RESEARCH PAPER
Analysis of women's knowledge about postpartum mental disorders – a pilot study
1
Śląski Uniwersytet Medyczny, Katowice, Polska
2
Zakład Biochemii i Genetyki Medycznej, Katedra Nauk Podstawowych, Wydział Nauk o Zdrowiu w Katowicach, Śląski Uniwersytet Medyczny, Katowice, Polska
Corresponding author
Joanna Iwanicka
Zakład Biochemii i Genetyki Medycznej, Katedra Nauk Podstawowych, Wydział Nauk o Zdrowiu w Katowicach, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 18, 40-752 Katowice, Polska, ul. Medyków 18, 40-752, Katowice, Polska
Zakład Biochemii i Genetyki Medycznej, Katedra Nauk Podstawowych, Wydział Nauk o Zdrowiu w Katowicach, Śląski Uniwersytet Medyczny w Katowicach, ul. Medyków 18, 40-752 Katowice, Polska, ul. Medyków 18, 40-752, Katowice, Polska
Med Og Nauk Zdr. 2024;30(2):153-160
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The World Health Organization (WHO) reports that globally, approximately 10% of pregnant women and 13% of women in the postpartum period experience mental disorders. The aim of this study was to investigate the level of women›s knowledge regarding mental disorders occurring in the postpartum period.
Material and methods:
The survey included a group of 350 women aged 17–66, and was conducted using an authorconstructed questionnaire. The results were analyzed using the software STATISTICA 13.0 and the OpenEpi website.
Results:
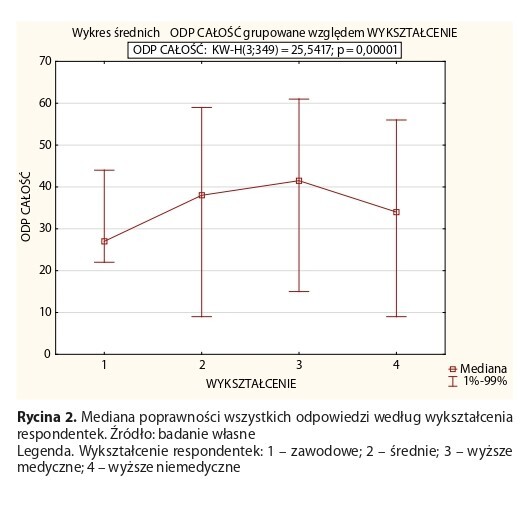
The women's knowledge about postpartum mental disorders can be described as low; the respondents achieved the mean score 36.8 per 79 scores possible (46.6%). The respondents displayed the lowest knowledge in the area of diagnosis and therapeutic procedures, obtaining 6.9 scores on average, which represented only 28.8% of the correct answers. Almost unanimously (92.30%) the surveyed women confirmed a lack of awareness of organizations working for individuals struggling with the discussed mental health issue. At the same time, women with medical education and those professionally associated with the medical field demonstrated greater knowledge concerning postpartum mental disorders, compared to other respondents.
Conclusions:
Women’s knowledge concerning postpartum mental disorders in Poland is low. Respondents with medical education are characterized by a higher degree of substantive correctness than other respondents. In addition, the lack of respondents’ knowledge was observed regarding organizations and associations which provide support to women and their families in challenging perinatal situations. It is also crucial to further disseminate information about the discussed disorders among the general population.
The World Health Organization (WHO) reports that globally, approximately 10% of pregnant women and 13% of women in the postpartum period experience mental disorders. The aim of this study was to investigate the level of women›s knowledge regarding mental disorders occurring in the postpartum period.
Material and methods:
The survey included a group of 350 women aged 17–66, and was conducted using an authorconstructed questionnaire. The results were analyzed using the software STATISTICA 13.0 and the OpenEpi website.
Results:
The women's knowledge about postpartum mental disorders can be described as low; the respondents achieved the mean score 36.8 per 79 scores possible (46.6%). The respondents displayed the lowest knowledge in the area of diagnosis and therapeutic procedures, obtaining 6.9 scores on average, which represented only 28.8% of the correct answers. Almost unanimously (92.30%) the surveyed women confirmed a lack of awareness of organizations working for individuals struggling with the discussed mental health issue. At the same time, women with medical education and those professionally associated with the medical field demonstrated greater knowledge concerning postpartum mental disorders, compared to other respondents.
Conclusions:
Women’s knowledge concerning postpartum mental disorders in Poland is low. Respondents with medical education are characterized by a higher degree of substantive correctness than other respondents. In addition, the lack of respondents’ knowledge was observed regarding organizations and associations which provide support to women and their families in challenging perinatal situations. It is also crucial to further disseminate information about the discussed disorders among the general population.
REFERENCES (34)
1.
Wilczek-Rużyczka E, Kwak M. Zdrowie psychiczne. Współczesne zagrożenia i możliwości wzmocnienia. 1st ed. Warszawa: PZWL; 2022. p. 11.
2.
Trawkowska D, Frąckowiak-Sochańska M, Zespół Obserwatorium Integracji Społecznej w Poznaniu w składzie: Czub K, et al. System wsparcia osób z zaburzeniami psychicznymi. W obszarze zdrowia na podstawie Diagnozy systemu wsparcia osób z zaburzeniami psychicznymi na terenie województwa wielkopolskiego. Poznań: Obserwatorium Integracji Społecznej; Oct 2017. p. 4–5.
3.
World Health Organization. World mental health report. Transforming mental health for all. Geneva 2022. https://www.who.int/publicatio... (access: 2023.01.29).
4.
Janik I, Maciejewska M, Fabian Danielewska A, et al. Emotional disorders in the perinatal period. Journal of Education, Health and Sport. 2018;8(9):983 989. http://dx.doi.org/10.5281/zeno....
5.
Sosnowska M. Doświadczenia z warsztatu o depresji okołoporodowej- zmiana tożsamości kobiety po porodzie i odkrywanie nowego „ja”. Psychiatry. 2019;16,3:139–145.
6.
Fleischman EK, Connelly CD, Calero P. Depression and Anxiety, Stigma, and Social Support Among Women in the Postpartum Period. Nurs Womens Health. 2022;26(2):95–106. https://doi.org/10.1016/j.nwh.....
7.
Balaram K, Marwaha R. Postpartum Blues. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023. PMID: 32119433.
8.
Huang W, Li G, Wang D, et al. Postpartum depression literacy in Chinese perinatal women: a cross-sectional study. Front Psychiatry. 2023;14:1117332. https://doi.org/10.3389/fpsyt.....
9.
Hidalgo-Padilla L, Toyama M, Zafra-Tanaka JH, et al. Association between maternity leave policies and postpartum depression: a systematic review. Arch Womens Ment Health. 2023;26(5):571–580. https://doi.org/10.1007/s00737....
10.
Agencja Oceny Technologii Medycznych i Taryfikacji. Rekomendacja nr 13/2020 z dnia 30 listopada 2020 r. Prezesa Agencji Oceny Technologii Medycznych i Taryfikacji w sprawie zalecanych technologii medycznych, działań przeprowadzanych w ramach programów polityki zdrowotnej oraz warunków realizacji tych programów, dotyczących problemu zdrowotnego depresji poporodowej. https://bipold.aotm. gov.pl/assets/files/ppz/2020/REK/13_2020.pdf (access: 2023.02.06).
11.
Serwis Ministerstwa Zdrowia i Narodowego Funduszu Zdrowia. Pacjent. gov.pl. https://pacjent.gov.pl/jak-zyc... matka-w-depresji (access: 2023.02.06).
12.
Silva BPD, Matijasevich A, Malta MB, et al. Common mental disorders in pregnancy and postnatal depressive symptoms in the MINA-Brazil study: occurrence and associated factors. Rev Saude Publica. 2022;56:83. https://doi.org/10.11606/s1518....
13.
Zaręba K, Banasiewicz J, Rozenek H, et al. Peripartum Predictors of the Risk of Postpartum Depressive Disorder: Results of a Case-Control Study. Int J Environ Res Public Health. 2020;17(23):8726. https://doi. org/10.3390/ijerph17238726.
14.
Cena L, Mirabella F, Palumbo G, et al. Prevalence of maternal antenatal anxiety and its association with demographic and socioeconomic factors: A multicentre study in Italy. Eur Psychiatry. 2020;63(1):e84. https://doi.org/10.1192/j.eurp....
15.
Grisbrook MA, Dewey D, Cuthbert C, et al. Associations among Caesarean Section Birth, Post-Traumatic Stress, and Postpartum Depression Symptoms. Int J Environ Res Public Health. 2022;19(8):4900. https:// doi.org/10.3390/ijerph19084900.
16.
Ahmadpour P, Faroughi F, Mirghafourvand M. The relationship of childbirth experience with postpartum depression and anxiety: a cross-sectional study. BMC Psychol. 2023;11(1):58. https://doi.org/10.1186/ s40359-023-01105-6.
17.
Walker AL, de Rooij SR, Dimitrova MV, et al. Psychosocial and peripartum determinants of postpartum depression: Findings from a prospective population-based cohort. The ABCD study. Compr Psychiatry. 2021;108:152239. https://doi.org/10.1016/j.comp....
18.
Hamel C, Lang E, Morissette K, et al. Screening for depression in women during pregnancy or the first year postpartum and in the general adult population: a protocol for two systematic reviews to update a guideline of the Canadian Task Force on Preventive Health Care. Syst Rev. 2019;8(1):27. https://doi.org/10.1186/s13643....
19.
Van Niel MS, Payne JL. Perinatal depression: A review. Cleve Clin J Med. 2020;87(5):273–277. https://doi.org/10.3949/ccjm.8....
20.
Stewart AL, Payne JL. Perinatal Depression: A Review and an Update. Psychiatr Clin North Am. 2023;46(3):447–461. https://doi.org/10.1016/j. psc.2023.04.003.
21.
Niegowska KW, Kobos E. Ocena częstotliwości występowania depresji poporodowej u kobiet w pierwszym tygodniu połogu. Med Og Nauk Zdr. 2019;25(4):251–257. https://doi.org/10.26444/monz/....
22.
Suchowiak S, Wszołek K, Suwalska J, et al. Badania przesiewowe w kierunku depresji okresu okołoporodowego: przegląd narzędzi i barier w skriningu. Neuropsychiatria i Neuropsychologia. 2020;15,1–2:60–69. https://doi.org/10.5114/nan.20....
23.
Dziennik Ustaw Rzeczypospolitej Polskiej. Rozporządzenie Ministra Zdrowia w sprawie standardu organizacyjnego opieki okołoporodowej z dnia 16 sierpnia 2018 roku. Poz. 1756. Warszawa, dnia 11 września 2018 roku. https://isap.sejm.gov.pl/isap.... WDU20180001756/O/D20181756.pdf (access: 2023.03.30).
24.
Koszewska Iwona. O depresji w ciąży i po porodzie. Warszawa: PZWL Wydawnictwo Lekarskie; 2010. p. 152. ISBN 978-83-200-6079-9. p.91–131.
25.
Lim G. Perinatal depression. Curr Opin Anaesthesiol. 2021;34(3):233– 237. https://doi.org/10.1097/ACO.00....
26.
Pacheco F, Guiomar R, Brunoni AR, et al. Efficacy of non-invasive brain stimulation in decreasing depression symptoms during the peripartum period: A systematic review. J Psychiatr Res. 2021;140:443–460. https:// doi.org/10.1016/j.jpsychires.2021.06.005.
27.
Friedman SH, Reed E, Ross NE. Postpartum Psychosis. Curr Psychiatry Rep. 2023;25(2):65–72. https://doi.org/10.1007/s11920....
28.
Grussu P, Jorizzo GJ, Alderdice F, et al. Preventing, Mitigating, and Treating Women‘s Perinatal Mental Health Problems during the COVID-19 Pandemic: A Scoping Review of Reviews with a Qualitative Narrative Synthesis. Behav Sci (Basel). 2023;13(5):358. https://doi.org/10.3390/bs1305....
29.
Branquinho M, Shakeel N, Horsch A, et al. Frontline health professionals› perinatal depression literacy: A systematic review. Midwifery. 2022;111:103365. https://doi.org/10.1016/j.midw....
30.
Al Hadi A, Paliwoda M, Dawson J, et al. Women's Utilisation, Experiences and Satisfaction with Postnatal Follow-up Care: Systematic literature review. Sultan Qaboos Univ Med J. 2022;22(4):455–471. https://doi. org/10.18295/squmj.10.2022.059.
31.
Rai S, Pathak A, Sharma I. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry. 2015;57(Suppl 2): S216–21. https://doi.org/10.4103/0019-5....
32.
Dominiak M, Antosik-Wojcinska AZ, Baron M, et al. Recommendations for the prevention and treatment of postpartum depression. Ginekol Pol. 2021;92(2):153–164. https://doi.org/10.5603/GP.a20....
33.
Ponzini GT, Snider MDH, Evey KJ, et al. Women's Knowledge of Postpartum Anxiety Disorders, Depression, and Cognitive Behavioral Therapy. J Nerv Ment Dis. 2021;209(6):426–433. https://doi.org/10.1097/ NMD.0000000000001315.
34.
Wang K, Li R, Li Q, et al. Knowledge, attitude, and practice toward postpartum depression among the pregnant and lying-in women. BMC Pregnancy Childbirth. 2023;23(1):762. https://doi.org/10.1186/s12884- 023-06081-8.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.