Collegium Medicum, Bydgoszcz, Nicolaus Copernicus University, Toruń, Poland
Corresponding author
Agnieszka Dombrowska-Pali
Katedra Perinatologii, Ginekologii i Ginekologii Onkologicznej, Wydział Nauk o Zdrowiu, Collegium Medicum im. Ludwika Rydygiera w Bydgoszczy, Uniwersytet Mikołaja Kopernika w Toruniu, Łukasiewicza 1, 85-821, Bydgoszcz, Polska
Katedra Perinatologii, Ginekologii i Ginekologii Onkologicznej, Wydział Nauk o Zdrowiu, Collegium Medicum im. Ludwika Rydygiera w Bydgoszczy, Uniwersytet Mikołaja Kopernika w Toruniu, Łukasiewicza 1, 85-821, Bydgoszcz, Polska
Med Og Nauk Zdr. 2022;28(2):165-171
KEYWORDS
postpartum depressionbreastfeedingEdinburgh Postpartum Depression Scalemilk cortisolserum cortisol concentration
TOPICS
ABSTRACT
Introduction and objective:
Scientific studies report that the risk of symptoms of postpartum depression (PPD) can significantly reduce breastfeeding time. It has not yet been shown whether there is a difference in cortisol levels in breast milk and serum cortisol levels in women at risk of PPD but without symptoms. The aim of the study was assessment of the levels of cortisol in breast milk and levels of serum cortisol in women at risk of PPD four weeks after birth.
Material and methods:
The study included 75 women who were recruited at a University Hospital and via social media. The proper study was conducted in the fourth week after delivery. The research tool used was The Edinburgh Postnatal Depression Scale (EPDS). Assessment of cortisol levels in breast milk was performed with the enzyme-linked immunosorbent assay CORTISOL saliva ELISA DiaMetra. Blood analysis was conducted in an ALAB Laboratory, one of a nationwide network of specialis laboratories.
Results:
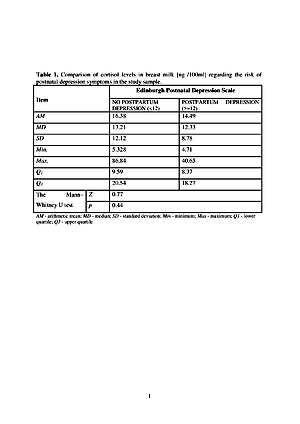
The prevalence of the risk of PPD symptoms in the study sample was estimated at 28% in EPDS. The risk of PPD symptoms does not differentiate between cortisol levels in breast milk and serum cortisol levels (p>0.05). A correlation was shown between the level of cortisol in breast milk and in the blood serum of the study sample (p<0.03).
Conclusions:
The study indicates that the risk of PPD symptoms does not differentiate between serum cortisol levels and cortisol levels in breast milk. The level of cortisol in breast milk reflects the level of cortisol in the blood serum of the subjects.
Scientific studies report that the risk of symptoms of postpartum depression (PPD) can significantly reduce breastfeeding time. It has not yet been shown whether there is a difference in cortisol levels in breast milk and serum cortisol levels in women at risk of PPD but without symptoms. The aim of the study was assessment of the levels of cortisol in breast milk and levels of serum cortisol in women at risk of PPD four weeks after birth.
Material and methods:
The study included 75 women who were recruited at a University Hospital and via social media. The proper study was conducted in the fourth week after delivery. The research tool used was The Edinburgh Postnatal Depression Scale (EPDS). Assessment of cortisol levels in breast milk was performed with the enzyme-linked immunosorbent assay CORTISOL saliva ELISA DiaMetra. Blood analysis was conducted in an ALAB Laboratory, one of a nationwide network of specialis laboratories.
Results:
The prevalence of the risk of PPD symptoms in the study sample was estimated at 28% in EPDS. The risk of PPD symptoms does not differentiate between cortisol levels in breast milk and serum cortisol levels (p>0.05). A correlation was shown between the level of cortisol in breast milk and in the blood serum of the study sample (p<0.03).
Conclusions:
The study indicates that the risk of PPD symptoms does not differentiate between serum cortisol levels and cortisol levels in breast milk. The level of cortisol in breast milk reflects the level of cortisol in the blood serum of the subjects.
REFERENCES (43)
1.
Avilla JC, Giugliani C, Bizon AMBL, et al. Association between maternal satisfaction with breastfeeding and postpartum depression symptoms.
3.
Liu S, Yan Y, Gao X, et al. Risk factors for postpartum depression among Chinese women: path model analysis. BMC Pregnancy &Childbirth. 2017; 17: 133. https://doi.org/10.1186/s12884....
4.
Marshall EM, Simpson JA, Rholes WS. Personality, communication, and depressive symptoms across the transition to parenthood: A dyadic longitudinal investigation. Eur J Pers. 2015; 29(2): 216–234. https://doi.org/10.1002/per.19....
5.
Kaźmierczak M, Michałek-Kwiecień J, Kiełbratowska B, et al. Parents’ personality and maternal experiencesin childcare as predictors of postpartum depressionin couples in transition to parenthood. Psychiatr Pol. 2020; 54(5): 991–1005. https://doi.org/10.12740/PP/On....
6.
Hechler CC, Beijers RR, Riksen-Walraven JM, et al. Are cortisol concentrations in human breast milk associated with infant crying? Dev Psychobiol. 2018; 60(6): 639−650. https://doi.org/10.1002/dev.21....
7.
Hinde K. Lactational programming of infant behavioral phenotype. In: Clancy KBH, Hinde K, Rutherford’s JN, et al. re. Primate development in proximate and ultimate perspective. New York: Springer Science & Business Media; 2013. p. 187–207.
8.
Grey KR, Davis EP, Sandman CA, et al. Human milk cortisol is associated with infant temperament. Psychoneuroendocrinology, 2012; 38(7): 1178−1185. https://doi.org/10.1016/j.psyn....
9.
Nolvi S, Uusitupa HM, Bridgett DJ, et al. Human milk cortisol concentration predicts experimentally induced infant fear reactivity: moderation by infant sex. Dev Sci. 2018; 21(4): e12625. http://dx.doi.org/10.1111/desc....
10.
Vancamelbeke M, Vermeire S, The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017; 11(9): 821–834. https://doi.org/10.1080/174741....
11.
Glynn LM, Davis EP, Schetter CD, et al. Postnatal maternal cortisol levels predict temperament in healthy breastfed infants. Early Hum Dev. 2007; 83(10): 675−681. https://doi.org/10.1016/j.earl....
12.
Aparicio M, Browne PD, Hechler C, et al. Human milk cortisol and immune factors over the first three postnatal months: Relations to maternal psychosocial distress. PloS One. 2020; 15(5): e0233554. https://doi.org/10.1371/journa....
13.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry, 1987; 150: 782–786.
14.
Khanlari S, Barnett AB, Ogbo FA, et al. Re-examination of perinatal mental health policy frameworks for women signalling distress on the Edinburgh Postnatal Depression Scale (EPDS) completed during their antenatal booking-in consultation: a call for population health intervention. BMC Pregnancy Childbirth. 2019; 19(1): 221. https://doi.org/10.1186/s12884....
15.
Smith-Nielsen J, Matthey S, Lange T, et al. Validation of the Edinburgh Postnatal Depression Scale against both DSM-5 and ICD-10 diagnostic criteria for depression. BMC Psychiatry 2018; 18 (1): 393. https://doi.org/10.1186/s12888....
16.
Priyambada LK, Bakhla AK, Pattojoshi A. Factor structure and internal consistency of Oriya version of Edinburgh Postnatal Depression Scale. Indian J Psychiatry. 2020; 62(3): 312–315. https://doi.org/10.4103/psychi....
17.
Dominiak M, Antosik-Wojcinska AZ, Baron M, et al. Recommendations for the prevention and treatment of postpartum depression. Ginekol Pol. 2021; 92(2): 153–164. https://doi.org/10.5603/GP.a20....
18.
Seth S, Lewis AJ, Galbally M. Perinatal maternal depression and cortisol function in pregnancy and the postpartum period: a systematic literature review. BMC Pregnancy Childbirth. 2016; 16: 124. https://doi.org/10.1186/s12884....
19.
Osnes RO, Eberhard-Gran M, Follestad T, et al. Mid-Pregnancy Insomnia and its Association with Perinatal Depressive Symptoms: A Prospective Cohort Study. Behav. Sleep Med. 2021; 19(3): 285–302. https://doi.org/10.1080/154020....
20.
O’Keane V, Lightman S, Patrick K, et al. Changes in the maternal hypothalamic-pituitary-adrenal axis during the early puerperium may be related to the postpartum ‘blues’. J. Neuroendocrinol. 2011; 23(11): 1149–1155. https://doi.org/10.1111/j.1365....
21.
Yahya NFZ, Teng NIMF, Das S, et al. Postpartum depression among Neonatal Intensive Care Unit mothers and its relation to postpartum dietary intake: A review. J Neonatal Nurs. 2021; 27(4): 229–237. https://doi.org/10.1016/j.jnn.....
22.
Çekin B, Turan T. The Stress Levels of Parents of Premature Infants and Related Factors in Nenoatal Intensive Care Units. Turk J Pediatr. 2018; 60(2): 117–125. https://doi.org/10.24953/turkj....
23.
Golec M, Rajewska-Rager A, Latos K, et al. The assessment of postpartum mood disorders and its risk factors. Psychiatria. 2016; 13(1): 1−7.
24.
Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Metaanalysis, and Meta-Regression of 291 Studies from 56 Countries. Front Psychiatry. 2017; 8: 248. https://doi.org/10.3389/fpsyt.....
25.
Arifin SRM, Cheyne H, Maxwell M. Review of the prevalence of postnatal depression across cultures. AIMS Public Health. 2018; 5(3): 260–295. https://doi.org/10.3934/public....
26.
Bradshaw H, Riddle JN, Salimgaraev R, et al. Risk factors associated with postpartum depressive symptoms: A multinational study. J Affect Disord. 2022, 301: 345–351. https://doi.org/10.1016/j.jad.....
27.
Khalifa DS, Glavin K, Bjertness E, et al. Postnatal depression among Sudanese women: prevalence and validation of the Edinburgh postnatal depression scale at 3 months postpartum. Int. J. Women’s Health. 2015; 7: 677–684. https://doi.org/10.2147/IJWH.S....
28.
Arikan I, Korkut Y, Demir BK, et al. The prevalence of postpartum depression and associated factors: a hospital-based descriptive study. J Clin Anal Med. 2017; 8(4): 300–305. https://doi.org/10.4328/jcam.5....
29.
Norhayati MN, Hazlina NH, Asrenee AR, et al. Magnitude and risk factors for postpartum symptoms: a literature review. J Affect Disord. 2015; 175: 34−52. https://doi.org/10.1016/j.jad.....
30.
Kossakowska K. Symptoms of postpartum depression and breastfeeding self-efficacy. Polish Journal of Paediatrics. 2018; 93(2): 107–116.https://doi.org/10.5114/polp.2....
31.
Kaźmierczak M, Przykłota M, Gierszewska M, et al. Multivariate analysis of risk factors for postpartum depression. Med Og Nauk Zdr. 2020; 26(2): 139–145. https://doi.org/10.26444/monz/....
32.
Ghaedrahmati M, Kazemi A, Kheirabadi G, et al. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017; 6: 60. https://doi.org/10.4103/jehp.j....
33.
Gerhant A, Olajossy M, Kalińska A, et al. Stolen motherhood-case study of postpartum depression. Curr Probl Psychiatry. 2016; 17(3): 149−163. https://doi.org/10.1515/cpp-20....
34.
Dettmer AM, Murphy AM, Guitarra D, et al. Cortisol in neonatal mother’s milk predicts later infant social and cognitive functioning in rhesus monkeys. Child Dev. 2017; 89(2): 525–538. https://doi.org/10.1111/cdev.1....
35.
Shukri MNH, Wells J, Eaton S, et al. Randomized controlled trial investigating the effects of a breastfeeding relaxation intervention on maternal psychological state, breast milk outcomes, and infant behavior and growth. Am J Clin Nutr. 2019; 110(1): 121–130. https://doi.org/10.1093/ajcn/n....
36.
Romijn M, van Tilburg L, Hollanders JJ, et al. The Association between Maternal Stress and Glucocorticoid Rhythmicity in Human Milk. Nutrients. 2021; 13(5): 1608. https://doi.org/10.3390/nu1305....
37.
Seth S, Lewis AJ, Galbally M. Perinatal maternal depression and cortisol function in pregnancy and the postpartum period: a systematic literature review. BMC Pregnancy Childbirth. 2016; 16(1): 124. https://doi.org/10.1186/s12884....
38.
Groër MW, Morgan K. Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology. 2007; 32(2): 133−139. https://doi.org/10.1016/j.psyn....
39.
Taylor A, Glover V, Marks M, et al. Diurnal pattern of cortisol output in postnatal depression. Psychoneuroendocrinology. 2009; 34(8): 1184−1188. https://doi.org/10.1016/j.psyn....
40.
Nierop A, Bratsikas A, Zimmermann R, et al. Are Stress-Induced Cortisol Changes During Pregnancy Associated With Postpartum Depressive Symptoms? Psychosom Med. 2006; 68(6): 931−937. https://doi.org/10.1097/01.psy....
41.
Yu Y, Liang HF, Chen J, et al. Postpartum Depression: Current Status and Possible Identification Using Biomarkers. Front. Psychiatry. 2021; 12: 620371. https://doi.org/10.3389/fpsyt.....
42.
Gillespie SL, Mitchell AM, Kowalsky JM, et al. Maternal parity and perinatal cortisol adaptation: The role of pregnancy-specific distress and implications for postpartum mood. Psychoneuroendocrinol. 2018; 97: 86–93. https://doi.org/10.1016/j.psyn....
43.
Lee HJ, Rubio MR, Elo IT, et al. Factors associated with intention to breastfeed among low-income, inner-city pregnant women. Matern Child Health J. 2005; 9(3): 253–261. https://doi.org/10.1007/s10995....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.